Honestly speaking, tracking and managing any autoimmune diseases is no easy task. It is a lot easy said than done. Quite frankly, life gets busy, and on top of it all, dealing with the disease itself and all of its associated symptoms. Trying to manage medications and other treatment options. It is hard.
Fortunately, you are not alone! This article will talk about tracking and managing autoimmune diseases…all located in one convenient place. Also, tracking and managing have never become simpler! It is a perfect way to live peacefully with the autoimmune disease as well as to take the necessary steps to excel! For your health, for your mental sake, for your physical sake, for your loved ones, and for the betterment of your quality of life! Let’s start living![1]
Autoimmune Diseases
What are Autoimmune Diseases?
Ultimately, the immune system exists to fight off foreign substances and tumor cells that enter the body (6). Basically, it behaves like the police and once it catches the “bad cells”, it seeks them out and destroys it. The human body is quite fascinating.
However, in some cases for unknown reasons, the immune system may begin producing antibodies that attack the body’s own tissues (instead of fighting other real infections)(8). Simply put, it is confused about which cells to attack. Despite not knowing the reason why an immune system behaves this way, there are studies investigating the triggers. Some studies suggest that genetics, environment, and certain infections could possibly explain this phenomenon (6).
Who Is At Risk?
One thing is for sure: Women are at a higher risk of developing an autoimmune disease than their male counterparts. A young, postpubescent woman is ten times more likely. Some studies believe that is due to higher levels of estrogen as this hormone can alter the immune response.[2][3]
Specific Autoimmune Diseases
Rheumatoid Arthritis (RA)
RA Overview
The immune system produces antibodies that will attach to the linings of joints. In conclusion, the immune system cells will then attack the joints, causing inflammation, swelling, and pain (8). It will typically start in small peripheral joints and is often symmetric. However, it will progress to involve proximal joints if left untreated. Over time, this joint inflammation leads to the destruction of the joint with cartilage and bone erosion (1).
For instance, the Diary function** (illustrated on the left) is one of the functions located in the CareClinic platform! By using this, using your own words, a diary log can be kept regarding the autoimmune disease that is affecting your life.
This will be a convenient way to store all your thoughts; readily accessible for future days if you ever need to recall (for yourself or your healthcare team). Do not struggle alone- sometimes, getting the words out (how you felt that day, how you are coping) are all healthy ways to learn to deal and cope with your disorder.
**Please note that all of these functions that are mentioned here (and below) are applicable to ALL diseases that will be discussed in this article.
Etiology
The etiology of RA is still unknown. However, it is thought to result from the interaction between the patients’ genotype and environment (1).
Epidemiology
The worldwide prevalence of RA is about 0.24%. The annual incidence (new cases per year) of RA in the United States and other western nations of northern Europe is about 40 per 100,000 persons (1).
Risk Factors
Some risk factors include (but are not limited to):
- For instance, cigarette smoking (Number one risk factor) (1)
- For example, diet (the traditional ‘western’ diet that is high in caloric content, and low in fiber increases the risk of RA. It has been shown that consumption of long-chain omega-3 polyunsaturated fatty acids can be at risk of RA) (1)
- Obesity (30% increase in the risk of RA for patients with a body mass index (BMI) of greater than 30 kg/m^2 and a 15% increased risk for those with a BMI of 25 to 29.9 kg/m^2) (1)
- Mucosal injury from occupational exposures and environmental pollutants (1)
Symptoms/Physical Exam

The most common and predominant symptoms include joint pain and stiffness, especially morning stiffness and joint swelling (illustrated in the picture on the right). Although multiple small joint involvements are a frequent feature, some patients may present with monoarticular and extraarticular involvement.
On physical examination, the affected joint will be painful if pressure is applied or on movement. Furthermore, synovial thickening with a “boggy” feel on palpation will be noted. If there are multiple joint involvements, reduced grip strength will be seen in physical testing. The classical physical findings of ulnar deviation, metacarpophalangeal joint subluxation, ulnar deviation, swan neck deformity, Boutonniere deformity, and the “bowstring” sign are seen in advanced chronic RA.
