Stool Tracker
Track bowel movements, digestive patterns, and gut health with precision.
The best poop tracker app helps you log bowel movements daily, monitor stool patterns using the Bristol Stool Chart, and identify digestive triggers for optimal gut health. Whether tracking for IBS, Crohn’s disease, Ulcerative Colitis (UC), celiac disease, constipation, or general digestive wellness, our free bowel movement tracker app ensures every detail supports your health goals.
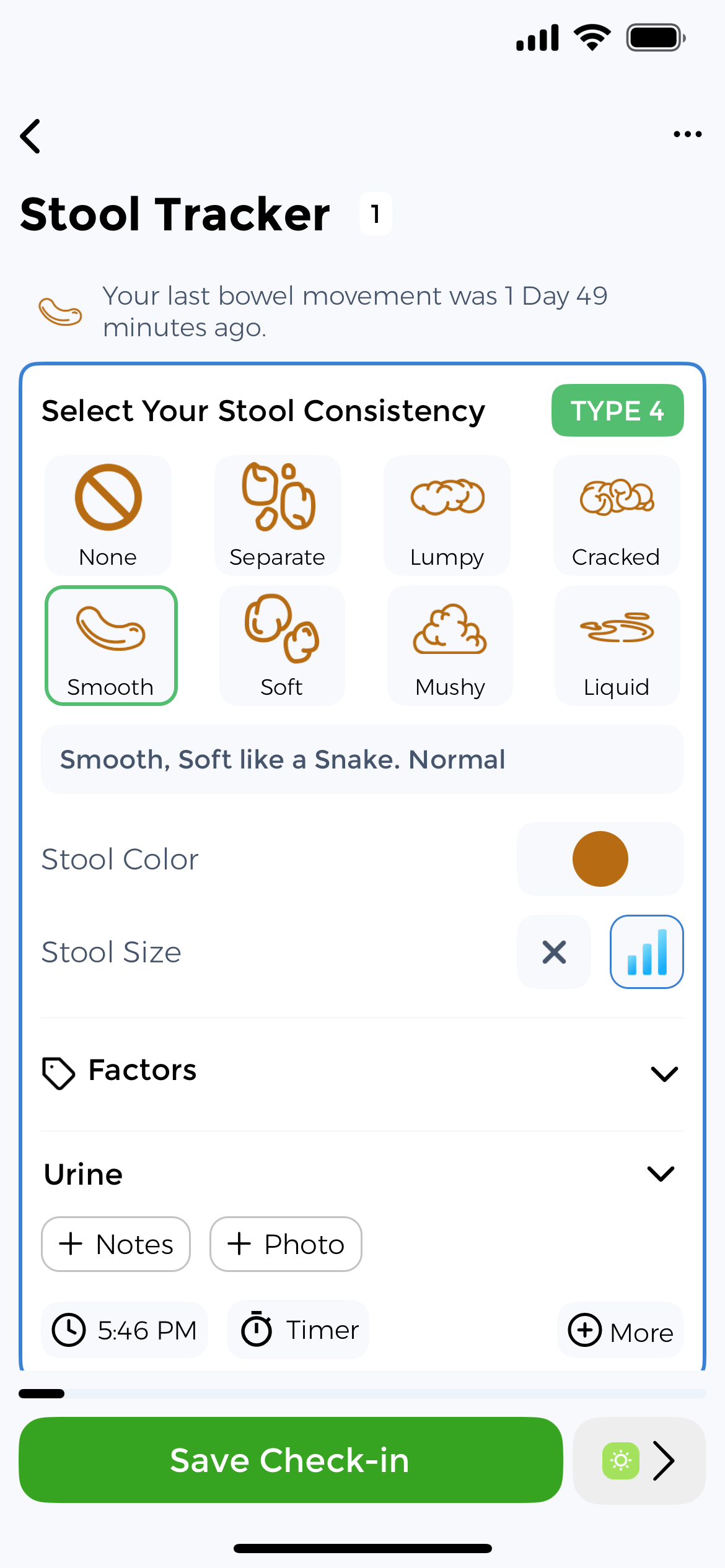
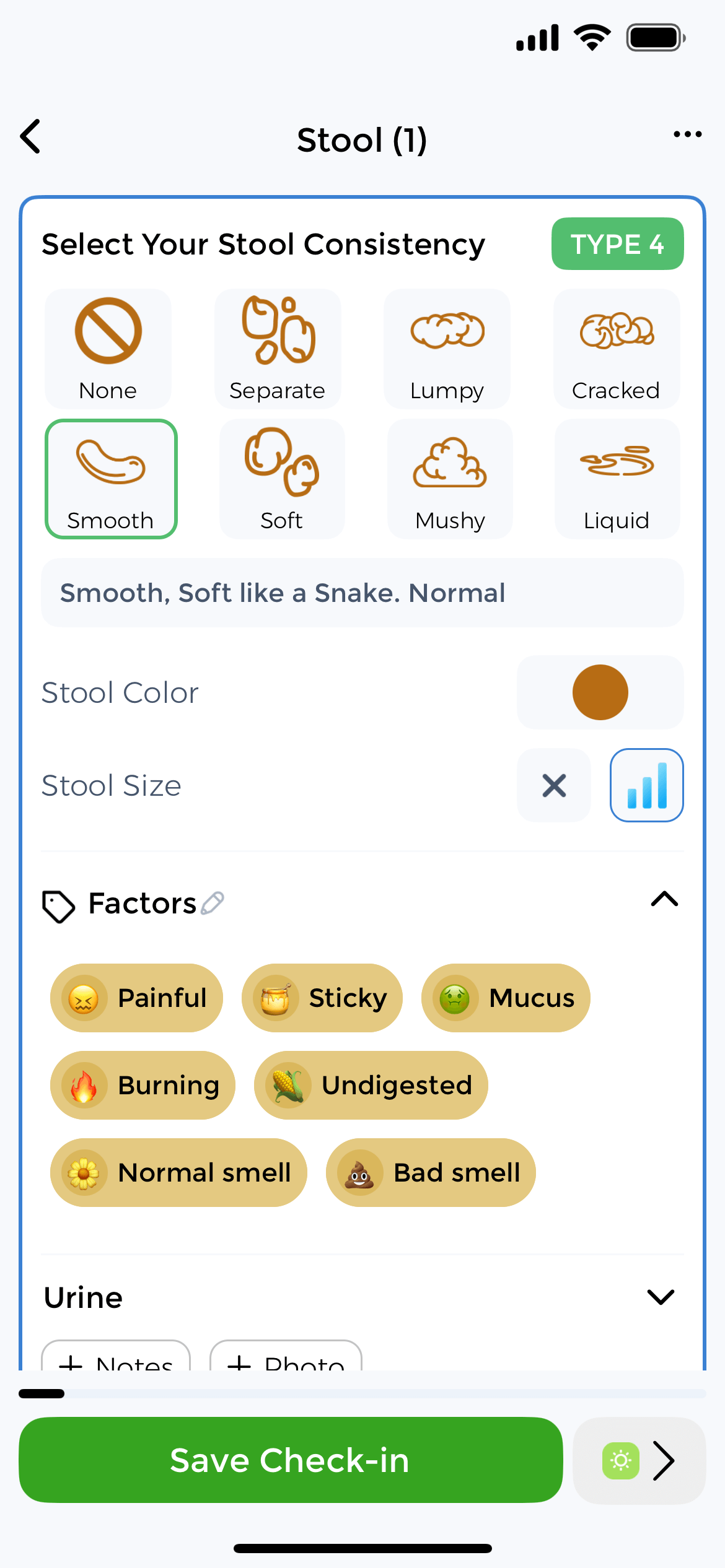
Track with Bristol Stool Chart
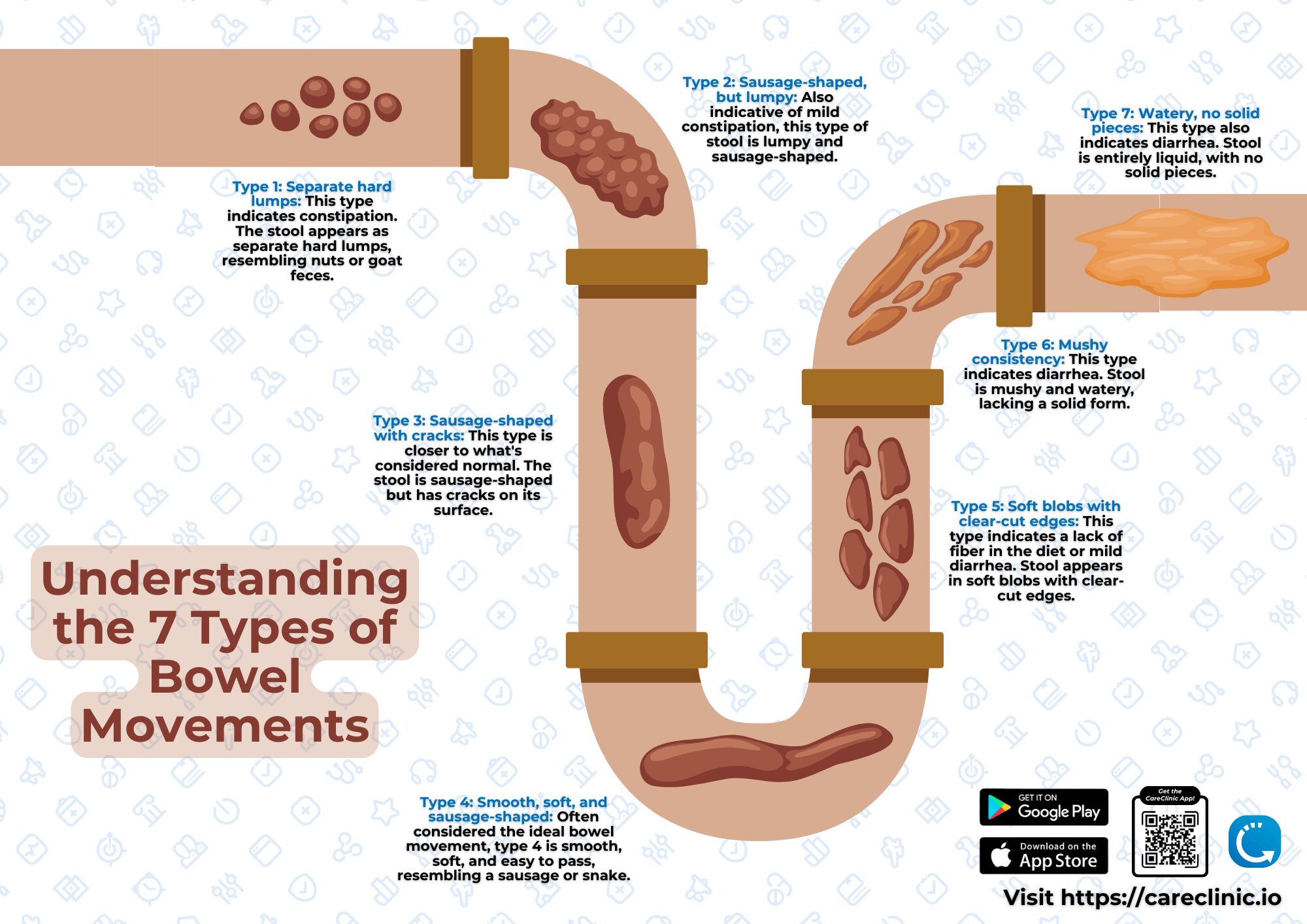
Understanding your digestive health starts with the Bristol Stool Scale, a clinically validated classification system used by gastroenterologists worldwide. This classification system provides standardized language for describing stool characteristics.
Our stool tracker app incorporates visual Bristol Scale references. You simply