
What is Ovarian Pain?
Ovarian pain or discomfort, such as ovarian pain while sneezing, can be frightening and have a number of underlying causes. We’ll be discussing possible causes of pain, including both ovarian and pelvic pain, as well as diagnosis and management.
The female reproductive system contains two tiny, almond-shaped structures called ovaries that are placed on either side of the uterus. They are essential for the development of eggs, their release for fertilization, and the secretion of hormones including progesterone and estrogen.1
Ovulation is one potential reason for ovarian pain when sneezing. The release of an egg into the fallopian tube for fertilisation is known as ovulation. Around the middle of the menstrual cycle, this process normally happens once a month. The ovaries swell and may become more sensitive or uncomfortable during ovulation, particularly if there are any ovarian cysts present. The ovaries may feel uncomfortable or painful as a result of coughing, sneezing, or any other physical action that puts pressure on the abdomen region.2
Endometriosis
Endometriosis is another potential reason why ovarian discomfort occurs when you sneeze. It is a condition where tissue normally grows on the ovaries, fallopian tubes, or the lining of the pelvis instead of inside the uterus. Extreme pelvic pain can result from it, particularly when menstruating or having sex. Due to the increased strain on the pelvic region, sneezing may also induce discomfort in the ovary region in endometriosis-affected women.3
Polycystic Ovary Syndrome (PCOS)
Ovarian pain while sneezing can also have other probable causes, including polycystic ovary syndrome (PCOS). PCOS is a hormonal condition that affects women who are fertile. Many tiny ovarian cysts, irregular menstruation, painful periods, and hormonal abnormalities are its defining features. Ovarian sensitivity and tenderness may increase due to the hormonal abnormalities brought on by PCOS, which may cause pain or discomfort when sneezing or engaging in other physical activities.4
Pelvic Inflammatory Disease (PID)
Another possible reason for ovarian pain while sneezing is pelvic inflammatory disease (PID). PID is a bacterial infection of the female reproductive system that is frequently brought on by STIs like gonorrhea and chlamydia. PID can cause excruciating abdominal pain and harm to the fallopian tubes, which can prevent conception. If PID is present, sneezing or a cough may produce discomfort or pain near the ovary.5
Multiple Causes of Ovarian Pain
All in all, there are a variety of underlying causes for ovaries that hurt or are uncomfortable while sneezing, from ovulation, and round ligament pain, to more serious problems like endometriosis or PID. If the discomfort is severe or persistent, or if additional symptoms like a fever or vaginal bleeding are present, it is crucial to see a doctor. A thorough medical examination can assist in determining the underlying cause and the best course of action for treating the symptoms and averting consequences.1
What is Pelvic Pain?
It’s normal for women to feel pain or discomfort in their pelvic area while performing certain physical activities, like sneezing. This is because sneezing can create a sudden rise in pressure in the abdominal and pelvic regions, which may result in ovarian pain or discomfort.
If the pelvic floor muscles are not working properly, it is not uncommon for people to suffer from bladder leakage during activities that exert pressure on the pelvic region, including laughing, coughing, sneezing, or lifting heavy objects. Healthy individuals have pelvic floor muscles that contract effectively, but those with weakened pelvic floor muscles or pelvic floor dysfunction may not be able to contract them promptly and as a result, be experiencing pelvic pain.
The pelvic floor muscles tend to relax more effectively with deep breathing, which allows the diaphragm to descend and reduces tension throughout the abdomen and pelvis. However, something as small as sniffles require you to take short and shallow breaths, which keeps the pelvic floor muscles in a constant state of tension, which can cause symptoms such as poor digestion, sleep difficulties, and pain that are unrelated to the illness or injury causing the sniffles.6
Acute vs Chronic Pain
Acute pelvic pain is sudden and severe, while chronic pain lasts for months or more, either continuously or in reoccurring episodes. Chronic pelvic pain is defined as pelvic discomfort that lasts more than six months and does not improve with treatment. The genitalia or other surrounding pelvic organs may be the cause of pelvic discomfort, or it may be psychological in origin. This may result in increased pain perception or actual discomfort even in the absence of any physical problems.7
Causes of Pelvic Pain
There are numerous factors that can lead to pelvic pain, including:8
- Acute appendicitis.
- Bladder pain can be due to disorders like urinary tract infections.
- Sexually transmitted infections.
- Kidney infection or kidney stones.
- Intestinal disorders such as diverticulitis or colitis.
- Nerve conditions, including pinched nerves of your spine.
- Hernia.
- Pelvic disorders like tightness and spasms of pelvic muscles.