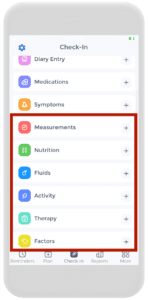
In addition, rheumatoid nodules are the most common cutaneous manifestations of RA. By using the CareClinic platform and the symptom tracker function, tracking RA symptoms (or other autoimmune disease symptoms) has never been easier.
Clinical Evaluation
Some testings needed to diagnose may involve:
- Blood work (usually reveals anemia of chronic disease, thrombocytosis, and neutropenia may be present if Felty syndrome is present) (1)
- Serology (About 75% to 85% of patients with RA will test positive for rheumatoid factor (RF), ACPA, or both) (1)
- Acute phase reactants (erythrocyte sedimentation rate (ESR) and levels of C-reactive protein (CRP), are usually elevated in patients with active disease and should be obtained) (1)
- Synovial fluid examination (usually reveals a leukocyte count between 1500 to 25,000/cubic mm and is predominantly polymorphonuclear cells) (1)
- Imaging (With advanced disease, joint involvement on Xrays will reveal periarticular osteopenia, joint space narrowing, and bony erosions. For earlier, MRI or ultrasounds may be useful) (1)
Treatment/Management

Other treatment options: Nonbiologic DMARDs, TNF inhibitors, Rituximab, Abatacept, Interleukin 6 Inhibitors, and Janus kinase (JAK) Inhibitors (1). Which medication is appropriate will be a discussion to have with the healthcare team.
Management of medications using the CareClinic platform can be easy as 1-2-3. By using the medication tracker function, simply input the medication name(s) and dosage and even get refill reminders! Never miss another dose again!
Prognosis
However, it is important to educate patients on using support groups, and exercising programs to improve joint functions, maintaining healthy body weight, quitting smoking, etc. A comprehensive interprofessional team can provide a multi-faceted approach to the treatment of RA and improve patient outcomes.
This can be all recorded conveniently on the CareClinic Platform using the first check-in page. Tracking and managing your autoimmune disease will be simpler than before. Begin your journey to the best version of you today!
Inflammatory Bowel Disease (IBD)
IBD Overview
Inflammatory bowel disease (IBD) is characterized by “repetitive episodes of inflammation of the gastrointestinal tract caused by an abnormal immune response to gut microflora”. Following categories:
- Ulcerative Colitis (UC)- involves diffuse inflammation of the colonic mucosa (2)
- Crohn’s Disease- transmural ulceration of any portion of the gastrointestinal tract (GI) most often affecting the terminal ileum and colon (2)
Etiology
IBD is found to occur in genetically susceptible individuals however, the true cause is unknown (2).
Epidemiology
The North American incidence of IBD ranges from 2.2 to 19.2 cases per 100,000 person-years for ulcerative colitis and 3.1 to 20.2 cases per 200,000 person-years for CD (2).
Risk Factors
Some risk factors are (but not limited to):
- For instance, smoking (high risk with Crohn’s) (2)
- For example, living in developed countries (2)
- Living in colder climates (2)
- Diet (is debatable)
Patients with IBD also have a higher risk of colorectal cancer (2).
Symptoms
Ulcerative colitis: bloody diarrhea with or without mucus. Patients commonly describe “tenesmus, a sensation of incomplete evacuation, and abdominal pain. The physical exam may reveal predominantly left lower or left upper quadrant abdominal pain. Signs of an acute abdomen including guarding, rebound tenderness, or percussion tenderness warrant investigation for toxic megacolon”(2). Some will experience skin changes as well.
Crohn’s disease: vary considerably depending on the region of gastrointestinal involvement. “The symptom complex of right lower quadrant pain, weight loss, and non-bloody diarrhea are suggestive of Crohn’s disease flare-up. Fistula formation may result in fecaluria, pneumaturia, and rectovaginal fistulas. Masses in the right lower quadrant suggest an abscess (2).”