tap the type that matches your observation. Track consistency from Type 1 (constipation) to Type 7 (diarrhea) to identify your digestive baseline and spot concerning changes early. This bowel movement tracker app helps you log frequency, timing, color, and associated symptoms.
Identify Digestive Triggers
Here’s how digestive problems sneak up on you: gradual discomfort becomes your new normal. Before you know it, you’re planning life around bathroom access. This bowel tracking app catches these shifts early. This is crucial when 14.1% of people globally have IBS.
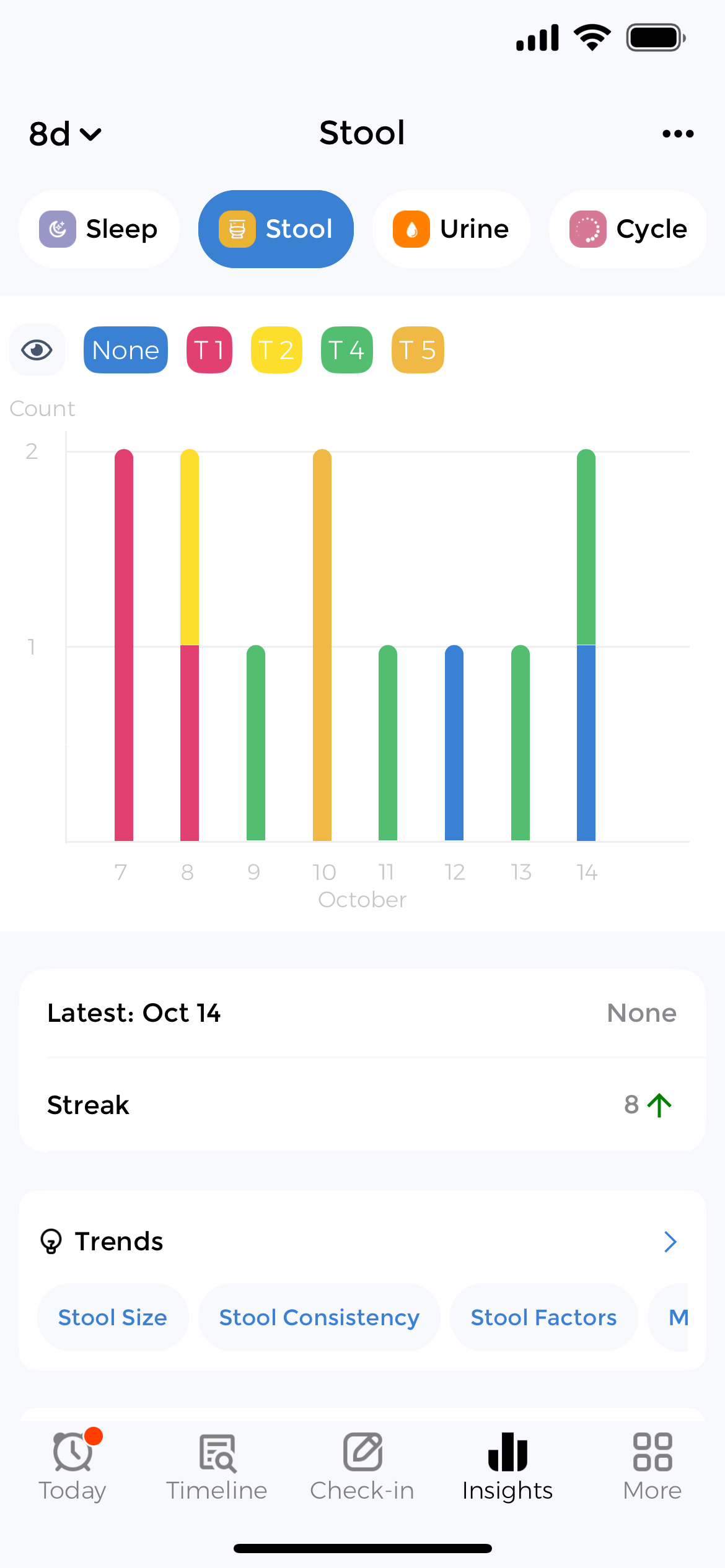
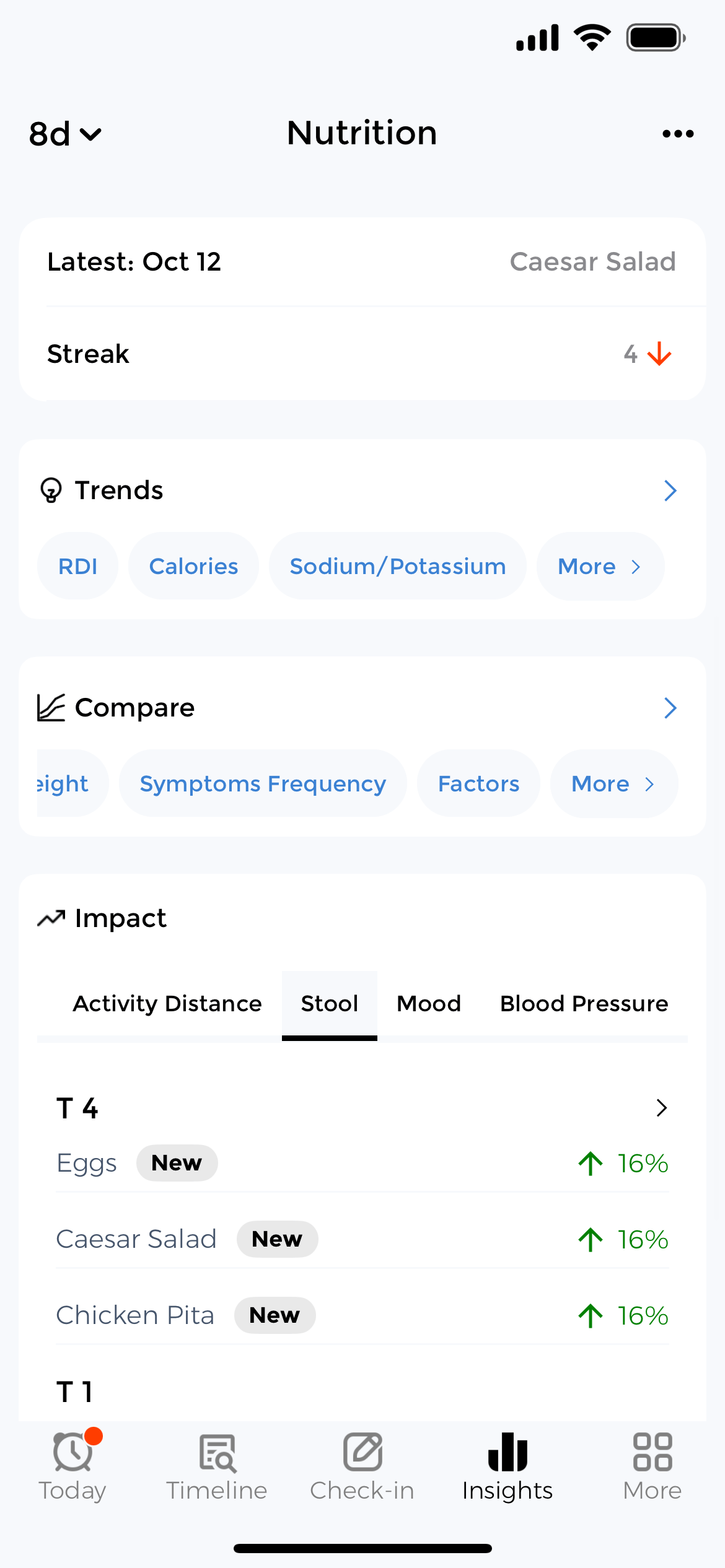
Without symptom logs in your poop diary, you’re playing medical detective with faulty memory. The app reveals patterns: that bloating always hits Tuesday, or pain spikes during stress. Track foods with the nutrition tracker, stress with the mood tracker, and correlate with bowel movements to identify triggers.
