Before we can begin explaining skin rashes linked with Ulcerative Colitis. it is important to understand the foundation of Ulcerative Colitis. A review of the classification of Ulcerative Colitis will be discussed as well as examining the Ulcerative Colitis skin rash(es) that may present itself.
Also, a kind warning, there will be many more pictures in this article. So if medical-grade pictures aren’t your thing…the only recommendation would be to get your garbage bin ready beside you.
What is Ulcerative Colitis Skin Rash?
Inflammatory Bowel Disease (IBD)
IBD is an inflammation of the intestines (a part of your digestive system), there are spectra of diseases that may fall into this broad category, but the main two are Ulcerative Colitis and Crohn’s Disease (1).
It behaves as the main umbrella term, Although an exact etiology is unknown, it is internationally believed to be caused by the abnormal activation of the immune system and is genetic (even though there is no single gene to cause IBD) (1,2). However, Caucasians and individuals of eastern European Jewish descent are more likely to develop ulcerative colitis (3).
Crohn’s Disease
Since this article is about Ulcerative Colitis- let’s keep this part very brief. Crohn’s Disease affects any part of the digestive system: from the mouth to the anus, as non-continuous or “skip” lesions! Also, it affects the whole thickness (transmural) of the bowel wall (6).
Ulcerative Colitis
Ulcerative Colitis mainly affects the colon and rectum with continuous lesions and only affects the gut’s inner lining (mucosal and submucosal layers). The “Col” in Colitis refers to the colon, and “-itis” is defined as inflammation. Pretty cool, right?
Another interesting element is that the word “ulcerative” explains what is happening due to this inflammation. People with Ulcerative Colitis have inflammation caused by such ulcers that destroy the lining of the colon wall, leading to diarrhea and bleeding (other symptoms will have their section- so please be patient) (1, 6).
Irritable Bowel Syndrome (IBS) and Ulcerative Colitis
IBD and IBS get confused; however, understanding the difference is important- despite having many similarities. However, the cause of IBS is believed to be dysfunction of the nerves and muscles of the intestines.
There is no identifiable inflammation; nonetheless, the main symptoms of IBS are abdominal pain and diarrhea (same as IBS). But it is possible to have both IBS and IBD simultaneously. However, these distinctions must be made with careful discussion with your healthcare team (because treatment is possible.) (1,3).
What are the First Signs of Ulcerative Colitis Symptoms?
Ulcerative Colitis Review
The first signs can vary amongst individuals, mild to severe. In addition, patients with ulcerative colitis will often have relapses when inflammation and symptoms worsen ( called “flares”), followed by periods of remission.
This can last months to years when symptoms subside (3). Usually, people are more reluctant to seek help when they subside. However, recognizing certain symptoms may be helpful to someone struggling or perhaps seeing someone with these symptoms:
- Loose and urgent bowel movements (3)
- Frequent need to empty the bowels (3)
- Bloody stool (3)
- Abdominal cramps and pain (3)
- Persistent diarrhea accompanied by abdominal pain and blood, mucus, or pus in the stool (3)
- Ulcerative Colitis Skin Rash(es) (6)**
**can precede bowel disease or bowel exacerbation and should alert clinicians to evaluate the possibility of underlying IBD so early diagnosis and intervention with the appropriate therapy can be initiated. (6) Please see your physician if you notice any of these symptoms! It may be urgent.
Other Ulcerative Colitis Symptoms
- Rectal Bleeding and Pain (3)
- Painful urge to move the bowels caused by the inflammation (3)
- Fatigue/tiredness(3)
- Loss of appetite(3)
- Weight Loss(3)
- Fever(3)
- Night Sweats
- Dehydration (3)
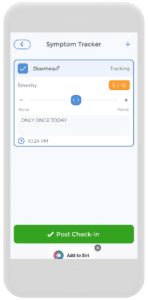
Monitoring these symptoms will be essential for your discussion with your professional healthcare team. And getting your way to living a flare-free life, using the Symptom-Tracker in the CareClinic Platform, you can monitor your symptoms daily, you can also rate your symptoms on a scale of 0-10 and put notes for your reference (in the future, if needed). Yay!
Ulcerative Colitis Diagnosis
Ulcerative Colitis is usually diagnosed by using a wide array of diagnostic testing. First, a patient’s medical and family history must be collected, afterward, a physical exam, laboratory tests, and endoscopic procedures are usually ordered, (1,2) consisting of the following:
- Stool testing (To check for and rule out infection or parasites) (1,2)
- Blood tests (1,2)
- Colonoscopy or sigmoidoscopy (1,2)
- Barium enema X-ray (1,2)
- Video capsule endoscopy (1,2)
- CT/MRI enterography (1,2)
- Tissue biopsy (1,2)
Ulcerative Colitis Treatment
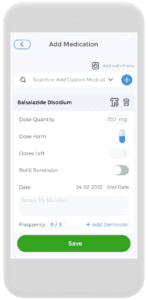
- Anti-inflammatory drugs (2)
- 5-ASA compounds
- Balsalazide (Colazal) (refer to the picture on the right)
- Mesalamine (Asacol, Pentasa, Rowasa, Lialda, Apriso)
- Olsalazine (Dipentum)
- Systemic corticosteroids (prednisone, prednisolone, cortisone)
- Topical corticosteroids
- 5-ASA compounds
- Immunomodulators (2)
- Biologic therapies (2)
- Janus kinase inhibitors (JAK Inhibitors) (2)
Therefore using the CareClinic Platform and the Medication Tracker function to help you keep track of all your medications, as a result, it usually requires more than one medication to keep symptoms from flaring. Life gets busy, so don’t miss a dose and get refill reminders, all in the same convenient place!
