As we age, our bodies have limitations on what they can endure. Children are full of energy and can run around and play all day, whereas adults may require adequate sleep, nutrition, and stretching to accomplish strenuous physical activities. Adults may not be able to do everything that a younger person can do. This contrasts the human fertility rate, which varies between men and women. Women’s ability to have children drops significantly from 35% in their mid-twenties to about 5% in their forties.1 This natural biological process is known as perimenopause or “around menopause,” marked by many symptoms and changes that signify the end of reproductive capability leading to perimenopause aches and pains.
Interestingly, as men age, it becomes more challenging to impregnate women as sperm quality and quantity decrease. However, it is still possible, albeit with more difficulty. This article focuses on the reproductive cycle in women and the symptoms and treatments for perimenopause and, eventually menopause.[1][2]
What Stage does Menstruation Begin?
Have you ever wondered why women are not reproductively capable once they have reached menopause? Or why men can relatively stay fertile. This is not a coincidence but a process that occurs during fetal development. Women are born with all the eggs they will ever produce. As they reach puberty around the age of 8-13 years old, the number of eggs will decline after each menstrual cycle as one age.2 When women do not get their periods in a year they have officially reached menopause which usually occurs around the age of 51.2
What is Menopause?
Women undergo the natural process of menopause as they age, which marks the end of their reproductive years. An indication of menopause is when a woman ceases to have a menstrual period for at least a year. Menopause can occur between the ages of 45-55, although the age range varies among individuals.3 Surgeries such as hysterectomy and chemotherapeutic agents can cause an early onset of menopause by damaging the ovaries. As women approach menopause, they may experience various symptoms such as irregular menstrual cycles and hot flashes, but most significantly, there is a decrease in the production of estrogen, the primary female sex hormone.4
What are Hormones?
Do you ever wonder how the brain can communicate with different body parts and initiate bodily processes even though they are very distant? Well, this is due to chemical messengers known as hormones. Hormones are produced by endocrine glands and travel through the bloodstream, attaching to their respective receptor and initiating changes. Hormones contribute to growth and development and are necessary for functioning reproductive systems within our bodies. Although many hormones are involved, the primary sex hormones in women are estrogen and progesterone.
Estrogen
Estrogen plays a crucial role in overall health by regulating various bodily functions. It is necessary for both men and women, but women require higher estrogen levels, as it is their primary sex hormone. There are three types of estrogen: estradiol, the most common during childbearing years; estrone, which decreases significantly after menopause; and estriol, the primary estrogen during pregnancy.24 Estrogen is essential for the reproductive system and the proper growth and maturation of bones. Without adequate levels of estrogen, bones can become brittle and develop osteoporosis.24[3][4]
Stages of Menopause
Menopause is not characterized by a sudden onset but a gradual process as a woman ages. There are three distinct stages; perimenopause, menopause, and post-menopause.
Perimenopause
Perimenopause, or “menopause transition,” is the earliest stage a woman experiences 8-10 years before menopause.4 The primary sex hormone in females, estrogen, drops in this stage. Some people experience specific menopausal symptoms such as hot flashes, night sweats, and irregular menstruation. Despite these symptoms, individuals are still able to conceive children.
Menopause
If within 12 months a woman has not undergone a menstrual cycle, this would indicate she is now in the menopause phase. Eggs are no longer released from the ovaries, and estrogen production decreases substantially.4
Post-menopause
Once a woman goes a year without experiencing menstrual cycles, months later she is then perceived to be in the postmenopausal phase. While specific symptoms of menopause, including muscle aches and hot flashes, may improve over time, they can persist during post-menopause. Hormonal changes during menopause increase the risk of health conditions such as osteoporosis and heart disease, but lifestyle changes can help combat these risks.4
Perimenopause In-Depth
Perimenopause, or the “time around menopause,” is an essential indicator that a woman’s body is changing, usually occurring during the mid to late 40s. Lasting about 2-8 years but typically is about 4 years in most women.5 There is a significant drop in estrogen during this time, and symptoms and severity also vary among individuals. For example, some experience hot flashes and heavy periods,6 while others may not have these irritating symptoms. Although there is variation, in the final 1-2 years of perimenopause, dropping in estrogen levels, changes in ovulation patterns, and symptoms while still having periods are prevalent.
