Are you struggling with both Irritable Bowel Syndrome (IBS) and acne? Can IBS cause acne problems? You may be surprised to learn that these seemingly unrelated conditions could be connected. In recent years, researchers have been increasingly exploring the link between IBS and healthy skin.
In this article, we will delve into the fascinating world of gut-skin interactions and discuss how managing your IBS can potentially improve your skin health. So, let’s get started!
Understanding Irritable Bowel Syndrome (IBS)
If you’ve been diagnosed with IBS, you’re not alone. This common gastrointestinal disorder affects millions of people worldwide. But what exactly is IBS? IBS is characterized by a variety of symptoms, including abdominal pain, bloating, diarrhea, and constipation. These symptoms can vary in severity and frequency from person to person, making IBS a complex condition to manage.
What is IBS?
IBS is a functional disorder, which means that there are no structural abnormalities or visible signs of disease in the digestive tract. Instead, IBS is thought to be caused by a combination of factors, including abnormal gut motility, increased sensitivity to pain, and disturbances in the communication between the brain and gut.
Common Symptoms of IBS
The most common symptoms of IBS include:
- Abdominal pain or discomfort
- Bloating and distension
- Changes in bowel habits (diarrhea, constipation, or alternating between the two)
- Excessive gas
These symptoms can significantly impact your quality of life, affecting everything from your daily activities to your emotional well-being.
Causes and Risk Factors of IBS
The exact causes of IBS are not yet fully understood. However, several factors are believed to contribute to the development of this condition:
- Abnormal gastrointestinal motility
- Sensitivity to certain foods such as oily fish
- Stress and emotional factors
- Changes in gut microbiota
While anyone can develop IBS, certain risk factors may increase your likelihood of developing this condition. These risk factors include a family history of IBS, female gender, and a history of mental health conditions.
It is important to note that IBS is a chronic condition, meaning that it is long-lasting and requires ongoing management. While there is no cure for IBS, there are various treatment options available to help alleviate symptoms and improve quality of life. These treatment approaches may include dietary changes, stress management techniques, medication, and alternative therapies such as acupuncture or probiotics.
Living with IBS can be challenging, but with the right support and management strategies, it is possible to lead a fulfilling life. It is important to work closely with your healthcare provider to develop an individualized treatment plan that addresses your specific symptoms and needs. Remember, you are not alone in this journey, and there are resources and support groups available to help you navigate the ups and downs of living with IBS.
The Connection Between Gut Health and Skin
Now, let’s explore the fascinating interplay between your gut health and your skin. You may be wondering how the digestive system and the skin are related, but the truth is, they share a close connection known as the gut-skin axis.
The Gut-Skin Axis: An Overview
The gut-skin axis refers to the bidirectional communication between the gut and the skin. This communication occurs through various pathways, including the immune system, the nervous system, and the endocrine system. Disruptions in this communication can lead to imbalances that may manifest as both gastrointestinal and dermatological symptoms.
But what exactly happens when there is a disruption in the gut-skin axis? Well, let’s dive a little deeper into the topic.
When there is inflammation in the gut, it can have a direct impact on the health of your skin. Inflammation plays a crucial role in both Irritable Bowel Syndrome (IBS) and many skin conditions, including acne. When your gut is inflamed, it can release inflammatory molecules that travel through your bloodstream and reach your skin, contributing to the development of acne lesions. This explains why individuals with IBS often experience flare-ups of acne during periods of gut inflammation.
The Role of Gut Microbiome in Skin Health
 Your gut is home to trillions of bacteria, collectively known as the gut microbiota. These bacteria play a vital role in various aspects of your health, including your skin. Imbalances in the gut microbiota, known as dysbiosis, can contribute to increased gut inflammation, impaired gut barrier function, and alterations in hormone levels, all of which can impact your skin health.
Your gut is home to trillions of bacteria, collectively known as the gut microbiota. These bacteria play a vital role in various aspects of your health, including your skin. Imbalances in the gut microbiota, known as dysbiosis, can contribute to increased gut inflammation, impaired gut barrier function, and alterations in hormone levels, all of which can impact your skin health.
But what exactly is dysbiosis and how does it affect your skin? Dysbiosis refers to an imbalance in the types and numbers of bacteria in your gut. This imbalance can occur due to factors such as a poor diet, stress, or the use of certain medications. When your gut microbiota is out of balance, it can lead to increased gut inflammation, which can then affect your skin health. Additionally, dysbiosis can impair the function of your gut barrier, allowing harmful substances to leak into your bloodstream and trigger inflammatory responses in your skin.
Furthermore, alterations in hormone levels can also occur as a result of dysbiosis. Hormones play a significant role in regulating various processes in your body, including those that affect your skin. Imbalances in hormone levels can lead to increased oil production, clogged pores, and inflammation, all of which can contribute to the development of skin conditions like acne.