Clinical Evaluation
IBD may require:
- For instance, clinical findings (2)
- For example, Inflammatory laboratory markers (2)
- Imaging findings (2)
- Endoscopic biopsies (2)
- Hematologic findings (2)
- Fecal calprotectin levels (2)
- Abdominal x-ray (2)
- Barium studies (2)
- Ultrasounds (2)
- Endoscopic evaluation (2)
Treatment/Management
The goal of treatment is to induce remission for either UC or CD. Treatment of IBD depends on the severity of the disease, usually in a step-wise fashion. Firstly, it will start with aminosalicylates. Finally, the immune-modifying agents (e.g Anti-TNF agents) are the step three drugs (2). Speak to your physician regarding what treatment is right for you.
Prognosis
Patients with IBD will need lifelong follow-up for their disease. However, on the bright side, there are many management tips, implementing food diaries, seeking support groups, etc., to help you not feel so alone and improve your quality of life!
Multiple Sclerosis (MS)
MS Overview
MS is a chronic autoimmune disease of the central nervous system (CNS) through it’s inflammation, demyelination, gliosis, and neuronal loss (7).
Etiology
The exact etiology of MS is unknown. However, factors in its pathogenesis are put into three categories:
-
Immune factors (7)
-
Environmental factors (7)
-
Genetic associations (7)
Epidemiology
Approximately 400,000 individuals in the United States and 2.5 million individuals worldwide have multiple sclerosis. The disease is three-fold more common in females than in males (7).
Symptoms
Typical clinical symptoms noted on verbal history include:
-
For instance, vision symptom: includes vision loss(either monocular or homonymous), double vision, and symptoms relating to optic neuritis (7)
-
For example, Vestibular symptoms: vertigo, gait imbalance (7)
-
Bulbar dysfunction: dysarthria, dysphagia (7)
-
Motor: weakness, tremor, spasticity, fatigue (7)
-
Sensory: loss of sensation, paresthesias, dysesthesias (7)
-
For instance, Urinary and bowel symptoms: incontinence, retention, urgency, constipation, diarrhea, reflux (7)
-
Cognitive symptoms: memory impairment, impairment of executive functions, trouble concentrating (7)
-
Psychiatric symptoms: depression, anxiety (7)
The physical exam will include:
-
For instance, evaluation for optic neuritis, classically manifesting as subacute monocular central vision loss; pain in eye movement (7)
-
Difficulty with adducting in lateral gaze suggests internuclear ophthalmoplegia (INO) (7)
-
Nystagmus (7)
-
For example, Diplopia (7)
-
For instance, Hearing loss (7)
-
Facial pain (7)
-
For instance, Partial transverse myelitis is typically unilateral or bilateral and characterized by sensory disturbances (7)
-
Brainstem symptoms classically involve diplopia, dysphagia, dysarthria, and ataxia (7)
-
L’hermittes sign; is known as a shock-like sensation that occurs with neck flexion (7)
-
Hyperreflexia (7)
-
Tremor (7)
-
Muscle spasms (7)
-
Fatigue/Weakness (7)
-
Erectile dysfunction (7)
Clinical Evaluation
Diagnosis occurs by reviewing the history and physical, MRI, evoked potentials, and CSF/blood studies and excluding other causes of the patient’s symptoms.
Treatment/Management
Disease-modifying therapies are often the mainstay of treatment of relapsing-remitting MS such as Glatiramer acetate, dimethyl fumarate, fingolimod, interferon-beta preparations, natalizumab, and mitoxantrone (7). Speak to your doctor today about which one is the best for you.
Prognosis
Multiple sclerosis is a complex disease process and therefore, needs a multifaceted approach to help the patient (7). Not only is a healthcare team recommended, but other support groups and reaching out is also recommended.
Diabetes Mellitus – Type 1 (T1DM)
T1DM Overview
Diabetes mellitus (DM) is a metabolic disease involving inappropriately elevated blood glucose levels. T1DM classically is a result of defective insulin secretion (5).
Etiology
T1DM is “known as the destruction of beta cells in the pancreas, typically secondary to an autoimmune process. The result is the absolute destruction of beta cells; consequentially, insulin is absent or extremely low (5)“.