Perimenopause is a gradual process that occurs in two stages. The early stage of perimenopause typically affects women between the ages of 40-44, although it can begin in some women in their 30s. Hallmarks of this stage include changes in menstrual flow and cycle length, which may become either longer or shorter, as well as estrogen surges.7 The latter stage of perimenopause typically affects women in their late 40s and early 50s. Women may experience irregular periods during this stage and start missing some altogether. In addition, a noticeable drop in estrogen is a symptom of this stage, which can lead to other symptoms such as hot flashes and vaginal dryness.7[5]
Symptoms of Perimenopause
Hot Flashes & Night Sweats
Have you ever experienced a sudden warmth on your palms, scalp, and chest while preparing to sleep or sitting down? This uncomfortable symptom is known as a hot flash, affecting 35-50% of women in the perimenopausal stage.6 Hot flashes occur randomly throughout the day or night, lasting 5-10 minutes. They can also persist for up to 10 years or longer, occurring 1-2 years after menopause.8
Managing Hot Flashes
- Avoid triggers, including spicy foods, hot drinks, and heated environments.5
- Breathing deeply and slowly.5
- Avoid wearing tight-fitted clothing; elect for looser fits, especially on warmer days.5
- During the night time, ensure you have a cool environment or a fan.5
- Drink cold liquids when hot flashes occur.5
Vaginal Dryness
During the late perimenopause stage, it is common for women to experience dryness in the vagina. This is due to the decreased production of estrogen and other essential hormones, resulting in vaginal walls becoming thinner and drier. This can cause discomfort, as individuals may experience enhanced irritation, itching, and pain during intercourse, leading 17-45% of women to report that sex is painful.9
Managing Vaginal Dryness
- Vaginal moisturizers such as Replens increase vaginal moisture, elasticity, and acidity.6
- Use of lubricants such as K-Y Jelly, Astroglide, and K-Y silk-E.6
- Low-dose vaginal estrogen cream, tablet, or ring.10
- Osphena, a selective estrogen receptor modulator taken orally, helps with pain during intercourse.10
Mood Changes
Emotional changes are one of the most common symptoms of menopause impacting women’s mental and physical health. You can download a free emotion-tracking app to record your feelings by clicking here. Although concrete evidence does not support that depression and menopause are linked, 20% of women have symptoms of depression, such as persistent sadness, restlessness, and irritability.11 A study showed that 70% of irritability is the most common and long-lasting symptom.12 Additionally, the stigma associated with aging women and menopause can cause lower mood due to negative body images, and anxiety as well as hot flashes and night sweats which limit sleeping and can cause an increase in irritability and difficulty concentrating.
Managing Mood Changes
- Incorporate exercise and a healthy diet into daily life.11
- Staying connected with friends and family.11
- Adopt new hobbies such as meditation and yoga.11
- Avoid depressants such as alcohol.11
- Join support groups or therapy such as Hormone Replacement Therapy (HRT).11
Slowing of Metabolism & Weight Gain
A common menopause symptom is “menopot,” better known as gaining weight, usually in the abdominal region. Weight gain can be attributed to hormonal changes but also advanced age, lifestyle, and genetic factors.13 Excess weight in addition to unhealthy lifestyle factors puts individuals at risk of type 2 diabetes, hypertension, and heart disease.13
Managing Weight Gain
- Include physical and aerobic exercises coupled with strength training for weight maintenance.13
- Keep track of what you are eating and limit unnecessary junk foods.13
- Limit alcohol intake.13
- Seek support either from family and friends or from personal fitness coaches.13

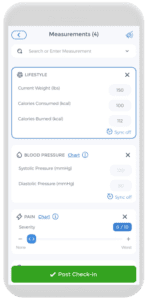
Women experiencing menopause should consider their current stage as it is an individualized experience with various symptoms associated with each stage. These symptoms will intensify as hormonal fluctuations become more significant. It is overwhelming to recall all the symptoms, and some may even be mistaken for normal daily experiences during menstruation. However, there is no need to worry as CareClinic, a mobile health app, provides an easy-to-use interface for symptom tracking. The app has a wide range of options for users to search and select specific symptoms they are experiencing. In addition, users can record the severity of their symptoms, such as perimenopause aches and pains, the time they occur, and the triggers. This data can be valuable for yourself as well as for medical practitioners. They can use it in combination with other factors, such as age and life events, to determine the specific stage of menopause a woman is in.
