Chronic musculoskeletal pain affects millions of people around the world, and it can have a profound impact on quality of life. Traditional pain medications provide some pain relief, but they come with a range of side effects and limitations. As such, an increasing number of healthcare professionals are exploring non-pharmacological approaches to chronic pain management. In this article, we’ll explore these methods and their potential benefits.[1][2][3]
Understanding Chronic Pain
Before we dive into non-pharmacological approaches, let’s first define what we mean by chronic pain. Essentially, chronic pain is pain that persists for longer than three months. This type of pain can be caused by a wide range of conditions, from arthritis and fibromyalgia to back injuries and neuropathic pain. Chronic pain is often associated with a range of physical and emotional symptoms, including fatigue, anxiety, and depression.
Defining Chronic Pain
According to the International Association for the Study of Pain, chronic pain is defined as “pain that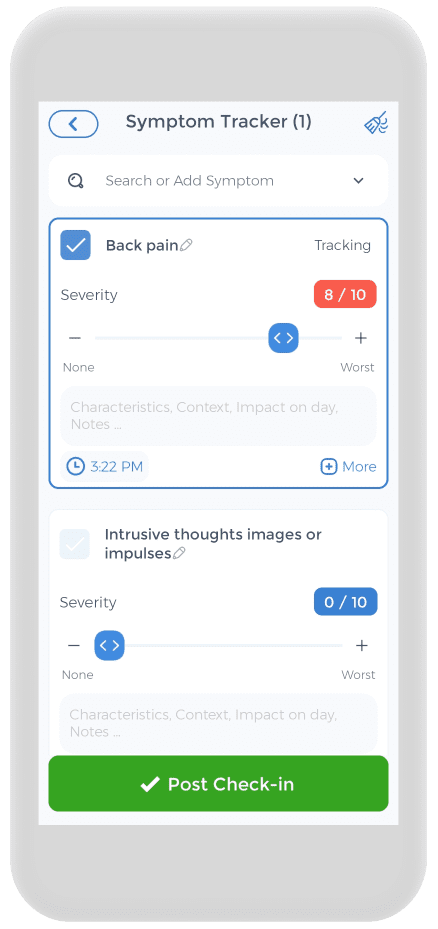 persists or recurs for longer than three months.” This type of pain is often debilitating, and it can interfere with an individual’s ability to complete day-to-day tasks.
persists or recurs for longer than three months.” This type of pain is often debilitating, and it can interfere with an individual’s ability to complete day-to-day tasks.
It is important to note that chronic pain is different from acute pain. Acute pain is a normal sensation that alerts us to possible injury or damage to our bodies. Acute pain typically lasts for a short time and can be managed with medication and other treatments. Chronic pain, on the other hand, persists for longer periods and can be more difficult to manage.
Causes of Chronic Pain
The causes of chronic noncancer pain are varied, but they can be broadly classified into two categories: nociceptive pain and neuropathic pain. Nociceptive pain comes from damage to the body’s tissues, while neuropathic pain is caused by damage or dysfunction of the peripheral and central nervous system (brain and spinal cord). Common causes of how individuals develop chronic pain include arthritis, muscle pain, back injuries, fibromyalgia, and nerve damage.
In some cases, chronic pain can be a symptom of an underlying medical condition, such as cancer or multiple sclerosis, which can make chronic pain worse. It is important to work with a healthcare provider to determine the cause of chronic pain and develop an appropriate plan to treat chronic pain.
The Impact of Chronic Pain on Quality of Life
Chronic pain can have a significant impact on quality of life. In addition to the physical symptoms of pain, chronic pain is often associated with emotional symptoms such as anxiety and depression. Chronic low back and neck pain can also interfere with an individual’s ability to work, socialize, and participate in leisure activities.
Individuals with chronic pain need to work with a healthcare provider to develop a comprehensive treatment plan that addresses both the physical and emotional aspects of pain. Non-pharmacological approaches, such as physical therapy, acupuncture, and cognitive-behavioral therapy, can be effective in managing chronic pain and improving quality of life.