So, as you can see, the connection between gut health and skin is a complex and intricate one. The gut-skin axis, inflammation, and the gut microbiota all play crucial roles in determining the health and appearance of your skin. By prioritizing your gut health through a balanced diet, stress management, and proper medication use, you can support a healthy gut-skin axis and promote radiant, glowing skin.
IBS and Acne: Is There a Link?
The relationship between IBS and acne is a topic of ongoing research. While the exact mechanisms linking these two conditions are not yet fully understood, several theories have been proposed.
The Science Behind IBS and Acne
One theory suggests that the gut-skin axis plays a role in connecting IBS and acne. As discussed earlier, inflammation and gut dysbiosis can contribute to the development of acne. Additionally, shared risk factors, such as stress and hormonal imbalances, may further contribute to the link between these two conditions.
Research has shown that the gut and the skin share a complex network of communication pathways. The gut microbiota, which consists of trillions of microorganisms residing in our digestive system, can influence various aspects of our health, including our skin. Imbalances in the gut microbiota, commonly seen in individuals with IBS, can lead to increased intestinal permeability, allowing toxins and inflammatory molecules to enter the bloodstream. This systemic inflammation can then manifest as acne on the skin.
IBS, Stress, and Acne: A Complex Relationship
Stress can have a profound impact on both IBS and acne. It is well-established that stress can worsen IBS symptoms, leading to increased abdominal pain and poor digestive health, altered bowel habits, and heightened intestinal inflammation. Similarly, stress can trigger or exacerbate acne by increasing sebum production and promoting inflammation in the skin. Managing stress levels, therefore, becomes crucial in addressing both IBS and acne.
Furthermore, chronic stress can disrupt the balance of the gut microbiota, leading to dysbiosis. This dysbiosis can further contribute to the development of both IBS and acne. Stress management techniques, such as mindfulness meditation, exercise, and adequate sleep, can help reduce stress levels and support a healthy gut-skin axis.
Hormonal Imbalances in IBS and Its Impact on Skin
Hormonal imbalances can also contribute to the development of both IBS and acne. For instance, fluctuations in certain hormones, such as cortisol and estrogen, can affect small intestinal bacterial overgrowth, increase gut permeability, and influence oil production in the skin. Maintaining hormonal balance through proper nutrition and stress management can help support both gut and skin health.
In women, hormonal fluctuations throughout the menstrual cycle can also influence the severity of IBS symptoms and acne breakouts. Estrogen, progesterone, and testosterone levels fluctuate during different phases of the menstrual cycle, potentially affecting gut function and skin health. Understanding these hormonal changes and working with healthcare professionals to manage them can be beneficial in addressing both IBS and acne.
Managing IBS to Improve Skin Health
 Now that we understand the intricate relationship between IBS and acne, let’s explore some strategies to help manage your IBS and potentially improve your skin health.
Now that we understand the intricate relationship between IBS and acne, let’s explore some strategies to help manage your IBS and potentially improve your skin health.
Living with Irritable Bowel Syndrome (IBS) can be challenging, but making certain dietary changes can make a significant difference in managing your symptoms and supporting skin health. Incorporating fiber-rich foods, such as fruits, vegetables, and whole grains, can promote regular bowel movements and support a healthy gut. These foods not only aid in digestion but also provide essential nutrients that contribute to overall skin health.
Avoiding trigger foods is another crucial aspect of managing IBS and improving skin health. Spicy foods, fatty foods, and caffeine are known to exacerbate IBS symptoms, and they can also have a negative impact on your skin. By eliminating these trigger foods from your diet, you may experience a reduction in both IBS symptoms and skin issues like acne.
When it comes to gut health and skin health, the role of probiotics cannot be overlooked. Taking probiotic supplements or consuming fermented foods, like yogurt and sauerkraut, can help restore a healthy balance of gut bacteria. This, in turn, may improve digestion, reduce IBS symptoms, and potentially lead to clearer, healthier skin.
Importance of Stress Management in IBS and Acne
Reducing stress levels is crucial for managing both IBS and acne. Stress has been linked to the exacerbation of IBS symptoms and the onset of acne breakouts. Therefore, incorporating stress management techniques into your daily routine is essential for overall well-being.
Regular physical exercise is not only beneficial for your physical health but also for your mental well-being. Engaging in activities like yoga or brisk walks can help reduce stress levels and promote a sense of calm. Additionally, exercise stimulates the release of endorphins, which are known as “feel-good” hormones that can contribute to a healthier complexion.
Practicing relaxation techniques, such as deep breathing exercises or meditation, can help calm your mind and body. These techniques promote a state of relaxation, reducing stress and its negative impact on both your gut and your skin. Incorporating these practices into your daily routine can lead to significant improvements in both IBS symptoms and skin issues.