- Broken pelvic bones.
- Psychogenic pain is caused by stress or past psychological traumas.
It is also worthwhile to note that damage to or dysfunction of the nervous system can result from inflammation or direct irritation of nerves due to injury, fibrosis, pressure, or intraperitoneal inflammation. This can cause neuropathic pain, a type of chronic pain.7
Unique Consideration for Women
In women and that assigned female at birth, possible causes of pelvic pain may also include:8
- Pregnancy.
- Ectopic pregnancy.
- Miscarriage.
- Pelvic inflammatory disease (PID).
- Ovulation.
- Menstrual cramps.
- Ovarian cysts or other ovarian disorders.
- Uterine fibroids.
- Endometriosis.
- Cervical, uterine, or ovarian cancer.
Symptoms of Pelvic Pain
Pelvic pain can be associated with additional symptoms or indications. The following are some of the most typical symptoms that accompany pelvic pain:7
- Vaginal bleeding, spotting, or discharge
- Menstrual pain
- Dysuria (painful urination)
- Constipation or diarrhea
- Bloating or flatulence
- Rectal bleeding (bleeding while passing stool)
- Painful intercourse
- Fever or chills
- Hip pain
- Groin area pain
Identifying the degree of pelvic pain is crucial, and if symptoms are severe, getting medical emergency help is advised. It’s crucial to get emergency medical help if your pelvic pain is severe, abrupt, or intense if you can’t stand up straight because of it, if there is blood in your stool or urine, if you’re feverish, or if you’ve just become pregnant. 7 A visit to a healthcare professional is also advised if your pelvic pain persists for longer than two weeks as this could be a sign of a significant underlying condition.
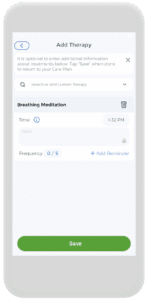
Symptoms that you experience can be tracked using the CareClinic App!
Severe Pelvic Pain
Among these factors, the prevalent origins of sudden and severe pain, such as severe abdominal pain, include:7
- Ectopic pregnancy (a pregnancy that occurs outside the uterus)
- Pelvic inflammatory disease (or PID, which is an infection of the reproductive organs)
- Ruptured or twisted ovarian cyst
- Miscarriage or imminent miscarriage
- Urinary tract infection
- Appendicitis
- Ruptured fallopian tube
Additional causes of acute pelvic pain could be linked to issues in the digestive tract (e.g. inflammatory bowel disease like Crohn’s disease), urinary tract, or nervous system.
In addition to being a symptom of digestive or urinary tract infections, pelvic organ abnormalities can also cause pain in the lower abdomen. Pelvic discomfort can have a variety of potential reasons, so it’s crucial to speak with a healthcare professional to get a proper diagnosis and course of treatment.7

How is Pelvic Pain Diagnosed?
To determine the cause of pelvic pain, your healthcare provider might ask about the following:7
- When and where does the pain occur?
- How long does the pain persist?
- Is the pain linked to your menstrual cycle, urination, or sexual activity?
- What kind of pain is it (e.g. sharp pain or dull pain/ stabbing pain)?
- Under what circumstances did the pain begin?
- How suddenly did the pain start?
Also, additional information regarding the time of the pain and the existence of other symptoms connected to activities like eating, resting, having sex, and moving around will help your healthcare provider make a diagnosis.
Pelvic Pain Tests
Determining the origin of pelvic pain may require an evaluation of symptoms and medical records, as well as a physical examination or other diagnostic tests. Blood tests, pregnancy tests, urinalyses, vaginal or penile cultures for STDs, abdominal and pelvic X-rays, laparoscopies, hysteroscopies, stool sample analysis, lower endoscopies, ultrasounds, and CT scans of the abdomen and pelvis are some of the tests that may be performed. These examinations can aid in locating anomalies or diseases such as endometrial growths, inflammation, infections, or irregular growths in the colon or rectum.7
Investigations
This is a list of possible investigations that may be carried out to determine the cause of your pain:7
- Blood and urine tests, including pregnancy tests in reproductive-age individuals.
- Vaginal or penile cultures to screen for sexually transmitted infections like gonorrhea and chlamydia.
- Ultrasound, which uses high-frequency sound waves to produce images of internal organs.
- Computed tomography (CT or CT scan), is a type of imaging test that creates detailed images of the body using X-rays and a computer.
- Magnetic resonance imaging (MRI), is a non-invasive procedure that generates two-dimensional images of internal organs or structures.