It is also important for chronic pain patients to practice self-care techniques, such as getting enough sleep, eating a healthy diet, and engaging in regular exercise. These strategies can help manage pain and improve overall well-being.[4][5][6]
The Limitations of Pharmacological Treatments
Pharmacological treatments, such as nonsteroidal anti-inflammatory drugs, have been a popular choice for managing and treating pain for decades. They can provide some chronic pain relief, but they come with a range of limitations and potential side effects that should be taken into consideration before starting any treatment.
Most chronic pain patients have decreased quality of life. While pharmacological treatments can be effective in decreasing pain, they are not without their drawbacks.
Side Effects of Pain Medications
Some of the most common side effects of pain medicine, such as nonsteroidal anti-inflammatory drugs, include nausea, dizziness, and drowsiness. These side effects can be particularly problematic for individuals who need to drive or operate heavy machinery as part of their daily routine.
Pain medications can also cause constipation, dry mouth, and difficulty urinating. These side effects can be especially challenging for individuals who are already dealing with other health issues.
The Risk of Addiction and Overdose
One of the biggest concerns with pain medications is the risk of addiction and overdose. Opioid therapy, in particular, can be highly addictive and has contributed to the ongoing opioid epidemic in the United States.
It’s important to note that not everyone who takes pain medications will become addicted. However, the risk of addiction should be taken seriously, and individuals who are prescribed pain medications should be closely monitored by their healthcare provider.
Ineffectiveness for Some Patients
Finally, it’s worth noting that pain medications may not be effective for all patients. Some individuals may have a reduced response to pain medications, or they may have side effects that prevent them from taking these medications.
For these individuals, alternative treatments such as physical therapy, acupuncture, or cognitive-behavioral therapy may be more effective in managing their chronic pain.
In conclusion, while pharmacological treatments can be effective in managing chronic pain, they come with a range of limitations and potential side effects that should be carefully considered. It’s important for individuals to work closely with their healthcare provider to determine the best course of treatment for their specific needs.[7][8][9][10][11]
Non-Pharmacological Approaches to Chronic Pain Treatment
Chronic pain is a complex condition that affects millions of people worldwide. While pharmacological treatments can be effective in managing pain, they often come with side effects and the risk of addiction. As a result, many healthcare professionals are exploring non-pharmacological approaches to chronic pain treatment. These methods can relieve chronic pain without the negative consequences associated with pain medications.
Cognitive-Behavioral Therapy (CBT)
![]() Cognitive-behavioral therapy (CBT) is a type of talk therapy that helps individuals learn coping skills for managing their pain. This type of therapy can be helpful for individuals with chronic pain, as it can help them reframe their thoughts about pain and develop strategies for managing their symptoms. CBT can also help individuals address any underlying psychological issues that may be contributing to their pain.
Cognitive-behavioral therapy (CBT) is a type of talk therapy that helps individuals learn coping skills for managing their pain. This type of therapy can be helpful for individuals with chronic pain, as it can help them reframe their thoughts about pain and develop strategies for managing their symptoms. CBT can also help individuals address any underlying psychological issues that may be contributing to their pain.
For example, if an individual with chronic pain has depression or anxiety, CBT can help them learn how to manage these conditions in addition to their pain. Additionally, CBT can help individuals develop healthy coping mechanisms for dealing with stress, which can exacerbate chronic neck pain.
Mindfulness and Meditation
Mindfulness and meditation are practices that can help individuals focus on the present moment and reduce stress. These practices are effective in managing chronic pain. Mindfulness involves paying attention to one’s thoughts and feelings without judgment, while meditation involves focusing one’s attention on a specific object or activity, such as breathing.
Research has shown that mindfulness-based stress reduction can reduce pain intensity and improve quality of life in individuals with chronic pain. These practices can also help individuals manage the emotional distress that often accompanies chronic pain, such as anxiety and depression.
Physical Therapy and Exercise
Physical therapy and exercise can help reduce pain and improve function in individuals with chronic pain. It may include exercises to improve strength and flexibility, as well as manual therapy techniques to reduce pain and improve mobility.
