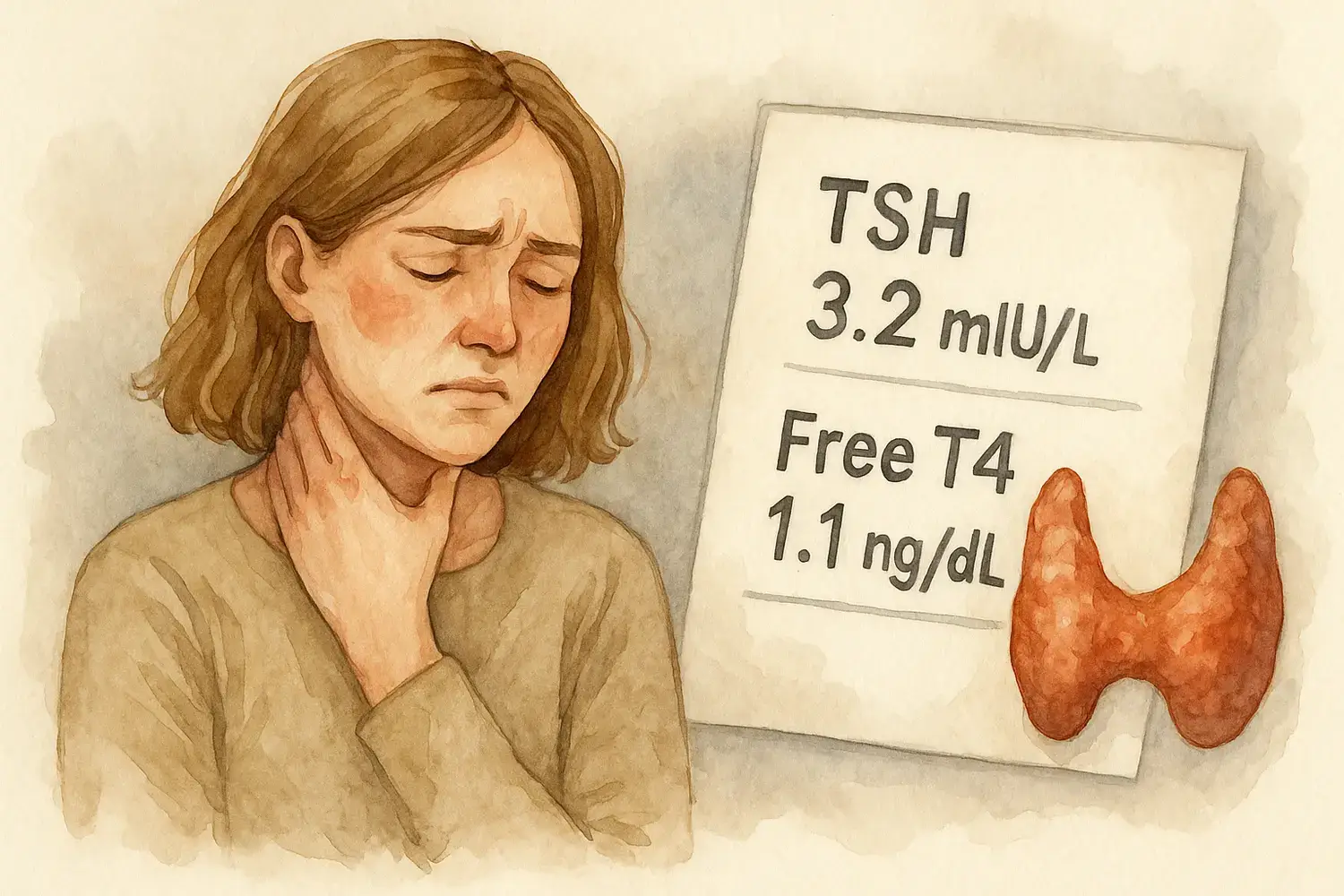
Your thyroid lab results arrive, but the numbers feel like a foreign language. TSH is 3.2 mIU/L, Free T4 shows 1.1 ng/dL, and your doctor says “everything looks normal.” Yet you still feel exhausted, gain weight easily, and struggle with brain fog. Sound familiar?