Your records become visual timelines that reveal what drives flare-ups or recovery. This poop tracking app turns daily symptom logs into real insights that improve your digestive care.
Track with Bristol Stool Chart
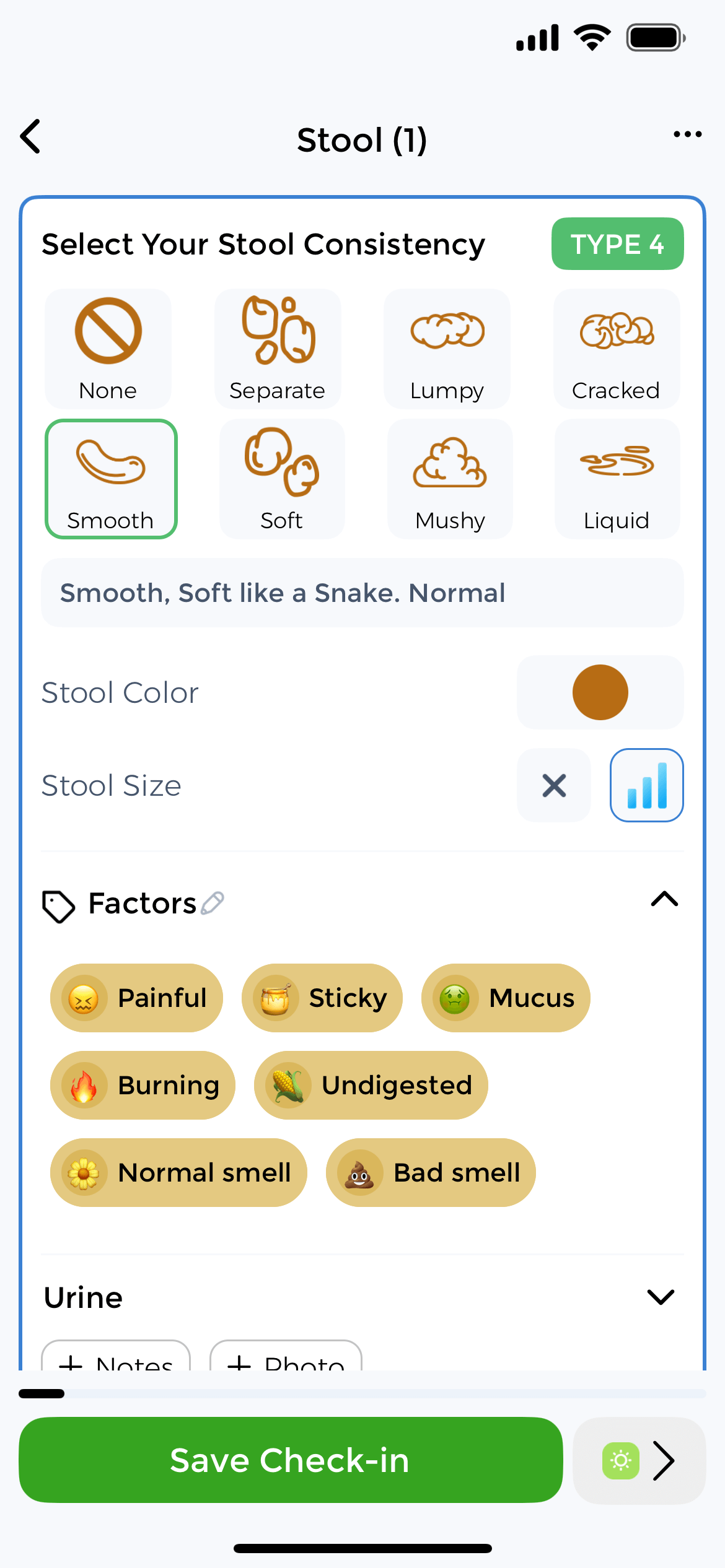
Our stool tracker app incorporates visual Bristol Scale references. You simply tap the type that matches your observation. Track consistency from Type 1 (constipation) to Type 7 (diarrhea) to identify your digestive baseline and spot concerning changes early. This bowel movement tracker app helps you log frequency, timing, color, and associated symptoms.