Exercise can also help to reduce inflammation in the body, which can contribute to chronic pain. For example, low-impact exercises such as swimming and yoga can be effective in reducing chronic low back pain and improving physical function in individuals with chronic low back pain.
Acupuncture and Traditional Chinese Medicine
Acupuncture and traditional Chinese medicine are alternative therapies to pain management that have been used in many cultures for centuries. These methods involve the use of needles, herbs, and other techniques to help reduce pain and improve overall health.
Acupuncture involves the insertion of thin needles into specific points on the body, which can stimulate the body’s natural pain-relieving mechanisms. Traditional Chinese medicine may also involve the use of herbal remedies and dietary changes to improve overall health and relieve chronic pain.
Massage Therapy and Bodywork
Massage therapy and bodywork involve the use of manual techniques to help reduce pain and improve flexibility. These methods can be especially helpful for individuals with common chronic pain conditions.
Massage therapy can help to reduce muscle tension and improve circulation, which can help to reduce pain and promote healing. Bodywork techniques such as myofascial release and trigger point therapy can also be effective in reducing pain and improving physical function.
Biofeedback and Relaxation Techniques
Biofeedback and relaxation techniques are methods for managing chronic pain that involve learning to control physiological responses to pain. These methods can help individuals with pain and improve their ability to cope with their symptoms.
Biofeedback involves using electronic devices to monitor physiological responses to pain, such as heart rate and muscle tension. By learning to control these responses, individuals can reduce pain and improve their overall sense of well-being. Relaxation techniques such as deep breathing, progressive muscle relaxation, and guided imagery can also be effective in reducing pain and promoting relaxation.
Nutritional and Lifestyle Changes
Finally, nutritional and lifestyle changes can play a role in chronic pain management. Eating a healthy diet and getting regular exercise can help individuals reduce inflammation and improve overall health. Additionally, activities such as yoga and tai chi can help individuals reduce stress and improve their ability to manage pain.
Other lifestyle changes that may be helpful for individuals with chronic back pain include getting enough sleep, reducing stress, and avoiding activities that exacerbate pain. By making these changes, individuals can improve their overall health and reduce the impact of chronic pain on their daily lives.[12][13][14][15]
Integrating Non-Pharmacological Approaches into a Comprehensive Pain Management Plan
Patients suffering from chronic pain may benefit from a comprehensive pain management plan that includes a range of non-pharmacological approaches. Chronic pain can be a complex and challenging condition to manage, and it often requires a multifaceted approach. While medications can be an important part of pain management, they are not always effective on their own. Non-pharmacological approaches can provide additional benefits and improve overall outcomes.
Non-pharmacological approaches to pain management can include a variety of techniques and therapies, such as physical therapy, cognitive-behavioral therapy, acupuncture, massage therapy, and mindfulness meditation. These approaches can help individuals manage their pain, reduce stress and anxiety, and improve overall quality of life.
Assessing Individual Needs and Preferences
Assessing individual needs and preferences is an important part of developing a comprehensive pain management plan. Healthcare professionals can work with patients to understand their goals for pain management and develop a plan that meets those needs. This may involve evaluating the patient’s medical history, conducting a physical exam, and discussing the patient’s current symptoms and pain levels.
It’s also important to consider the patient’s personal preferences and lifestyle when developing a pain management plan. For example, some patients may prefer non-pharmacological approaches, while others may prefer to use medications. By taking into account the patient’s individual needs and preferences, healthcare professionals can develop a plan that is tailored to the patient’s unique situation.
Developing a Multidisciplinary Team
A multidisciplinary team of healthcare providers can provide a range of services and support for individuals with chronic pain. This team may include primary care physicians, physical therapists, mental health professionals, and alternative medicine practitioners. By working together, these professionals can provide a comprehensive approach to pain management that addresses the physical, emotional, and psychological aspects of chronic pain.
Physical therapists can help patients improve their strength, flexibility, and mobility, which can help reduce pain and improve overall function. Mental health professionals can work with patients to develop coping strategies and address any underlying psychological factors that may be contributing to their pain. Alternative medicine practitioners, such as acupuncturists and massage therapists, can provide additional pain relief and relaxation techniques.