Understanding thyroid lab values requires more than checking whether numbers fall within reference ranges. Optimal levels differ from normal ranges. Timing matters. Individual variation exists. This guide breaks down each test, explains what the numbers really mean, and shows you how to track patterns that reveal the complete picture of your thyroid health.
Table of Contents
- Why Standard Lab Interpretation Often Falls Short
- Complete Thyroid Lab Panel Breakdown
- Thyroid Antibody Tests Explained
- Advanced Thyroid Markers
- Factors That Affect Thyroid Lab Results
- Reading Your Lab Report Like a Pro
- When Lab Results Don’t Match Symptoms
- Optimal vs Normal Thyroid Lab Values
- Tracking Lab Trends with Digital Tools
- Working with Healthcare Providers on Lab Interpretation
- Special Considerations for Different Patient Groups
- Common Lab Interpretation Mistakes
- Lab Monitoring During Treatment
- Understanding Complex Lab Patterns
- Building Your Lab Tracking System
- The Final Message
Why Standard Lab Interpretation Often Falls Short
Reference ranges represent 95% of the population tested, including people with undiagnosed thyroid disease. A 2019 study in the European Journal of Endocrinology found that 15% of people with “normal” TSH levels between 2.5-4.0 mIU/L had underlying thyroid dysfunction when antibodies were tested.
Most labs use outdated reference ranges established decades ago. The American Association of Clinical Endocrinologists recommends TSH levels between 0.3-3.0 mIU/L for optimal function, narrower than the standard 0.4-4.0 range most labs report.
Single test snapshots miss fluctuations. TSH varies by time of day, season, stress levels, and illness. Free T4 and Free T3 provide better insight into actual hormone availability. Antibody tests reveal autoimmune processes that standard panels miss entirely. Understanding these nuances becomes crucial for effective thyroid management. A comprehensive approach combines lab interpretation with symptom tracking to guide treatment decisions.
CareClinic’s lab tracking feature stores all your thyroid results with timestamps, creating trend analysis that shows patterns over time. Upload lab reports directly or enter values manually. The correlation engine identifies relationships between lab changes and symptom severity.
Complete Thyroid Lab Panel Breakdown
TSH (Thyroid Stimulating Hormone)
TSH measures how hard your pituitary gland works to stimulate thyroid hormone production. Higher TSH indicates your thyroid needs more stimulation to produce adequate hormones.
| TSH Level (mIU/L) | Standard Interpretation | Functional Medicine View | Symptoms Often Present |
|---|---|---|---|
| 0.1-0.3 | Low Normal | Potentially Hyperthyroid | Anxiety, rapid heart rate, insomnia |
| 0.4-1.0 | Normal | Optimal Range | Most people feel best here |
| 1.1-2.0 | Normal | Acceptable | May have mild symptoms |
| 2.1-3.0 | Normal | Suboptimal | Fatigue, weight gain, mood changes |
| 3.1-4.0 | Normal | Subclinical Hypothyroid | Multiple hypothyroid symptoms |
| 4.1+ | High | Hypothyroid | Significant symptoms requiring treatment |
Research published in Archives of Internal Medicine tracked 25,000 people for 20 years. Those with TSH above 2.0 had significantly higher rates of thyroid failure requiring hormone replacement therapy.
Free T4 (Free Thyroxine)
Free T4 measures unbound thyroid hormone available to cells. Total T4 includes protein-bound hormone that cells cannot use. Free T4 provides accurate assessment of thyroid hormone availability.
Normal range: 0.9-1.7 ng/dL (ranges vary by lab)
Optimal range: 1.3-1.5 ng/dL for most people
Low Free T4 with high TSH confirms primary hypothyroidism. Low Free T4 with normal/low TSH suggests central hypothyroidism (pituitary problem). High Free T4 with low TSH indicates hyperthyroidism.
Medication timing affects results. Take thyroid hormone replacement 24 hours before blood draw for accurate readings. Biotin supplements can interfere with lab assays, causing falsely elevated results.
Free T3 (Free Triiodothyronine)
T3 is the active thyroid hormone. Your body converts T4 to T3 in peripheral tissues. Some people have conversion problems, maintaining normal T4 levels while producing insufficient T3.