Biologic Therapies for Ulcerative Colitis
The most recent innovation in treating ulcerative colitis is what is referred to as biologic therapy. “Biologic therapy is therapy with antibodies directed against molecules that the immune system produces and causes the inflammation”. The most available biologic therapy is directed against a protein produced by the immune system called the tumor necrosis factor. (3)
Increased Risk of Colon Cancer from Ulcerative Colitis
Annual colonoscopies with biopsies may be needed as individuals with Ulcerative Colitis have an increased risk of colon cancer (3).
Surgery for Ulcerative Colitis
Surgery is usually saved as a last resort when all else fails, treating the inflammation, preventing or treating cancer, or treating a complication such as rupture of the colon (3).
Living with Ulcerative Colitis
Dietary Changes from Ulcerative Colitis
There is no scientific correlation between diet and symptoms of ulcerative colitis, therefore, it is also important to ensure that the diet is nutritionally adequate, as ulcers in the intestines may reduce the absorption of essential nutrients, (3) talking to your licensed dietitian and your healthcare team to help you achieve your goals.
Fluid Intake for Ulcerative Colitis
People living with IBD or even IBS will suffer from chronic diarrhea, as diarrhea forces the colon to expel the feces much quicker and decreases the time needed for nutrient absorption, therefore the high water loss in diarrhea can cause dehydration (3).
It is important to maintain an adequate fluid intake- as humans can only live a couple of days with severe dehydration! Scary! The simplest way to judge whether intake is enough for your body is to look at the volume and color of urine each day. A small amount or if the urine is dark in color can suggest that water intake may not be adequate. A suggested amount of liquid to drink each day is half an ounce per pound of weight(3). It is important to discuss this with your physician.
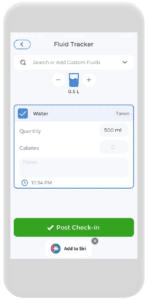
However, using the CareClinic Platform, you can track the amount of water you are intaking. Therefore, you can input different kinds of beverages you may be consuming throughout the day. This open discussion with your healthcare team needs to be as transparent as possible.
Sometimes, what may seem like a harmless beverage may be exacerbating your symptoms. Let’s take the positive step forward and take every precaution to your healthcare goals.
Supplements and Probiotics for Ulcerative Colitis
Depending on the severity, supplements may be needed and will vary from case to case; for example, if a person has blood loss leading to anemia (low red blood cell count), a physician will put the patient on supplementary iron, this will be up to your healthcare team and you to have this important discussion.
Probiotics are “good bacteria” that live symbiotically (in conjunction) in our intestines, as studies have shown that probiotics help people with ulcerative colitis maintain their remissions, (3) this will also be a part of your discussions as well.
Ulcerative Colitis Rash
What does an Ulcerative Colitis Rash Look Like?
Unfortunately, there is no one type of Ulcerative Colitis rash. Quite a few skin manifestations affect a person’s face, stomach, legs, and more! An ulcerative colitis rash can precede bowel disease or bowel exacerbation and should alert clinicians to evaluate the possibility of underlying IBD.
An early diagnosis and intervention with the appropriate therapy can be initiated and may show a better prognosis in the long run,(6) let’s begin breaking down each one with its associated pictures!
Erythema Nodosum (EN)
EN is the most common skin rash patients present with, as it affects about 3–10% of Ulcerative Colitis patients and 4–15% of Crohn’s Disease patients, as EN displays painful, reddish lumps under the skin, usually around the lower legs and ankle region, similarly, these nodules can resemble a bruise on the legs but are not always easily visible.
These bumps only appear with flare-ups and disappear with the resolution of symptoms; above all, to ease the pain, it is recommended to keep your legs elevated and apply a cool compress, as pain relievers, like ibuprofen or naproxen, may also help (4, 6, 7).
Figure 1. EN in the lower legs (7)
Pyoderma Gangrenosum (PG)
PG is the second most common skin rash. It starts with a small, red bump, usually on your legs or near where you had surgery, it grows into a large, painful sore or ulcer within hours or days, as PG is the most severe and debilitating and is more common in ulcerative colitis (5–12%) than Crohn’s (1–2%), it can be difficult to treat, The most common treatment is daily steroids and wound care, and medications you rub on your skin (4, 6, 7).