Monitoring Progress and Adjusting Pain Treatment as Needed
Finally, it’s important to monitor progress over time and adjust treatment plans as needed. A comprehensive pain management plan should be a dynamic process that evolves and adapts as the individual’s needs change. Healthcare professionals can track the patient’s pain levels, functional abilities, and overall quality of life to determine if the current treatment plan is effective.
If the patient is not experiencing adequate pain relief or is experiencing side effects from medications, the treatment plan may need to be adjusted. This may involve trying different non-pharmacological approaches, adjusting medication dosages, or referring the patient to a specialist for further evaluation.[16][17][18][19]
The Future of Non-Pharmacological Chronic Pain Management
The field of non-pharmacological chronic pain management is constantly evolving, and new therapies and technologies are emerging all the time. This is great news for the millions of people who suffer from chronic pain and are looking for alternatives to traditional pain medications.
Emerging Therapies and Technologies
Virtual reality therapy is one emerging technology that has shown promise in managing chronic pain. By immersing patients in a virtual world, it can distract them from their pain and provide a sense of relaxation. Transcranial magnetic stimulation is another promising therapy that uses magnetic fields to stimulate nerve cells in the brain, which can help reduce pain. Bioelectronic medicine is also being explored as a potential treatment for chronic pain, using electrical impulses to regulate the body’s natural functions and reduce pain signals.
The Role of Patient Education and Advocacy
Patient education and advocacy will play a critical role in the future of chronic pain management. As more individuals seek non-pharmacological options for pain management, they must have access to accurate information and resources. Patients should be empowered to make informed decisions about their treatment options and have access to a variety of non-pharmacological therapies.
Advocacy is also important in ensuring that these therapies are covered by insurance and widely available. Patients and healthcare professionals can work together to advocate for increased research funding and policy changes that support non-pharmacological pain management.
Overcoming Barriers to Access and Acceptance
Finally, overcoming barriers to access and acceptance will be a key challenge for the field of non-pharmacological chronic pain management. Healthcare professionals, policymakers, and patients will need to work together to ensure that these methods are widely available and accepted as a legitimate approach to pain management.
One barrier to access is the cost of some of these therapies. Patients may not be able to afford them or may not have insurance coverage for them. This highlights the need for increased research funding to make these therapies more affordable and accessible to patients.
Another barrier is the lack of awareness and acceptance of non-pharmacological therapies among healthcare professionals. Many physicians may not be familiar with these therapies or may not believe in their effectiveness. Education and training for healthcare professionals can help increase awareness and acceptance of these therapies.
In conclusion, the future of non-pharmacological chronic pain management looks promising, with new therapies and technologies emerging all the time. However, patient education, advocacy, and overcoming barriers to access and acceptance will be critical in ensuring that these methods are widely available and accepted as a legitimate approach to pain management.[20][21][22]
Using the CareClinic App to Manage Pain
Having a pain tracker app is crucial for your health, and the CareClinic app can help with that. You can use the![]() app as your health and clinical journal. Just go to the pain diary section of the app and enter your daily symptoms, medications, and other triggers, as they occur.
app as your health and clinical journal. Just go to the pain diary section of the app and enter your daily symptoms, medications, and other triggers, as they occur.
This can help you be aware of early warning signs. Whether you suffer from chronic low back pain, chronic tension headache, impaired physical and mental functioning, chronic headaches, chronic widespread pain, chronic musculoskeletal pain, chronic neck pain, or depressive and anxiety disorders, the app is here to help you improve your chronic pain-related health.
The app also has a medication section where you can precisely track the pain therapies you are undergoing, whether it be superficial heat, spinal manipulation, relaxation therapy, or transcutaneous electrical nerve stimulation. Hopefully, having all this information handy will help you with treating chronic pain conditions. You can also see our review of Apps such as Visible to understand why CareClinic can help much more.
Non-pharmacological approaches to chronic pain management offer a range of benefits for individuals with chronic pain. From cognitive-behavioral therapy and mindfulness meditation to acupuncture and nutritional changes, there are a wide variety of options available. By working with healthcare professionals to develop a comprehensive pain management plan, individuals with chronic pain can reduce their reliance on pain medications and improve their quality of life.