Identify Digestive Triggers
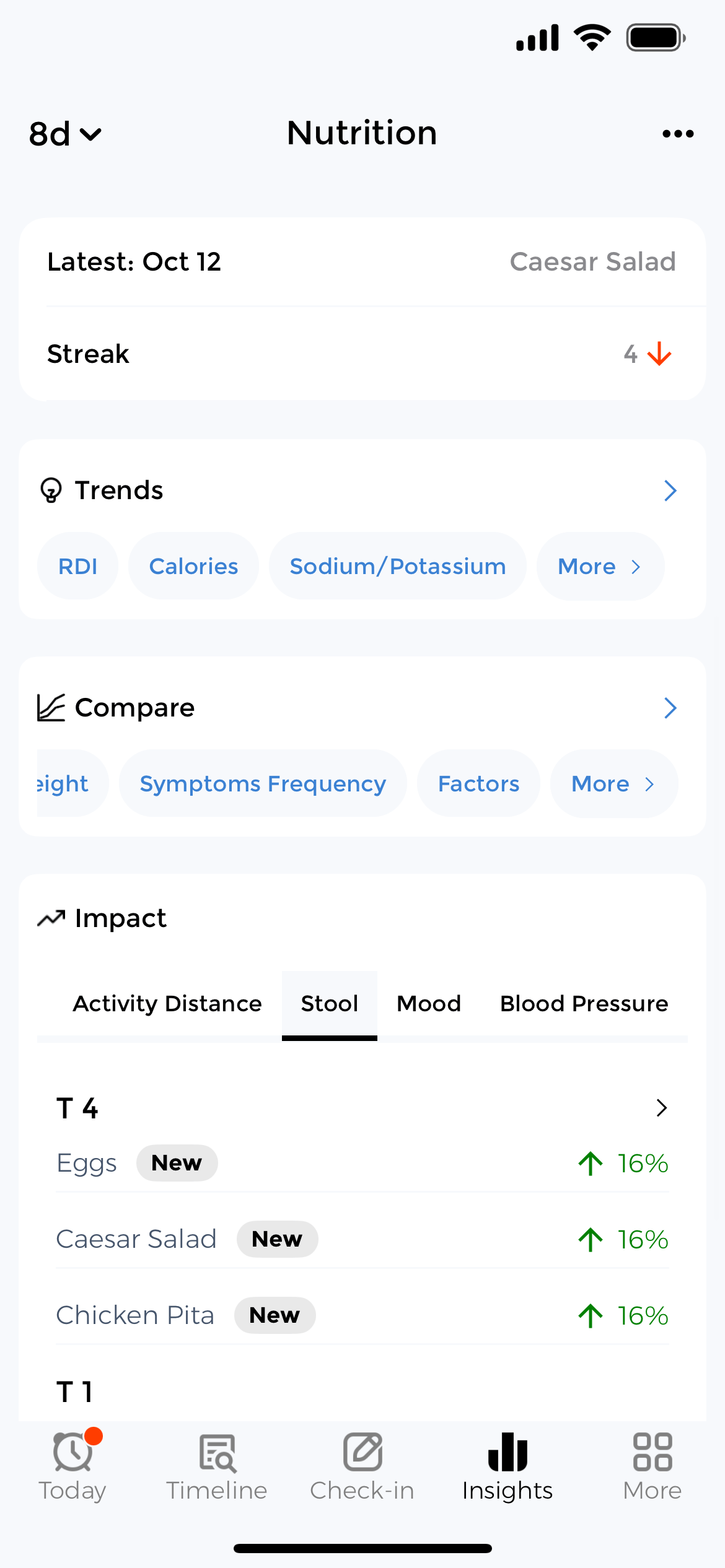
Without symptom logs in your poop diary, you’re playing medical detective with faulty memory. The app reveals patterns: that bloating always hits Tuesday, or pain spikes during stress. Track foods with the nutrition tracker, stress with the mood tracker, and correlate with bowel movements to identify triggers.
Your records become visual timelines that reveal what drives flare-ups or recovery. This poop tracking app turns daily symptom logs into real insights that improve your digestive care.
What to Track Daily
Effective bowel movement tracking extends beyond simple frequency counts. Your Tuesday morning espresso, yesterday’s takeout, that stressful presentation. Each influences tomorrow’s digestive reality. This stool tracker app helps you document these connections.