Figure 2. PG (7)
Acne
For instance, some medications, especially steroids, can cause acne and a puffy face, as other side effects of other drugs may include stretch marks on the stomach region, thin skin, ankle swelling, and slow wound healing (7).
Figure 3. Acne on Face (7)
Pyoderma Vegetans
Pyoderma vegetans can lead to blisters or patches around the groin or under the arms, which get darker as they heal, therefore, there is no standard treatment but directly treating the IBD.
Figure 4. Pyoderma vegetans on the Right Foot (7)
Leukocytoclastic Vasculitis
Vasculitis means “inflammation of the blood vessels,” and leukocytoclastic means “immune cells that build up in blood vessel walls”. It looks like raised red spots on your legs and feet. They are sometimes itchy or painful. If it is severe, they might turn into open sores or large blisters. Vasculitis usually goes away with the treatment of ulcerative colitis (7).
Figure 5. Leukocytoclastic vasculitis in the feet (7)
Vitiligo
Vitiligo makes your skin lose color in blotches as the immune system destroys the melanin skin cells. A supermodel that you may be familiar with, Winnie, has Vitiligo; for instance, it is more common in people with IBD because of a genetic reason or something related to the immune system, as treatments include medicines, creams, and light therapy (7).
Figure 6. Vitiligo in the stomach region (7)
Acquired Epidermolysis Bullosa
It causes blisters on your knees, elbows, hands, and feet by ongoing inflammation in your intestines, as steroids and other types of medicine can treat epidermolysis bullosa (4, 6, 7).
Figure 7. Epidermolysis Bullosa on bilateral hands (7)
Sweet’s Syndrome
For instance, this one is rarer than the other ones listed; however, it will start with a fever when it occurs. Then, tender or painful bumps will appear on the upper limbs, face, or neck.
It becomes difficult to distinguish from EN if it appears on the legs, it is highly treatable with your healthcare team, but Sweet’s Syndrome is more likely to reoccur (4, 6, 7).
Figure 8. Sweet’s Syndrome on the upper shoulder (7)
Bowel-Associated Dermatosis-Arthritis Syndrome (BADAS)
This is a rare problem that might happen after bowel bypass surgery, and it is caused by the “overgrowth of gut bacteria resulting in the production of antibodies to gut bacteria antigen (peptidoglycan) which cross-reacts with skin and joints”.
Symptoms of BADAS will look like Sweet’s syndrome and pyoderma gangrenosum and resolves on their own in about 1-2 weeks (4, 6, 7).
Acrodermatitis Enteropathica
Therefore, due to the reduced mucosa availability for absorption in the colon and chronic diarrhea that can lead to malnutrition, thus zinc is an important nutrient that fails to be absorbed, this is caused by zinc deficiency.
This disorder usually causes a flaky rash or blisters on your hands, feet, face, or genitals. Simple enough: taking a zinc supplement will avoid this (4, 6, 7).
Figure 9. Acrodermatitis Enterpathica (7)
Other Skin Manifestations Associated with IBD
Therefore the ones associated with Ulcerative Colitis only. In addition, IBD is still the umbrella term, and there is a lot of overlap in Crohn’s disease. Although some may appear more often in one versus the other. For example, it is still important to list them to meet a higher understanding. For example, some of the other skin manifestations are below:
- Skin Tags (4, 6, 7)
- Mouth Sores (4, 6, 7)
- Enterocutaneous Fistulas (4, 6, 7)
- Psoriasis (4, 6, 7)
- Perianal Fissures or Fistulas (4, 6, 7)
Ulcerative Colitis Symptoms Rash
Well done for reading this far! It is, honestly, a lot of information to take in, for example, dealing with either IBS or IBD can be a really difficult situation for you, your family, and your social circle. If you are personally dealing with it or know someone, you truly are a superstar.
Ulcerative Colitis Symptoms Rash Tracking
A rash or many other skin manifestations are problematic, therefore, the treatment does not require more medications but treating IBD or IBS.
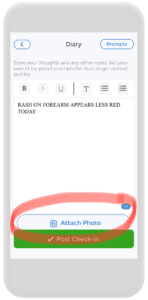
Therefore, remembering a daily log will be impossible to do by yourself in your head. Imagine your physician asking you: “What did your rash look like when it first appeared?” or “Can you show me what it looks like before or after treatment?”.
How will you do any of this? Therefore, do not waste your time during your consultation, use it to your full advantage!
Therefore, using the CareClinic Platform’s Diary Entry is a perfect strategy to incorporate into your daily routine, especially if you are starting to feel your symptoms flare or reside.
Furthermore, the diary function allows you to write what you may be feeling that day (physically or mentally) and attach actual photos associated with your post, you can be on top of your symptoms, rashes, and other health-related needs!
Start on your Ulcerative Colitis Symptoms Rash relief today by using your Android or iOS devices to download the CareClinic Platform.