Sources
- https://www.ninds.nih.gov/health-information/disorders/pain
- https://painbc.ca/health-professionals/education/OT-workshop
- https://austinpaindoctor.com/your-pain-care-plan-to-occupational-pain-management
References
- “Musculoskeletal health”. https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions
- “Non-pharmacological treatment of chronic widespread musculoskeletal pain”. https://pubmed.ncbi.nlm.nih.gov/22094203/
- “Chronic Musculoskeletal Pain: Nonpharmacologic, Noninvasive Treatments | AAFP”. https://www.aafp.org/pubs/afp/issues/2020/1015/p465.html/
- “Pain Management Center – Chapter 1 – International Association for the Study of Pain (IASP)”. https://www.iasp-pain.org/resources/toolkits/pain-management-center/chapter1/
- “Chronic pain management: nonpharmacological therapies for chronic pain – PubMed”. https://pubmed.ncbi.nlm.nih.gov/25970869/
- “Non-Drug Approaches to Chronic Pain – Whole Health Library”. https://www.va.gov/WHOLEHEALTHLIBRARY/tools/non-drug-approaches-to-chronic-pain.asp
- “Nonsteroidal anti-inflammatory drugs: adverse effects and their prevention – PubMed”. https://pubmed.ncbi.nlm.nih.gov/18823646/
- “What opioid use disorder costs Pennsylvania”. https://www.axios.com/local/pittsburgh/2025/05/28/what-opioid-use-disorder-costs-pennsylvania
- “We’re All Responsible For Our Opioid Reliance-Even Patients”. https://time.com/4446503/opioid-reliance-responsibility/
- “FDA approves painkiller designed to eliminate the risk of addiction associated with opioids”. https://apnews.com/article/b1dd4276fce3d88ff32e3062e95f408f
- “Purdue Pharma, Sacklers reach $7.4 billion national opioid settlement”. https://www.reuters.com/business/healthcare-pharmaceuticals/purdue-pharma-sacklers-reach-74-bln-national-opioid-settlement-2025-01-23/
- “5 alternative treatments for chronic pain | UCLA Health”. https://www.uclahealth.org/news/article/5-alternative-treatments-chronic-pain
- “Exercise May Help You Better Tolerate Pain”. https://time.com/6283513/exercise-improves-pain-tolerance/
- “Health Rounds: Acupuncture reduces leg pain from a herniated disk”. https://www.reuters.com/business/healthcare-pharmaceuticals/health-rounds-acupuncture-reduces-leg-pain-herniated-disk-2024-10-25/
- “Helping patients cope with chronic non-malignant pain: it’s not about opioids – BPJ63 September 2014”. https://bpac.org.nz/BPJ/2014/September/chronicpain.aspx
- “Pharmacological Methods of Pain Management: Narrative Review of Medication Used – PMC”. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10402723/
- “Complementary Health Approaches for Chronic Pain: What the Science Says | NCCIH”. https://www.nccih.nih.gov/health/providers/digest/complementary-health-approaches-for-chronic-pain-science
- “Nonopioid Treatments for Chronic Pain—Integrating Multimodal Biopsychosocial Approaches to Pain Management | Guidelines | JAMA Network Open | JAMA Network”. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2793231
- “The Multidisciplinary Team in Pain Management – PubMed”. https://pubmed.ncbi.nlm.nih.gov/35718393/
- “Effectiveness of Virtual Reality-Based Interventions for Managing Chronic Pain on Pain Reduction, Anxiety, Depression and Mood: A Systematic Review – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC9602273/
- “Transcranial magnetic stimulation for the treatment of chronic low back pain: a narrative review – PubMed”. https://pubmed.ncbi.nlm.nih.gov/37213707/
- “Virtual Reality Therapy Emerges for Chronic Pain Management”. https://advancementsinpainmanagement.com/therapeutic-care/intervention-strategies/exploring-impact-virtual-reality-therapy-chronic-pain-management/
- “Multimodal non-invasive non-pharmacological therapies for chronic pain: mechanisms and progress – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC10542257/