Epidemiology
Globally, 1 in 11 adults has DM (ten% has T1DM). The onset of T1DM gradually increases from birth and peaks at ages 4 to 6 years and then again from 10 to 14 years. While most autoimmune diseases are more common in females, there are actually no apparent gender differences in the incidence of childhood T1DM. Furthermore, the incidence of T1DM has been increasing worldwide (5).
Symptoms
Symptoms include:
- For example, polyuria (5)
- Polydipsia (5)
- For instance, Weight loss (5)
- Poor skin turgor (from dehydration) (5)
- For example, fruity odor coming from the breath (in people with diabetic ketoacidosis) (5)
- Eye exam: may show hemorrhages or exudates on the macula (5)
Clinical Evaluation
During patient history, questions about family history, autoimmune diseases, and insulin-resistant are critical to making the diagnosis of DM. However, other evaluations are:
- Elevated serum glucose levels (fasting glucose greater than 126 mg/dL, random glucose over 200 mg/dL, or hemoglobin A1C (HbA1c exceeding 6.5%) (5)
- With or without antibodies to glutamic acid decarboxylase (GAD) and insulin (5)
Treatment/Management
For instance, the treatment and management of diabetes are complex and require a multitude of interventions in order to be truly successful long-term. Diabetic education and patient engagement are critical in management. Patients have better outcomes if they can manage their diet (carbohydrate and overall caloric restriction), exercise regularly (more than 150 minutes weekly), and independently monitor glucose (5).
Prognosis
The prognosis of DM is significantly influenced by the degree of glucose management (5).
Psoriasis
Overview
Psoriasis is a “chronic proliferative and inflammatory condition of the skin. Therefore, it is characterized by erythematous plaques covered with silvery scales, particularly over the extensor surfaces, scalp, and lumbosacral region (4)“.
Etiology
The exact etiology is unknown, but it is known to be an autoimmune disease aggravated by T lymphocytes (4).
Epidemiology
Psoriasis has a prevalence ranging from 0.2% to 4.8%. In the United States, about 2% of the population is hit, yet interestingly, higher rates of psoriasis are in the Faroe Islands. On the other hand, the prevalence of psoriasis is low in Japan and may be absent in Aboriginal Australians and Indians from South America (4).
Symptoms
Psoriasis presents as well-defined erythematous plaques covered with silvery scales commonly over the scalp, extensors of extremities, particularly over knees and elbows, and lumbosacral regions (4).
There are also different types of psoriasis that will also show different symptoms. The one that is known as plaque psoriasis (the most common). Other ones are:
- For instance, guttate psoriasis (4)
- For example, Pustular psoriasis (4)
- Erythrodermic psoriasis (4)
- For example, Inverse psoriasis (4)
- Psoriatic arthritis (4) – Learn more about arthritis flare ups here.
Clinical Evaluation
Usually, diagnosis is made by clinical observation and site of lesions; other laboratory studies can be brought forward (4).
Treatment/Management
- For example, topical therapy (4)
- For instance, Phototherapy (4)
- Systemic drugs (4)
- Steroids (4)
Discuss which medication or treatment option is right for you.
Prognosis
Psoriasis is a chronic condition that is known to have a negative impact on the quality of life in patients. Its management is very complex and usually requires a team of professionals dedicated to this disease (4).
Hashimoto’s Thyroiditis
Hashimoto’s Thyroiditis Overview
Hashimoto’s thyroiditis is an autoimmune disease that destroys thyroid cells. It is the most common cause of hypothyroidism in developed countries (3).
Etiology
The etiology of Hashimoto’s disease is not understood, “most patients develop antibodies to a variety of thyroid antigens, the most common of which is anti-thyroid peroxidase (anti-TPO). Many also form antithyroglobulin (anti-Tg) and TSH receptor-blocking antibodies (TBII). Therefore, these antibodies attack the thyroid tissue, eventually leading to inadequate production of thyroid hormone (3).”
