Buprenorphine is a medication that has gained significant attention in recent years for its potential benefits in pain management. As medical professionals continue to search for safe and effective alternatives to traditional pain medications, buprenorphine has emerged as a promising option. In this article, we will explore the benefits of buprenorphine for pain management and discuss its role in improving patient outcomes.[1][2][3]
Understanding Buprenorphine: An Overview
Before delving into the benefits of buprenorphine, it’s important to have a solid understanding of what![]() this medication is and how it works. Buprenorphine is a semi-synthetic opioid that was first introduced for the treatment of opioid addiction. However, its unique properties have also made it an attractive choice for managing pain.
this medication is and how it works. Buprenorphine is a semi-synthetic opioid that was first introduced for the treatment of opioid addiction. However, its unique properties have also made it an attractive choice for managing pain.
Buprenorphine’s journey began in the late 1960s when it was first synthesized by a team of researchers led by Dr. K. W. Bentley. The goal was to create a medication that could effectively treat pain without the risk of respiratory depression and overdose associated with traditional opioids. This led to the development of buprenorphine, a medication that has revolutionized the field of pain management.
What is Buprenorphine?
Buprenorphine belongs to a class of medications known as opioid partial agonists. Unlike traditional opioids, which are full agonists and bind to opioid receptors in the brain, buprenorphine only partially activates these receptors. This partial activation produces a ceiling effect, meaning that higher doses of buprenorphine do not result in greater pain relief. This characteristic reduces the risk of respiratory depression and overdose, making buprenorphine a safer option for chronic pain patients.
It’s important to note that buprenorphine is not only used for pain management in chronic pain patients but also for the treatment of opioid addiction. Its unique pharmacological properties make it an effective medication for opioid detoxification and maintenance therapy. By reducing cravings and withdrawal symptoms, buprenorphine helps individuals on the path to recovery regain control of their lives.
How Does Buprenorphine Work?
When buprenorphine binds to opioid receptors, it blocks other opioids from attaching to these receptors. Competetive opioid antagonists can be be particularly beneficial in patients who struggle with opioid addiction, as it helps to reduce cravings and withdrawal symptoms. However, in the context of pain management, buprenorphine’s ability to block other opioids can also enhance its efficacy. By preventing other opioids from binding to the receptors, buprenorphine allows for more targeted pain relief.
Furthermore, buprenorphine’s long duration of action sets it apart from other opioids. While traditional opioids may require frequent dosing to maintain pain relief, buprenorphine’s effects can last for up to 72 hours. This extended duration of action not only provides sustained pain relief but also reduces the need for frequent medication administration, improving convenience and compliance amongst chronic pain patients.
Additionally, buprenorphine’s unique pharmacokinetic profile contributes to its overall safety and effectiveness. Its high affinity for opioid receptors and slow dissociation from these receptors results in a reduced risk of overdose and respiratory depression. This makes buprenorphine a valuable option for patients who require long-term pain management or those at risk of opioid-related complications.
In conclusion, buprenorphine is a versatile medication that offers significant benefits in both opioid addiction treatment and pain management. Its partial agonist properties, competitive antagonism, and extended duration of action make it a safer and more effective alternative to traditional opioids. By understanding the mechanisms of buprenorphine, healthcare professionals can make informed decisions and provide optimal care to their patients.[4][5][6]
The Role of Buprenorphine in Pain Management
Now that we have a basic understanding of buprenorphine, let’s explore its role in chronic pain management and how it compares to traditional pain management methods.
Pain management is a critical aspect of healthcare, as it aims to alleviate suffering and improve the quality of life for patients experiencing acute or chronic pain. Traditionally, opioids such as morphine or oxycodone have been commonly used for pain relief. While these medications can be effective for short-term pain relief, long-term use carries significant risks.
Opioids are notorious for their potential to cause addiction, tolerance, and overdose, even among opioid naïve patients. The addictive nature of opioids can lead to a cycle of dependency, making it challenging for both buprenorphine users and opioid naïve patients to discontinue their use due to withdrawal symptoms. Additionally, the development of tolerance over time may require higher and higher doses to achieve the same level of pain relief. This can lead to a dangerous escalation of opioid dosage, increasing the risk of overdose.