Chronic Pain: Joints and Muscles
Have you ever finished an intense workout or activity and felt incredibly sore afterward? However, you notice that your joint and muscle pain gradually decreases and is gone after a few days. We are fortunate, as an estimated 75% of women experience musculoskeletal pain during perimenopause.14 Perimenopause aches and pains persist over time and are chronic, affecting individuals in postmenopause as well.
What Causes Joint and Muscle Pain?
You may think that painful joints and muscle pain are just natural processes accompanied by age. This is true; as we age, we lose muscle mass, which can increase the prevalence of conditions leading to perimenopause aches and pains, especially arthritis and arthralgia. Remember the discussion about hormonal changes? Well, estrogen is the main culprit of the perimenopause aches and pains women in perimenopause experience. Research suggests that the decrease in estrogen in perimenopausal women will increase their sensitivity to pain.15 Estrogen has anti-inflammatory properties essential to lower the perception of pain. When estrogen is presented in low quantities, problematic inflammatory states prevail, leading to swelling of the joints and the persistence of pain.[6]
The Link Between Menopause and its Conditions
Joint stiffness, aches, and pain affect everybody to some degree but is a frequent obstacle in the lives of women during menopause. Joint stiffness and associated symptoms affect more than half of women in menopause, increasing the risk of experiencing chronic pain by 85%.16 Menopause’s stages make individuals prone to develop various chronic conditions due to multiple factors, primarily estrogen deficiency. These conditions include osteoporosis, rheumatoid arthritis, arthralgia, and fibromyalgia
Osteoporosis
Loss of bone density is a concern for women in perimenopause, as research indicates 20% of bone loss can occur during these stages.17 Bone loss is accelerated, as estrogen-deficient women will not have adequate receptor binding in regions such as the joints. This makes bones brittle and prone to breaks and fractures. This chronic condition, osteoporosis, poses another obstacle and painful experience for perimenopausal women.
Arthralgia & Fibromyalgia
Development of arthralgia increases when a woman enters menopause associated with estrogen levels. Arthralgia, which leads to joint stiffness, can make it increasingly difficult to accomplish daily tasks such as getting physical activity.
Additionally, fibromyalgia is another chronic condition that leads to painful joints, fatigue, digestive problems, and overall tenderness in the body.18 Women who enter menopause early are twice as likely to develop fibromyalgia than women who have not reached menopause. Consequently, other chronic conditions common in estrogen-deficient women during menopause increase the risk of fibromyalgia.19[7][8][9][10]
Treatment Options
Exercise
You may think including exercise when experiencing pains in joints and muscles is counterintuitive. Luckily, it is not, as bone strength/health improves during activities. We do not mean to get into a strenuous weight training program, but more so to take gradual steps and participate in low-impact exercises. Activities such as swimming, biking, and yoga are great examples. Yoga may not seem active, but it is a great way to improve stretch and flexibility. Ultimately relieving joint stiffness and perimenopause aches and pains. Additionally, weight gain is a natural process during menopause, so keeping your weight under a healthy range is essential as it puts less stress on joints.
Engaging in physical activity can be very difficult, especially in the era of social media. Distractions such as TikTok, Instagram, and gaming can make us lazy. It is essential to include some physical activity in everyday life. This has countless benefits, such as improving cognition and lowering the risk of diseases.20 CareClinic is a great app to log your fitness journey using the measurement tool. Inputting current weight, calories consumed, burned, and weight goals serve as motivation. Analysis of charts regarding your fitness journey allows insight to see how much you have improved and how far you have come.