Normal range: 2.3-4.2 pg/mL (varies by lab)
Optimal range: 3.2-4.0 pg/mL
Free T3 testing reveals conversion issues missed by TSH and Free T4 alone. Stress, illness, certain medications, and nutrient deficiencies impair T4 to T3 conversion. Reverse T3 (rT3) blocks T3 receptors, creating functional hypothyroidism despite normal lab values.
Calculate your Free T3 to Free T4 ratio: (Free T3 × 100) ÷ Free T4. Healthy ratios fall between 20-30. Lower ratios suggest conversion problems.
Reverse T3 (rT3)
Reverse T3 is an inactive form of T3 that blocks thyroid hormone receptors. High rT3 creates symptoms of hypothyroidism even when Free T3 levels appear normal.
Normal range: 10-24 ng/dL
Optimal range: 12-18 ng/dL
Chronic stress, illness, calorie restriction, and certain medications increase rT3 production. High rT3 with normal Free T3 explains persistent symptoms despite “normal” thyroid labs.
CareClinic users can track stress levels, sleep quality, and dietary changes alongside rT3 results to identify triggers that increase production of this blocking hormone.
Thyroid Antibody Tests Explained
TPO Antibodies (Anti-Thyroid Peroxidase)
TPO antibodies attack the enzyme needed for thyroid hormone production. Elevated levels indicate Hashimoto’s thyroiditis, the most common cause of hypothyroidism in developed countries.
Normal range: <35 IU/mL (varies by lab) Hashimoto’s diagnosis: >100 IU/mL
TPO antibodies can be elevated years before TSH becomes abnormal. Early detection allows intervention to slow thyroid destruction. Levels may fluctuate based on stress, infections, and dietary triggers.
Thyroglobulin Antibodies (TgAb)
Thyroglobulin antibodies target the protein scaffold where thyroid hormones are made. These antibodies are present in 10-20% of people with Hashimoto’s disease, sometimes appearing when TPO antibodies are normal.
Normal range: <4 IU/mL Elevated: >20 IU/mL
TgAb testing is particularly important for thyroid cancer survivors. Rising levels may indicate cancer recurrence. For Hashimoto’s patients, TgAb levels help monitor autoimmune activity.
TSI/TRAb (Thyroid Stimulating Immunoglobulin/TSH Receptor Antibodies)
These antibodies mimic TSH, overstimulating the thyroid and causing hyperthyroidism. They confirm Graves’ disease diagnosis and help predict treatment response.
TSI normal range: <140%
TRAb normal range: <1.75 IU/L
High levels predict treatment difficulty and increased relapse risk. Monitoring during treatment helps assess remission probability. Pregnant women with Graves’ disease need monitoring because these antibodies cross the placenta.
Advanced Thyroid Markers
Thyroglobulin (Tg)
Thyroglobulin is a protein produced by thyroid cells. It’s primarily used to monitor thyroid cancer recurrence after total thyroidectomy. In people with intact thyroids, elevated levels may indicate thyroid inflammation or nodular disease.
Post-thyroidectomy goal: <0.2 ng/mL
With thyroid present: 1.5-38.5 ng/mL
Calcitonin
Calcitonin is produced by C-cells in the thyroid. Elevated levels may indicate medullary thyroid cancer, though other conditions can cause increases.
Normal range: <10 pg/mL for men, <5 pg/mL for women
This test is not routinely ordered but may be included when evaluating thyroid nodules or family history of medullary thyroid cancer.
Factors That Affect Thyroid Lab Results
Timing and Preparation
TSH follows a circadian rhythm, peaking between 2-4 AM and reaching lowest levels in the afternoon. Blood draws between 7-9 AM provide most consistent results. Avoid testing during illness, as stress hormones temporarily alter thyroid function.
Fast for 12 hours before testing if cholesterol levels are included. TSH can be measured non-fasting, but Free T4 and Free T3 may be more accurate with fasting.
Take thyroid medication after blood draw, not before. Levothyroxine peaks 2-4 hours after ingestion, potentially skewing Free T4 results.