- Laparoscopy, a tiny tube with a lens and light (laparoscope) is put into an incision in the abdominal wall to inspect the pelvic region and find any endometrial growths during laparoscopy, a minor surgical procedure.
- X-ray is a method that uses electromagnetic energy to create images of bones and internal organs.
- Colonoscopy, with the use of a colonoscopy, a doctor can visually inspect the length of a patient’s large intestine to look for abnormal growths, inflammatory tissue, ulcers, and bleeding. The colon is examined with a colonoscope, a long, flexible tube with a light, which is introduced into the rectum.
- Sigmoidoscopy, a diagnostic procedure that examines the interior of a portion of the large intestine using a short, flexible, lighted tube (sigmoidoscope) inserted through the rectum, which inflates the intestine to facilitate viewing, helps determine the causes of diarrhea, constipation, abdominal pain, abnormal growths, and bleeding.
Treatment for Pelvic Pain
The reason, severity, and frequency of the discomfort are only a few variables that affect how pelvic pain is treated. Traditional methods for treating pelvic pain include medicine, which may include antibiotics if necessary, surgery, or other medical interventions if the problem is with one of the pelvic organs. Another viable choice for some people is physical therapy. It can be difficult and emotionally taxing to manage persistent pelvic pain. According to research, many people find it beneficial to speak with a licensed therapist, physical therapist, psychologist, or psychiatrist.7 Further information on pelvic pain treatments that are available can be obtained from your healthcare professional.
At-Home Pain Management
There are various self-care techniques you can use if you have persistent pelvic pain to reduce symptoms.7 For instance:
- Utilize over-the-counter painkillers. The inflammation that causes pelvic pain can be reduced with the help of nonsteroidal anti-inflammatory drugs (NSAIDs), such as naproxen sodium or ibuprofen. Acetaminophen might also assist in easing uncomfortable feelings.
- Make time for exercise in your schedule. Even though it could be difficult to move, exercise can improve blood flow and possibly lessen discomfort.
- Put warmth on. Take a soothing hot bath or apply a warm compress or heating pad to the affected area.
- Quit smoking. Products with nicotine can aggravate nerves and cause pain. Taking these things out of your routine may help with pain management.
- Practice relaxing strategies. Stress and tension can be reduced by exercises like yoga, meditation, or mindfulness, which may lessen the discomfort of chronic pain.
Exercises and other activities, such as meditation, can all be easily tracked using the CareClinic App!

Treatment Considerations
Depending on the underlying cause of your pelvic discomfort, many treatment modalities exist.9 Your healthcare professional will go over the available alternatives with you based on the following considerations:
- Your general well-being and medical background
- The severity of your condition
- Underlying causal factors
- Your capacity to withstand particular treatments, therapies, or techniques
- The expected progression of the ailment
- Your individual choices or beliefs
If a medical cause of your pelvic pain cannot be found, your doctor may advise psychotherapy to help you deal with the persistent pain. As an alternative, healthcare professionals could advise a multidisciplinary approach to treatment that incorporates several tactics like changing your nutrition, your environment, getting physical therapy, and using pain management approaches.9
Understanding Chronic Pelvic Pain (CPP)
Due to the complexity of the condition and the variety of anatomical structures and causes associated with pelvic discomfort, a thorough and gender-specific examination is recommended. It’s important to analyze patients from multiple perspectives. There is thought to be a connection between central nervous system alterations and chronic pelvic pain, specifically altered activity of the hypothalamic-pituitary-adrenal axis and autonomic nervous system. 10 Psychological distress also plays a role in pelvic discomfort. Chronic pelvic pain has been linked to psychosocial factors, like heightened pain sensitivity, stress, personality traits, social factors, melancholy, anxiety, trauma-related illnesses, somatization, and substance misuse.10 Therefore, when treating persistent pelvic pain, it is always important to take psychosocial variables into account.