How the Bowel Movement Tracker Works
1. Log Your Movements
Open the app, select Bristol Stool type, add notes, and record symptoms. Logging takes under 30 seconds.
2. Track Patterns
After two weeks, view analytics showing common stool types, frequency patterns, and correlations with foods or stress.
3. Share with Doctor
Export visual reports for medical consultations. No more guesswork about symptom frequency or triggers.
Understanding the Bristol Stool Chart
Developed at Bristol Royal Infirmary, this classification system provides standardized language for describing stool characteristics. The poop analyzer app incorporates Bristol Scale visual references. You simply tap the type that matches your observation rather than struggling with descriptions. Clinical studies show the scale has strong reliability with an inter-rater agreement of 0.88 among gastroenterologists, making it the global standard for assessment in any bowel movement logger.
Types 1-2: Constipation
Type 1: Hard lumps. Severe constipation, 100+ hour transit. Often painful.
Type 2: Lumpy sausage. Mild constipation, 70-hour transit. May require straining.
Types 3-4: Ideal
Type 3: Sausage with cracks. Normal, 48-hour transit.
Type 4: Smooth soft sausage. Ideal, 24-48 hour transit. This is your target.
Types 5-7: Diarrhea
Type 5: Soft blobs. Borderline loose from food intolerance or stress.
Type 6: Mushy pieces. Mild diarrhea from inflammation or infection.
Type 7: Liquid. Severe diarrhea. Seek medical care if persistent 48+ hours.
Monitor IBS, IBD & Digestive Conditions
Essential for managing IBS, Crohn’s disease, Ulcerative Colitis (UC), celiac disease, SIBO, gastroparesis, diverticulitis, and chronic constipation. Track symptoms → identify triggers → reduce flare-ups. Document patterns for gastroenterologist consultations and treatment adjustments.
Track Crohn’s & UC Flares
Monitor stool frequency, blood presence, urgency, and pain severity. Identify dietary triggers, medication effectiveness, and stress correlations. Essential for adjusting biologics, immunosuppressants, and documenting disease activity for your gastroenterologist.
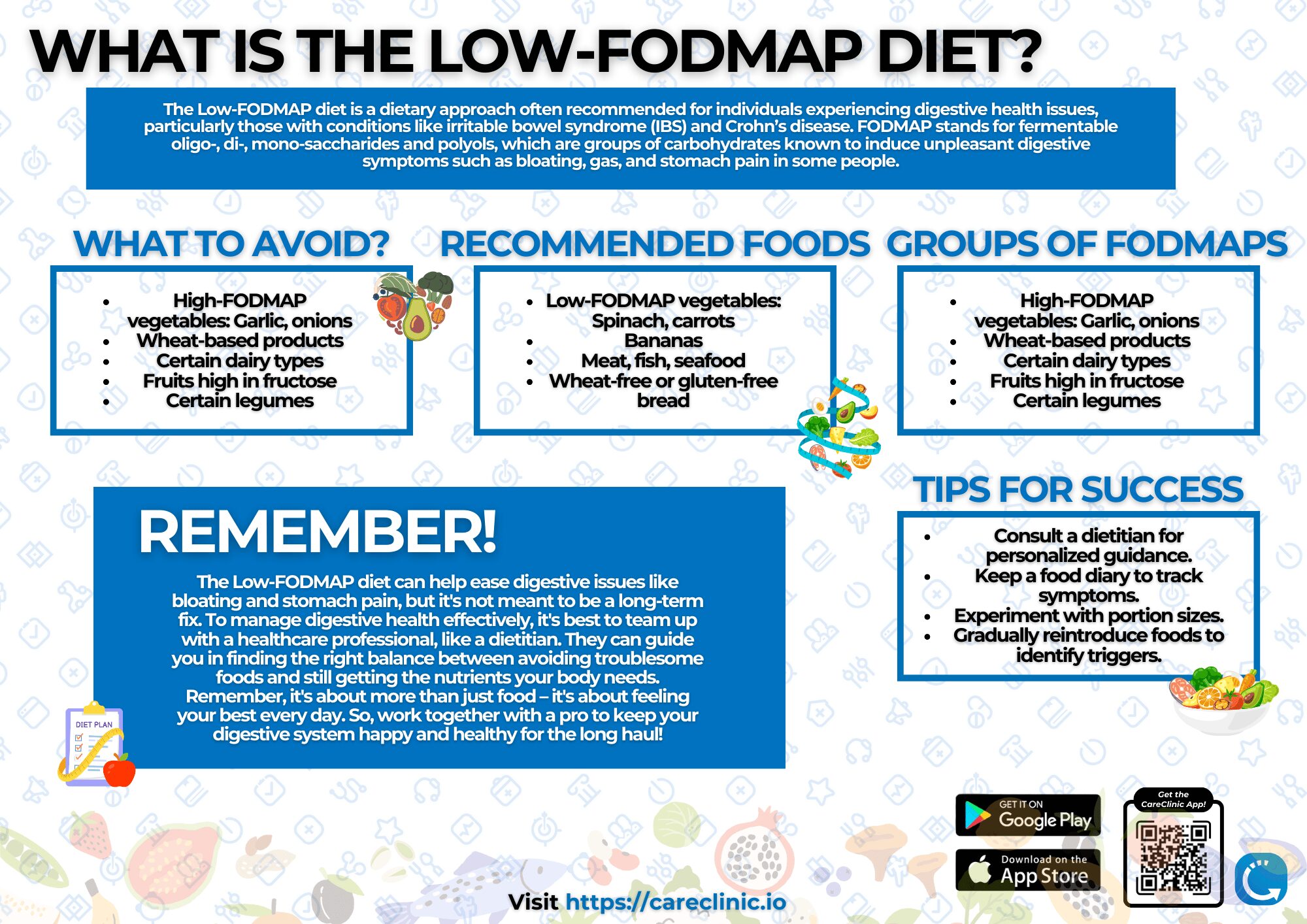
Identify IBS & Food Intolerances
Correlate meals with symptoms to spot FODMAP triggers, lactose intolerance, or gluten sensitivity. Track elimination diet phases and symptom improvements. 50-75% of IBS patients achieve relief when tracking systematically reveals hidden triggers.
Red Flags Requiring Medical Attention
Blood in stool, unexplained weight loss >5%, persistent fever, severe abdominal pain, jaundice, diarrhea/constipation lasting >2 weeks, or pencil-thin stools. Document frequency and severity to share with your doctor promptly.
Infant & Pediatric Tracking
Monitor infant stool patterns, formula intolerances, and pediatric celiac symptoms. Create separate profiles per child. Photo feature captures stool appearance for accurate pediatrician consultations. Detect concerning changes early.