Medications and Supplements That Interfere
| Substance | Effect on Labs | Recommended Action |
|---|---|---|
| Biotin (>5mg daily) | Falsely elevates Free T4, Free T3 | Stop 72 hours before testing |
| Levothyroxine | Elevates Free T4 if taken before test | Take after blood draw |
| Liothyronine (T3) | Elevates Free T3, suppresses TSH | Timing depends on formulation |
| Estrogen/Birth Control | Increases binding proteins | Use Free hormone tests |
| Lithium | May lower Free T4, raise TSH | Cannot discontinue – note on requisition |
| Amiodarone | Complex effects on all thyroid tests | Requires specialized interpretation |
Illness and Stress Effects
Non-thyroidal illness syndrome (sick euthyroid syndrome) causes abnormal thyroid labs during acute illness. TSH may be low, Free T4 normal, and Free T3 decreased. These changes usually resolve with recovery.
Chronic stress increases cortisol, which blocks T4 to T3 conversion and increases reverse T3. The CareClinic app’s stress tracking helps identify correlations between stressful periods and changes in thyroid function.
Reading Your Lab Report Like a Pro
Understanding Reference Ranges
Lab reference ranges show the middle 95% of values from the tested population. This includes people with undiagnosed thyroid disease, explaining why “normal” ranges may be too broad for optimal health.
Different labs use different testing methods and equipment, creating varying reference ranges. Always compare your results to the specific range provided by the testing laboratory.
Pregnancy requires different reference ranges. TSH should be <2.5 mIU/L in the first trimester and <3.0 mIU/L in later pregnancy. Free T4 targets are higher during pregnancy.
Patterns That Matter More Than Individual Values
TSH and Free T4 moving in opposite directions confirms primary thyroid dysfunction. Rising TSH with falling Free T4 indicates hypothyroidism. Falling TSH with rising Free T4 suggests hyperthyroidism.
Normal TSH with low Free T4 may indicate central hypothyroidism (pituitary problem). This requires specialized evaluation and different treatment approaches.
Antibody trends predict disease progression. Rising TPO antibodies in Hashimoto’s patients may signal need for treatment adjustment. Falling TSI levels in Graves’ disease indicate remission.
When Lab Results Don’t Match Symptoms
Subclinical Thyroid Disease
Subclinical hypothyroidism occurs when TSH is elevated (>4.0 mIU/L) but Free T4 remains normal. About 3-8% of the population has this condition. Symptoms may be present despite “normal” Free T4 levels.
Treatment recommendations vary. The American Thyroid Association suggests treatment when TSH exceeds 10 mIU/L or when symptoms are present with TSH 4.5-10 mIU/L.
Subclinical hyperthyroidism involves suppressed TSH (<0.4 mIU/L) with normal Free T4 and Free T3. This condition increases risks of atrial fibrillation and osteoporosis, particularly in older adults.
Tissue Resistance and Conversion Problems
Some people have genetic variations affecting thyroid hormone transport or receptor sensitivity. They may need higher hormone levels to achieve symptom relief.
Poor T4 to T3 conversion creates normal Free T4 with low Free T3. Causes include:
– Chronic stress
– Nutrient deficiencies (selenium, zinc, iron)
– Chronic illness
– Certain medications
– Aging
Reverse T3 dominance blocks thyroid hormone receptors despite adequate Free T3 levels. This requires specialized testing and treatment approaches.
Optimal vs Normal Thyroid Lab Values
What Functional Medicine Practitioners Target
| Test | Standard Range | Optimal Range | Why It Matters |
|---|---|---|---|
| TSH | 0.4-4.0 mIU/L | 0.5-2.0 mIU/L | Most people feel best in lower half |
| Free T4 | 0.9-1.7 ng/dL | 1.3-1.5 ng/dL | Upper third of range often ideal |
| Free T3 | 2.3-4.2 pg/mL | 3.2-4.0 pg/mL | Active hormone should be robust |
| Reverse T3 | 10-24 ng/dL | 12-18 ng/dL | Lower levels allow better T3 function |
| TPO Antibodies | <35 IU/mL | <10 IU/mL | Lower indicates less autoimmune activity |
Individual Variation in Optimal Levels
Your personal optimal ranges may differ from population averages. Some people feel best with TSH near 1.0 mIU/L, while others prefer levels closer to 2.0 mIU/L.