Epidemiology
After age six, Hashimoto’s is the most common cause of hypothyroidism in the United States and in those areas of the world where iodine intake is adequate. The incidence is at estimated at 0.8 per 1000 per year in men and 3.5 per 1000 per year in women (3).
Symptoms
- For example, Myxedema (an edema-like skin condition) (3)
- For instance, dry, coarse, brittle hair (3)
- Fatigue, exertional dyspnea, and exercise intolerance (3)
- Weight gain (3)
- Cold intolerance (3)
- Decreased sweating (3)
- For instance, nerve deafness (3)
- Peripheral neuropathy (3)
- Decreased energy (3)
- For example, depression (3)
- For example, Dementia (3)
- Memory loss (3)
- Muscle cramps (3)
- Joint pain (3)
- Menorrhagia (3)
-
Bradycardia (3)
-
The delayed relaxation phase of tendon reflexes (3)
-
For instance, Elevated blood pressure (3)
-
Slow speech (3)
-
Ataxia (3)
-
Macroglossia (3)
Clinical Evaluation
- For example, increased TSH levels (3)
- Low total T4 or free T4 level (3)
- Presence of anti-thyroid peroxidase and anti-thyroglobulin antibodies (3)
- For instance, Anemia (3)
- Creatine kinase, prolactin, cholesterol levels (3)
- For example, Thyroid ultrasound (3)
Treatment/Management
The mainstay of treatment for hypothyroidism is thyroid hormone replacement. The drug of choice is titrated levothyroxine sodium administered orally (3).
Prognosis
Hashimoto’s thyroiditis is a lifelong disorder with no cure; therefore, it is best managed with a multifaceted approach and team (3). Even for pregnant patients. Speak to your healthcare team on how to better help you manage your Hashimoto’s.
Other Autoimmune Diseases
- For example, Systemic lupus erythematosus (SLE) (8)
- For instance, Guillain-Barre syndrome (8)
- Chronic inflammatory demyelinating polyneuropathy (8)
- Graves Disease (8)
- For example, Myasthenia gravis (8)
- Scleroderma (8)
- Vasculitis (8)
- Thyrotoxicosis (6)
- Pernicious Anemia (6)
- For instance, autoimmune Atopic Gastritis (6)
- For example, Addison’s Disease (6)
- Goodpasture Syndrome (6)
- Autoimmune Hemolytic Anemia (6)
Using CareClinic for all your Tracking & Managing Needs
The CareClinic patient app can help make tracking and managing your autoimmune disease much simpler and easier. A place where you can write daily diary logs, and keep track of all your symptoms, medications, and external factors (diet, activity, therapy, etc)…in the palm of your hand. Start your journey today by downloading from your iOS or Android devices by clicking below.[10]
References
- “Patient Apps – Autoimmune Association”. https://autoimmune.org/resource-center/patient-support/patient-apps/
- “Lupus and other autoimmune diseases strike far more women than men. Now there's a clue why”. https://apnews.com/article/aff0e28dece3ef4168f301bd84331ea5
- “Autoimmune Disease: Does Sex Matter?”. https://www.hss.edu/conditions_autoimmune-disease-sex.asp
- “Rheumatoid arthritis: pathological mechanisms and modern pharmacologic therapies – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC5920070/
- “Environmental and gene-environment interactions and risk of rheumatoid arthritis – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC3402910/
- “Environment and Lifestyle: Their Influence on the Risk of RA – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC7601336/
- “Modifiable environmental exposure and risk of rheumatoid arthritis—current evidence from genetic studies – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC7310443/
- “Exposure to Traffic Pollution and Increased Risk of Rheumatoid Arthritis | Environmental Health Perspectives | Vol. 117, No. 7”. https://ehp.niehs.nih.gov/doi/10.1289/ehp.0800503
- “Rheumatoid arthritis”. https://en.wikipedia.org/wiki/Rheumatoid_arthritis
- “Tracker, Reminder – CareClinic on the App Store”. https://apps.apple.com/us/app/tracker-reminder-careclinic/id1455648231