Treatment and Rehabilitation
Conservative interventions such as education, medication, psychotherapy, exercise, or physical therapy should be included in the treatment of pelvic pain. Interventional and surgical techniques could be considered when less invasive therapies don’t work. Ablative techniques, sacral neuromodulation, neurolysis, hysterectomy, vulvar or vestibular surgery, resection, and prostatectomy are a few examples of these techniques.11
Patient Education, Diet Change and Behavioural Treatment
You may find relief from symptoms with the use of behavioural therapy, which includes scheduled urination and restricted fluid consumption. Stress management techniques, patient education initiatives, and support groups can all be helpful. Furthermore, it is advised to keep a bladder diary and adhere to a diet plan that excludes acidic beverages, coffee, tea, overly-fattening, spicy, and gas-producing foods, as well as large quantities, of alcohol, and artificial sweeteners. Probiotics are advised together with dietary changes in cases of gastrointestinal diseases including irritable bowel syndrome.12
Pharmacological Treatment
Pharmacotherapy for CPP should be tailored to the source of discomfort. Depending on the illness, different drugs are employed, including NSAIDs, hormonal therapies, opioids, antidepressants, anticonvulsants, alpha-blockers, and antibiotics. With CPP, neuropathic pain management is essential. Anticonvulsants like gabapentin and pregabalin were found to be useful in the treatment of 119 CPP patients.13 A different study found that when it came to treating CPP, gabapentin outperformed amitriptyline.14 Pregabalin may or may not be ineffective in individuals with chronic prostatitis, according to a systematic review, but more research is needed to make this claim.15
Physiotherapy and Rehabilitation
Physiotherapy and rehabilitation have been shown to be effective in treating CPP. Various methods, including exercise, manual therapy, and electrotherapy, can be used. Kegel exercises, posture, core stabilization, stretching, and strengthening should be included in rehabilitation programs. Additionally, percutaneous tibial nerve neuromodulation and interventional sacral neuromodulation have been shown to be effective in reducing pain and improving the quality of life in CPP patients. A recent meta-analysis found that PTNS was beneficial in treating chronic prostatitis/CPP, while sacral neuromodulation was effective in treating CPP.16
Injection Techniques in Pelvic Pain
Compression of joints, muscles, and nerves in the pelvic area can result in pain in the lower extremities or the back. The discomfort in this region can be treated with a variety of injections, including epidural injections, sacroiliac joint injections, facet joint injections, and myofascial trigger points and ligaments.17 By using ultrasonography (USG) or computed tomography (CT), injections can be guided to avoid sensitive anatomical structures.18
Interdisciplinary Approach
The management of CPP should emphasise interdisciplinary collaboration, according to a European Association of Urology guideline. Numerous medical specialists, including physiatrists, urologists, gynecologists, gastroenterologists, general surgeons, neurologists, psychiatrists, pain medicine doctors, physiotherapists, psychologists, and social workers, are involved in this.19 If you’re considering self-management, a complete strategy that combines medical, psychological, and sexual care is intended.20
References
- Schaefers-Okkens, A. C., & Kooistra, H. S. (2010). Ovaries. Clinical endocrinology of dogs and cats: an illustrated text, (Ed. 2), 203-234.
- “Pain in Your Ovaries.” Cleveland Clinic, my.clevelandclinic.org/health/symptoms/24726-ovary-pain. Accessed 8 Apr. 2023.
- Lebovic, D. I., Mueller, M. D., & Taylor, R. N. (2001). Immunobiology of endometriosis. Fertility and sterility, 75(1), 1-10.
- Azziz, R. (2004). PCOS: a diagnostic challenge. Reproductive biomedicine online, 8(6), 644-648.
- Brunham, R. C., Gottlieb, S. L., & Paavonen, J. (2015). Pelvic inflammatory disease. New England Journal of Medicine, 372(21), 2039-2048.
- Lawson, J. O. (1974). Pelvic anatomy. I. Pelvic floor muscles. Annals of the Royal College of surgeons of England, 54(5), 244.
- “Pelvic Pain.” hopkinsmedicine.org, www.hopkinsmedicine.org/health/conditions-and-diseases/pelvic-pain.
- “Pelvic Pain: Symptoms, Causes & Treatment.” Cleveland Clinic, my.clevelandclinic.org/health/symptoms/12106-pelvic-pain. Accessed 8 Apr. 2023.
- “How Is Pelvic Pain Treated?” Https://Www.nichd.nih.gov/, www.nichd.nih.gov/health/topics/pelvicpain/conditioninfo/treatments. Accessed 8 Apr. 2023.
- Vural M. Pelvic pain rehabilitation. Turk J Phys Med Rehabil. 2018 Nov 4;64(4):291-299. doi: 10.5606/tftrd.2018.3616.
- Cohen, S. P. (2017). Essentials of Pain Medicine. Elsevier-Health Sciences Division.
- Bharucha, A. E., Chakraborty, S., & Sletten, C. D. (2016, August). Common functional gastroenterological disorders associated with abdominal pain. In Mayo Clinic Proceedings (Vol. 91, No. 8, pp. 1118-1132). Elsevier.
- Agarwal, M. M., & Elsi Sy, M. (2017). Gabapentenoids in pain management in urological chronic pelvic pain syndrome: Gabapentin or pregabalin?. Neurourology and urodynamics, 36(8), 2028-2033.