Age affects optimal ranges. Older adults may tolerate slightly higher TSH levels better than younger people. Pregnancy requires lower TSH targets for fetal development.
Athletes and highly active individuals often need Free T3 in the upper normal range to support metabolic demands. Sedentary individuals may function well with lower levels.
Tracking Lab Trends with Digital Tools
CareClinic Lab Tracking Features
The CareClinic app’s lab module stores unlimited thyroid test results with automatic trend graphing. Upload lab reports as photos or PDFs, or enter values manually. The system tracks changes over time and correlates lab values with symptom severity scores.
Set up lab reminders based on your testing schedule. Most thyroid patients need labs every 3-6 months initially, then annually once stable. The app sends notifications when testing is due.
Generate reports combining lab trends with symptom patterns for healthcare provider visits. Export data as PDFs or share directly from the app during appointments.
Creating Your Personal Thyroid Lab Database
Document testing conditions for each lab draw:
– Time of day blood was drawn
– Last thyroid medication dose timing
– Supplements taken that week
– Illness or stress levels
– Menstrual cycle phase (for women)
Note any lab changes and corresponding symptom shifts. Rising TSH with increasing fatigue confirms the need for medication adjustment. Stable labs with worsening symptoms may indicate conversion problems requiring additional testing.
Track medication changes alongside lab results. Dose adjustments should correlate with lab improvements within 6-8 weeks for synthetic hormones.
Working with Healthcare Providers on Lab Interpretation
Questions to Ask About Your Results
“What are my exact numbers, not just whether they’re normal?”
“Where do my values fall within the reference range?”
“Have my levels changed compared to previous tests?”
“Could my symptoms be related to thyroid function despite normal TSH?”
“Should we test thyroid antibodies to check for autoimmune disease?”
“Would Free T3 testing provide additional information?”
Preparing for Lab Review Appointments
Bring printed copies of all previous thyroid labs, including results from other healthcare providers. Create a timeline showing lab changes correlated with symptom changes.
Use CareClinic’s correlation reports to show relationships between lab values and daily symptoms. Document how you felt during the weeks surrounding each lab draw.
Research your family history of thyroid disease. Genetic factors influence optimal hormone levels and treatment response.
Special Considerations for Different Patient Groups
Pregnancy and Thyroid Labs
Pregnancy dramatically changes thyroid hormone requirements. Human chorionic gonadotropin (hCG) stimulates the thyroid in early pregnancy, potentially lowering TSH.
First trimester TSH should be <2.5 mIU/L, second and third trimesters <3.0 mIU/L. Free T4 targets are 10-15% higher than non-pregnant ranges.
Thyroid antibodies pose additional pregnancy risks. TPO antibodies increase miscarriage risk and postpartum thyroiditis. Graves’ disease antibodies can cross the placenta, affecting fetal thyroid function.
Older Adults and Thyroid Function
TSH naturally increases with age. Reference ranges may need adjustment for adults over 65. Some endocrinologists accept TSH up to 5.0-6.0 mIU/L in healthy elderly patients without symptoms.
Cardiac considerations become more important with age. Thyroid hormone replacement in older adults requires careful monitoring to avoid atrial fibrillation and bone loss.
Medication absorption may decrease with age due to reduced stomach acid and slower gastrointestinal transit. Free hormone levels become more important than TSH for monitoring treatment adequacy.
Athletes and Active Individuals
Intense training affects thyroid function through changes in cortisol, inflammation, and metabolic demands. Athletes may need higher Free T3 levels to support performance and recovery.
Low T3 syndrome can develop with excessive training volume or inadequate nutrition. This manifests as normal TSH and Free T4 with low Free T3.
Regular lab monitoring helps distinguish between training-induced changes and true thyroid dysfunction in athletes.
Common Lab Interpretation Mistakes
Relying Only on TSH
TSH-only testing misses 10-15% of thyroid dysfunction cases. Central hypothyroidism, T3-only toxicosis, and conversion problems all require additional testing beyond TSH.