Diet
Maintaining a healthy diet is difficult, as we find ourselves so busy sometimes we forget to eat and cook. We tend to take the easy route to order food, especially since it is so easy with apps such as UberEats and Skip the Dishes. Diets high in carbohydrates, and sugars and low in omega-3 fatty acids worsen pain and lead to chronic inflammation. Fruits, vegetables, and overall high-fibre foods, in addition to omega-3-rich foods such as salmon and nuts, can help combat the physical symptoms of menopause. Additionally, vitamin D and magnesium supplements are essential as they promote bone and joint health and have anti-inflammatory properties.21
Hormone Replacement Therapy
Much of menopausal symptoms can be attributed to estrogen deficiencies leading to difficulty living comfortably. Many alternatives are available to treat symptoms, the best being hormonal replacement therapy (HRT). HRT involves medications that increase female hormones, specifically estrogen and progesterone.22 Research shows, hot flashes, vaginal discomfort, and mood swings are reduced during HRT.22 Alleviation of chronic symptoms of arthritis is also reduced, including slowing down bone density loss as well as reducing the chances of fracture.22,23[11][12]
Using CareClinic as a Treatment Tool
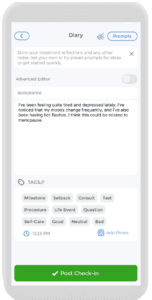
Life can be stressful, and we must learn how to cope with various stressors. Coping mechanisms can be positive or negative, and we must choose the right path. When we think about health, we often focus on physical health, such as eating a healthy diet and exercising regularly. However, mental health is just as important and needs attention. Many people suppress their emotions because they fear appearing weak or not knowing how to manage them correctly. Journaling is a simple and effective method of alleviating stress that I have adopted.
However, carrying a physical journal and pen everywhere can be impractical. Luckily, Careclinic offers a built-in diary function that lets you easily record your thoughts and feelings on your phone. With many prompts to choose from, it is an excellent tool for coping with mood changes and depression that are common among women in perimenopause. Taking care of our mental health is crucial, and using Careclinic can be an essential step in achieving that goal.[13]
References
- “How much does egg freezing cost? Everything you want to know about fertility preservation”. https://www.axios.com/local/charlotte/2019/12/11/how-much-does-egg-freezing-cost-everything-you-want-to-know-about-fertility-preservation-189280
- “30-somethings nudge U.S. birth rate off record low”. https://www.axios.com/2025/04/24/pregnancy-age-birth-rate-cdc-fertility
- “Eunice Kennedy Shriver National Institute of Child Health and Human Development – NICHD”. https://www.nichd.nih.gov/health/topics/factsheets/puberty
- “Menopause”. https://www.who.int/news-room/fact-sheets/detail/menopause
- “Perimenopause: Age, Stages, Signs, Symptoms & Treatment”. https://my.clevelandclinic.org/health/diseases/21608-perimenopause
- “Most Women Experience Hot Flashes for Over 7 Years, Study Finds”. https://time.com/3711162/menopause-symptoms-7-years/
- “Musculoskeletal Pain during the Menopausal Transition: A Systematic Review and Meta-Analysis – PubMed”. https://pubmed.ncbi.nlm.nih.gov/33299396/
- “Update on Menopausal Hormone Therapy for Fracture Prevention – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC6944675/
- “Menopausal arthralgia: Fact or fiction – PubMed”. https://pubmed.ncbi.nlm.nih.gov/20537472/
- “Fibromyalgia and menopause. Examination of the relationship”. https://pubmed.ncbi.nlm.nih.gov/3463950/
- “How (and why) to exercise during menopause: 10 tips and practices — Calm Blog”. https://blog.calm.com/blog/exercise-during-menopause
- “Managing Joint Pain During Menopause: Expert Tips and Strategies”. https://puresportsmed.com/blog/posts/managing-joint-pain-during-menopause
- “The Power of Journaling: What Science Says About the Benefits for Mental Health and Well-Being – Child Mind Institute”. https://childmind.org/blog/the-power-of-journaling/