Adequate sleep plays a vital role in stress management and overall health. Lack of sleep can increase stress levels, leading to worsened IBS symptoms and skin issues. By prioritizing quality sleep and establishing a consistent sleep routine, you can support your body’s natural healing processes and promote healthier skin.
Medical Treatments and Therapies for IBS and Acne
If lifestyle modifications alone are not sufficient, various medical treatments and therapies are available for managing both IBS and acne. It’s essential to consult with your healthcare provider to determine the most appropriate treatment options for your specific needs.
For IBS, your healthcare provider may prescribe medications to help alleviate symptoms such as abdominal pain, bloating, and irregular bowel movements. Additionally, they may recommend therapies such as cognitive-behavioral therapy (CBT) or hypnotherapy, which have shown promising results in managing IBS symptoms.
When it comes to acne, dermatological treatments can be highly effective in improving skin health. Your dermatologist may recommend topical treatments, oral medications, or procedures such as chemical peels or laser therapy to target acne and promote clearer skin.
While the link between IBS and acne is still being explored, evidence suggests that there may indeed be a connection. By understanding and managing your IBS, you may be able to improve your skin health as well. Remember to make dietary changes, prioritize stress management, and discuss medical treatment options with your healthcare provider. Taking care of your digestive issues may just be the key to achieving healthier, clearer skin.
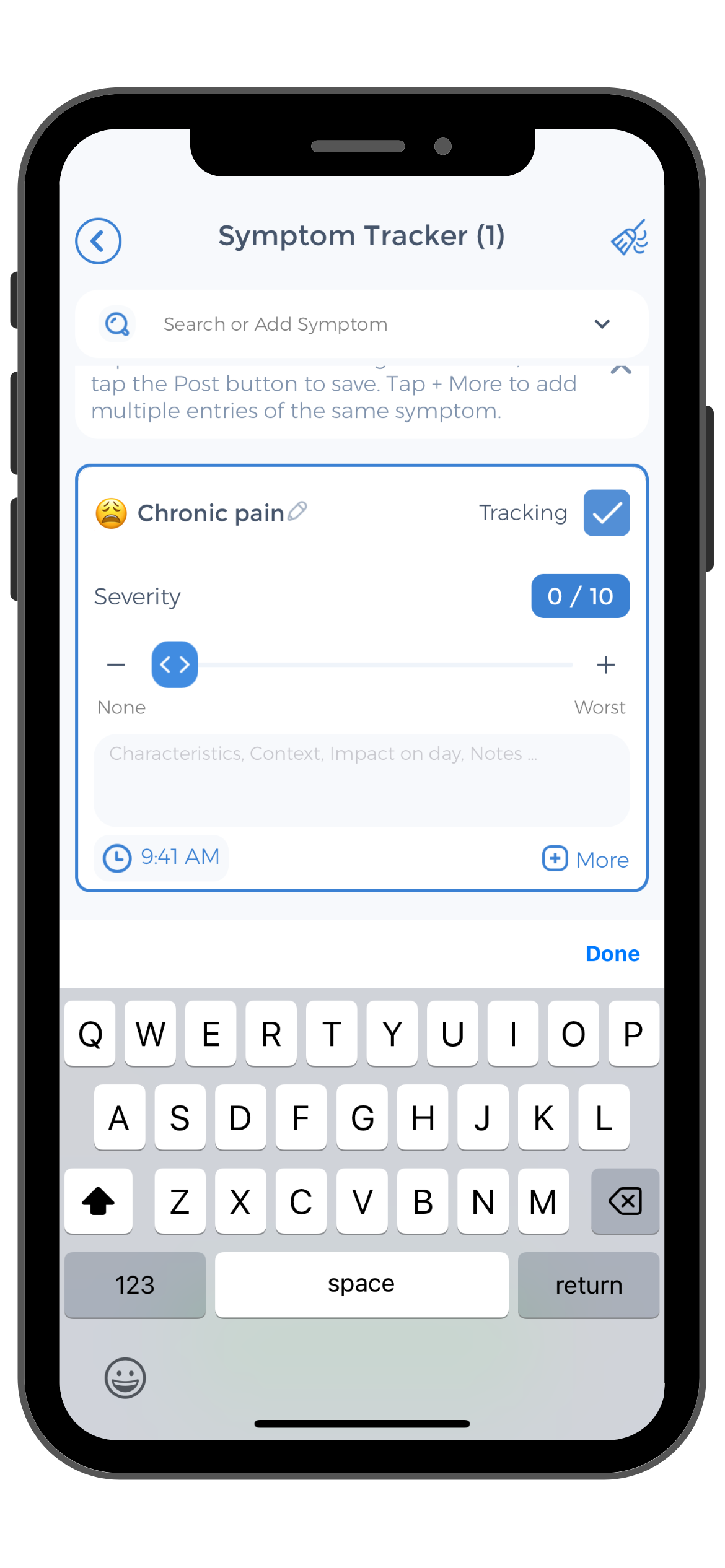
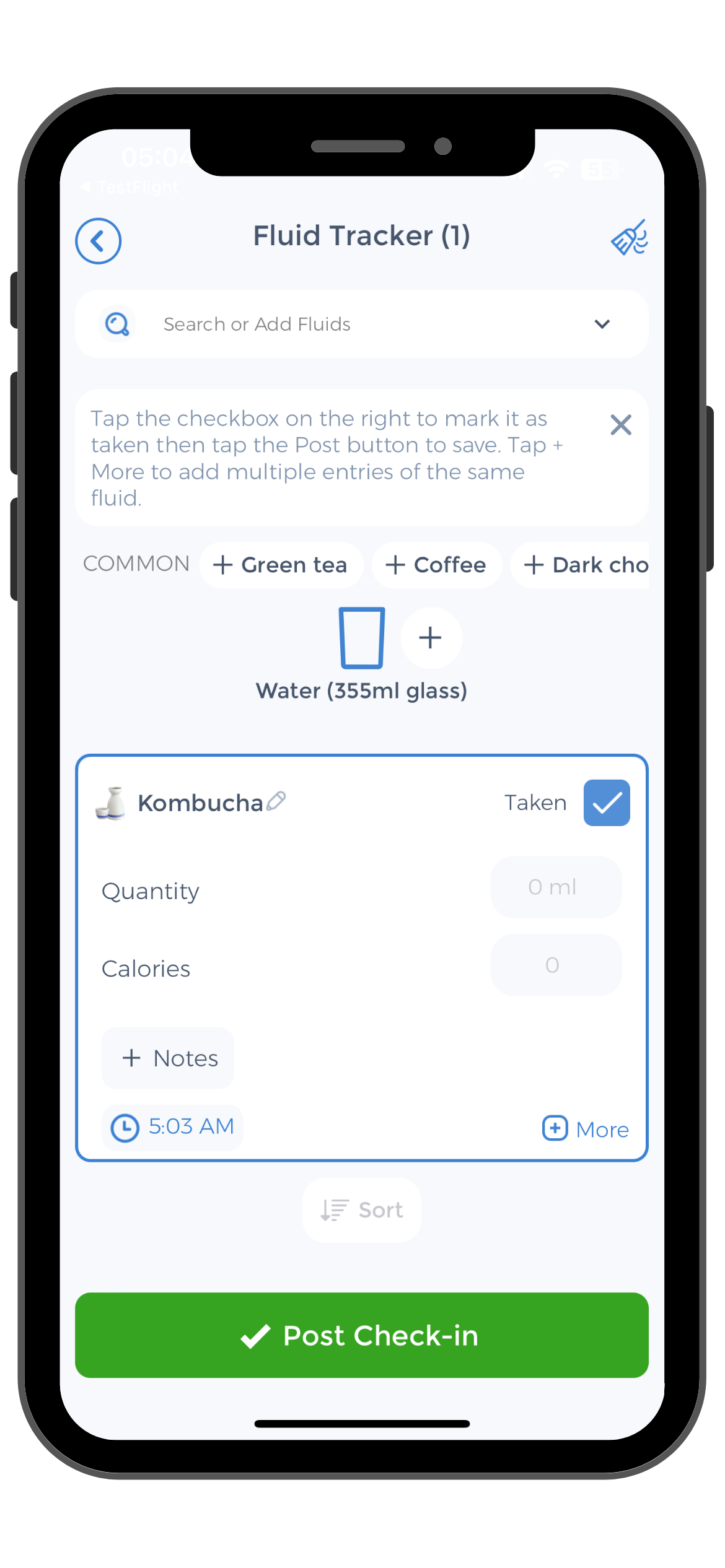
Use the CareClinic App to Manage IBS Symptoms
Managing IBS and its potential impact on skin health is made easier with the CareClinic App. By tracking your diet, stress levels, and symptoms, the app helps you identify patterns and triggers that may be contributing to both IBS and acne. The CareClinic App’s features include a symptom tracker, medication reminders, and a diary for logging food intake and stress management activities, providing a comprehensive approach to managing your health.
Download the CareClinic App Today
With the CareClinic App, you can expect to gain insights into how different aspects of your lifestyle affect your IBS and skin condition. This data-driven approach allows for more informed discussions with your healthcare provider, potentially leading to improved health outcomes. Take control of your IBS and skin health today by installing the CareClinic App.