Normal TSH doesn’t rule out thyroid disease when symptoms are present. Free T4, Free T3, and antibody testing provide crucial additional information.
Ignoring Antibody Tests
Antibody testing identifies autoimmune thyroid disease early, often before TSH becomes abnormal. This allows intervention to slow disease progression.
Hashimoto’s thyroiditis can cause fluctuating symptoms even with normal TSH. Antibody levels help explain symptom variability and guide treatment decisions.
Not Considering Optimal Ranges
Many patients feel significantly better when thyroid levels are optimized within the normal range rather than simply “not abnormal.”
Individual variation means some people need TSH near 1.0 mIU/L while others feel best at 2.5 mIU/L. Symptom tracking helps identify personal targets.
Lab Monitoring During Treatment
Initial Treatment Phase
New thyroid patients need labs every 6-8 weeks until levels stabilize. TSH responds slowly to medication changes, requiring patience during dose adjustments.
Free T4 changes more quickly than TSH, often normalizing within 2-4 weeks of appropriate dosing. Free T3 may take longer to optimize, particularly in patients with conversion issues.
Symptom improvement typically lags behind lab normalization by 2-6 weeks. Don’t expect immediate relief when labs first normalize.
Maintenance Monitoring
Stable patients on consistent doses need labs every 6-12 months. Any symptom changes warrant earlier testing regardless of scheduled timing.
Medication changes due to manufacturer switches, other drug interactions, or weight changes require lab monitoring within 6-8 weeks.
Life changes affecting thyroid hormone needs include pregnancy, significant weight loss/gain, other medications, or development of other medical conditions.
Understanding Complex Lab Patterns
Mixed Hyperthyroid and Hypothyroid Symptoms
Some patients experience symptoms of both conditions simultaneously. This may indicate:
– Hashitoxicosis (Hashimoto’s with transient hyperthyroid phase)
– Over-replacement therapy
– Conversion problems with high reverse T3
– Mixed autoimmune conditions
Normal Labs with Persistent Symptoms
When standard thyroid labs are normal but symptoms persist, consider:
– Adrenal dysfunction affecting thyroid hormone utilization
– Sex hormone imbalances
– Nutrient deficiencies (B12, vitamin D, iron)
– Sleep disorders
– Other autoimmune conditions
CareClinic’s multi-condition tracking helps identify patterns that point toward root causes when thyroid labs appear normal.
Building Your Lab Tracking System
Setting Up Effective Monitoring
Create a systematic approach to lab tracking that includes:
– Regular testing schedule based on your treatment phase
– Consistent timing for blood draws
– Documentation of all factors affecting results
– Correlation with symptom patterns
– Long-term trend analysis
How Best To Speak To Your Careprovider
Share your lab tracking data proactively during appointments. Providers appreciate patients who come prepared with organized information.
Use visual trend reports from CareClinic to highlight concerning patterns or treatment successes. Data presentation improves communication and clinical decision-making.
Request copies of all lab results for your personal records. Many healthcare systems now provide patient portals for easy access, but maintaining your own database ensures continuity of care.
The Final Message
Reading thyroid labs requires understanding that optimal health extends beyond normal reference ranges. Your numbers tell a story when viewed over time and correlated with symptoms. TSH alone provides insufficient information for most thyroid conditions.
Comprehensive panels, including Free T4, Free T3, and relevant antibodies, offer clearer pictures of thyroid function. Advanced markers like reverse T3 explain persistent symptoms despite normal standard labs.
Digital tracking through platforms like CareClinic transforms isolated lab values into meaningful health insights. Correlating lab trends with daily symptoms, medication changes, and lifestyle factors guides optimization of thyroid health.
The path to feeling your best starts with understanding what your numbers really mean. Armed with this knowledge and systematic tracking tools, you can advocate effectively for optimal thyroid care rather than settling for “normal” results that leave you feeling unwell.
Remember that thyroid health extends beyond lab values. Symptoms matter. Quality of life matters. Your individual optimal ranges may differ from population averages. Work with healthcare providers who understand these principles and support your journey toward optimal thyroid function.