Traditional Pain Management Methods vs. Buprenorphine Therapy
Recognizing the limitations and risks associated with traditional pain treatment methods, alternative options have been explored. Buprenorphine, a partial opioid agonist, offers a safer alternative by providing effective analgesia without the same level of risk for dependency and overdose.
Unlike full opioid analgesics, such as morphine, buprenorphine has a ceiling effect on respiratory depression. This means that even if higher doses are administered, the risk of respiratory depression and subsequent overdose remains relatively low. This property makes buprenorphine a valuable tool in pain management, especially for patients who are at risk for opioid-related complications.
Another advantage of buprenorphine is its long duration of action. Unlike short-acting opioids, which require frequent administration to maintain pain relief, buprenorphine can provide sustained analgesia for up to 72 hours. This extended duration of action reduces the need for frequent dosing, enhancing convenience and compliance amongst chronic pain patients.
Types of Pain Treated with Buprenorphine
 Buprenorphine treatment has been shown to be effective in managing a wide range of pain conditions. From acute post-operative pain to chronic and severe pain associated with conditions such as cancer or neuropathy, buprenorphine has demonstrated its versatility for chronic pain patients.
Buprenorphine treatment has been shown to be effective in managing a wide range of pain conditions. From acute post-operative pain to chronic and severe pain associated with conditions such as cancer or neuropathy, buprenorphine has demonstrated its versatility for chronic pain patients.
In the acute setting, buprenorphine treatment can provide effective pain relief after surgical procedures, reducing the need for high-dose opioids. This is particularly beneficial for patients who may be at risk for opioid-related complications, such as the elderly or those with pre-existing respiratory conditions.
In chronic severe pain management, buprenorphine has shown promise in improving pain control and overall quality of life. Conditions such as cancer-related pain or neuropathy can be debilitating and challenging to manage. Buprenorphine’s unique pharmacological profile allows for effective pain relief while minimizing the risk of addiction and opioid overdose.
Furthermore, buprenorphine has been found to have a lower risk of developing tolerance compared to traditional opioids. This means that patients may experience sustained pain relief without the need for escalating doses over time.
Overall, buprenorphine plays a crucial role in pain management by offering a safer alternative to traditional pain medications. Its unique properties make it a valuable option for patients who may not respond well to other pain medications or who are at risk for opioid-related complications. By providing effective analgesia with a reduced risk of addiction, tolerance, and opioid overdose, buprenorphine has the potential to improve the lives of countless individuals suffering from acute or chronic pain.[7][8][9][10][11][12]
The Benefits of Buprenorphine for Pain Management
Now that we understand buprenorphine’s role in pain management, let’s explore the specific benefits it offers to patients.
Improved Pain Control
One of the primary benefits of buprenorphine is its ability to provide effective pain relief. Through its unique mechanism of action, buprenorphine can target and alleviate pain without the same risk of tolerance that is commonly associated with other opioids. This means that patients can experience sustained pain control without the need for frequent dose adjustments.
Buprenorphine works by binding to the opioid receptors in the brain, spinal cord, and other parts of the body. However, unlike other opioid analgesics, it acts as a partial agonist, meaning it only partially activates these receptors. This partial activation allows buprenorphine to provide pain relief without the same level of respiratory depression and sedation that is often seen with other opioid analgesics.
Furthermore, buprenorphine has a long duration of action due to its high affinity for the opioid receptors. This means that it stays bound to the receptors for a longer period of time, providing sustained pain relief. Patients can benefit from this extended pain control, as it allows them to go longer periods between doses and reduces the risk of breakthrough pain.
Reduced Side Effects
Unlike traditional opioids, buprenorphine has been found to have fewer side effects. This is partially attributed to its partial agonist properties, which result in a ceiling effect and reduce the risk of respiratory depression and sedation. The ceiling effect means that as the dose of buprenorphine increases, the pain relief plateaus, while the risk of side effects remains relatively stable.
Additionally, buprenorphine has a longer half-life compared to other opioids, which allows for less frequent dosing and a more stable blood concentration. This can help to minimize fluctuations in pain control and reduce the likelihood of side effects. Patients can experience a more consistent level of pain relief throughout the day, without the need for frequent dosing that can disrupt their daily activities.