- Cheong, Y. C., Smotra, G., & de C Williams, A. C. (2014). Non‐surgical interventions for the management of chronic pelvic pain. Cochrane Database of Systematic Reviews, (3).
- Aboumarzouk, O. M., & Nelson, R. L. (2012). Pregabalin for chronic prostatitis. Cochrane database of systematic reviews, (8).
- Vural, M., & Karan, A. (2016). Physical Therapy and Rehabilitation in Urogynecology.
- Elkins, N., Hunt, J., & Scott, K. M. (2017). Neurogenic pelvic pain. Physical Medicine and Rehabilitation Clinics, 28(3), 551-569.
- Domingo-Rufes, T., Bong, D. A., Mayoral, V., Ortega-Romero, A., Miguel-Pérez, M., & Sabaté, A. (2013). Ultrasound-guided pain interventions in the pelvis and the sacral spine. Techniques in Regional Anesthesia and Pain Management, 17(3), 107-130.
- Engeler, D. S., Baranowski, A. P., Dinis-Oliveira, P., Elneil, S., Hughes, J., Messelink, E. J., … & Williams, A. C. (2013). The 2013 EAU guidelines on chronic pelvic pain: is management of chronic pelvic pain a habit, a philosophy, or a science? 10 years of development. European urology, 64(3), 431-439.
- Bornstein, J., Goldstein, A. T., Stockdale, C. K., Bergeron, S., Pukall, C., Zolnoun, D., … & International Society for the Study of Vulvovaginal Disease (ISSVD). (2016). 2015 ISSVD, ISSWSH, and IPPS consensus terminology and classification of persistent vulvar pain and vulvodynia. The journal of sexual medicine, 13(4), 607-612.
References
- “Ovarian cyst”. https://en.wikipedia.org/wiki/Ovarian_cyst
- “Ovarian torsion”. https://en.wikipedia.org/wiki/Ovarian_torsion
- “Ovarian vein syndrome”. https://en.wikipedia.org/wiki/Ovarian_vein_syndrome
- “What causes pelvic pain? | NICHD – Eunice Kennedy Shriver National Institute of Child Health and Human Development”. https://www.nichd.nih.gov/health/topics/pelvicpain/conditioninfo/causes
- “Pelvic Pain: Causes, Symptoms, Treatment & Relief”. https://my.clevelandclinic.org/health/symptoms/12106-pelvic-pain
- “How is pelvic pain diagnosed? | NICHD – Eunice Kennedy Shriver National Institute of Child Health and Human Development”. https://www.nichd.nih.gov/health/topics/pelvicpain/conditioninfo/diagnosed
- “Diagnosing Pelvic Pain | NYU Langone Health”. https://nyulangone.org/conditions/pelvic-pain/diagnosis
- “Pelvic Pain: Diagnosis & Treatment | NewYork-Presbyterian”. https://www.nyp.org/womens/general-gynecology/pelvic-pain/treatment
- “Chronic Pelvic Pain in Women: ACOG Updates Recommendations | AAFP”. https://www.aafp.org/pubs/afp/issues/2021/0201/p186.html
- “Evaluation and Medical Management of Chronic Pelvic Pain – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC10415055/
- “Approach to diagnosis and management of chronic pelvic pain in women: incorporating chronic overlapping pain conditions in assessment and management – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC9297339/
- “Chronic Pelvic Pain: A Comprehensive Guide – Ask The Nurse Expert”. https://askthenurseexpert.com/chronic-pelvic-pain-a-comprehensive-guide/
- “How is pelvic pain treated? | NICHD – Eunice Kennedy Shriver National Institute of Child Health and Human Development”. https://www.nichd.nih.gov/health/topics/pelvicpain/conditioninfo/treatments
- “How to manage persistent pelvic pain | Jean Hailes for… | Jean Hailes”. https://www.jeanhailes.org.au/health-a-z/persistent-pelvic-pain/what-you-can-do
- “A multidisciplinary approach to self care in chronic pelvic pain”. https://pubmed.ncbi.nlm.nih.gov/17353816/
- “Central changes associated with chronic pelvic pain and endometriosis – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC4501205/
- “Autonomic Nervous System Dysfunction Is Related to Chronic Prostatitis/Chronic Pelvic Pain Syndrome – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC10782122/
- “Mental disorders in patients with chronic pelvic pain syndrome (CPPS) – PubMed”. https://pubmed.ncbi.nlm.nih.gov/28554368/