Foods for Digestive Health
Modern food processing introduces complexities our ancestors never faced. Emulsifiers and preservatives alter gut microbiome composition—especially critical for managing IBS, Crohn’s disease, Ulcerative Colitis, and celiac disease. Use the nutrition tracker alongside your bowel log to identify which foods work best for your unique physiology and condition.
Probiotics & Fermented Foods
Yogurt with Lactobacillus and Bifidobacterium shows 69% symptom improvement in IBS patients. Kefir provides 61 bacterial strains. Track probiotic intake to correlate with improvements.
Fiber type matters more than quantity. Soluble fiber (oats, psyllium) helps constipation. Insoluble fiber (wheat bran) may worsen IBS. Log intake and correlate with stool quality.
Low-FODMAP Diet for IBS
50-75% symptom improvement when following low-FODMAP protocols. Hidden FODMAPs lurk in garlic powder, high-fructose corn syrup, and sugar alcohols.
Track every ingredient to spot triggers. Three phases: elimination (2-6 weeks), reintroduction, personalization. The app correlates foods with symptoms for easier identification.
How Stress Affects Your Gut
Your enteric nervous system contains 500 million neurons, which is more than your spinal cord. This “second brain” communicates bidirectionally with your central nervous system. Remarkably, 90% of your body’s serotonin is produced in the gut. Track stress levels in the mood tracker to identify patterns between emotional state and digestive symptoms in your bowel movement app.
Breathing & Physical
Diaphragmatic breathing: Inhale 4, hold 7, exhale 8. Activates parasympathetic response, improving gut motility.
Exercise: 20-minute walks improve transit time. 44% lower constipation risk with daily activity.
Hydration: Water reduces constipation risk by 19-46%. Track fluids alongside bowel movements.
Psychological Approaches
CBT: 42% response in IBS patients. 36% achieve complete remission. Track sessions and progress.
Gut-directed hypnotherapy: 71-76% response rates. Benefits maintained in 73% at 12 months.
Mindfulness: Normalizes cortisol rhythms affecting digestive function. Track practice daily.
Sleep Quality and Digestive Health
Sleep quality profoundly impacts digestive health. Circadian disruption alters gut microbiome composition within 48 hours. Research involving 9,521 participants reveals individuals with short-duration sleep patterns face twice the risk of developing digestive diseases. Track sleep patterns in the sleep tracker alongside bowel movements to identify correlations in your poop tracking app.
Track Bowel Movements and Improve Your Gut Health
Stop guessing what's wrong with your gut. Download the best poop tracker app free today. Join thousands who use this bowel movement tracker app to log stool patterns, track digestive symptoms, and identify IBS triggers for better digestive health.
Frequently Asked Questions