Moreover, buprenorphine has a lower risk of causing constipation, a common side effect of opioids. This is because it does not affect the gastrointestinal motility to the same extent as full agonist opioids. Patients who are already experiencing constipation due to other medications or medical conditions may find buprenorphine to be a more tolerable option.
Potential for Lower Addiction Risk
Perhaps one of the most significant benefits of buprenorphine in pain management is its lower risk of addiction compared to other prescription opioids. Due to its partial agonist properties and receptor-blocking effects, buprenorphine is less likely to cause physical dependence and cravings. This makes it an attractive option for patients who are at risk for opioid addiction or who have a history of substance abuse.
By occupying the opioid receptors in the brain, buprenorphine blocks the effects of other opioids. This means that if a patient were to take a full agonist opioid while on buprenorphine, they would not experience the same level of euphoria or pain relief. This deterrent effect can help prevent relapse in individuals who are in recovery from opioid addiction.
Furthermore, buprenorphine is available in different formulations, such as sublingual tablets or transdermal patches, which can be prescribed for pain management. These formulations provide a controlled release of the medication, reducing the risk of misuse or diversion. Patients can benefit from the pain-relieving effects of buprenorphine without the same potential for abuse as other opioids.
In conclusion, buprenorphine offers several benefits for pain management. It provides improved pain control without the risk of tolerance, has fewer side effects, and carries a lower risk of addiction compared to other prescription opioids. These advantages make buprenorphine an attractive option for patients who require long-term pain management, especially those who may be at risk for opioid addiction or have a history of substance abuse.
Clinical Studies Supporting Buprenorphine Use
As buprenorphine’s popularity grows, so does the body of evidence supporting its use in pain management.
Buprenorphine, a semi-synthetic opioid, has been the subject of numerous clinical studies that have demonstrated its efficacy in various pain conditions. These studies provide valuable insights into the use of buprenorphine and its potential benefits for patients seeking effective pain relief.
Key Research Findings
One notable study published in the Journal of Pain Research focused on patients with chronic back pain. The researchers compared the effectiveness of buprenorphine with other opioid analgesic medications commonly used for pain management. The study found that chronic pain patients treated with buprenorphine had superior pain relief and improved functional outcomes compared to the other opioids tested. This suggests that buprenorphine may be a more effective option for individuals suffering from chronic back pain.
In addition to chronic back pain, buprenorphine has also shown positive outcomes in other pain conditions. Studies have reported its efficacy in relieving pain associated with osteoarthritis, a degenerative joint disease that affects millions of people worldwide. Furthermore, research has indicated that buprenorphine may be beneficial for individuals with fibromyalgia, a chronic condition characterized by widespread musculoskeletal pain.
Post-surgical pain is another area where buprenorphine has demonstrated its effectiveness. Studies have shown that buprenorphine can provide effective pain relief after surgical procedures, reducing the need for other opioids and potentially minimizing the risk of opioid-related side effects.[13][14]
Potential Risks and Side Effects of Buprenorphine
While buprenorphine offers significant benefits, it is not without its potential risks and side effects. It’s important for both patients and healthcare professionals to be aware of these considerations.
Common Side Effects
Like any medication, buprenorphine can cause side effects. Some of the most common side effects include constipation, nausea, dizziness, and headache. However, it’s worth noting that these side effects are generally mild and well-tolerated.
Constipation is a common side effect of buprenorphine due to its effects on the gastrointestinal system. Patients may experience infrequent bowel movements or difficulty passing stool. It is important for patients to maintain a healthy diet, increase fluid intake, and engage in regular physical activity to help alleviate this side effect.
Nausea is another common side effect of buprenorphine. It can range from mild discomfort to severe vomiting. Patients can try taking the medication with food to help reduce the likelihood of experiencing nausea. If the symptoms persist, patients should consult their healthcare provider for further guidance.
Dizziness is a potential side effect that can occur when starting buprenorphine or adjusting the dosage. It is important for patients to be cautious when performing activities that require alertness, such as driving or operating heavy machinery. If dizziness becomes persistent or severe, medical attention should be sought.
Headache is also reported as a common side effect of buprenorphine. It can range from mild to moderate intensity and may be accompanied by sensitivity to light or sound. Patients can try over-the-counter pain relievers, such as acetaminophen or ibuprofen, under the guidance of their healthcare provider to alleviate headache symptoms.
It’s important for patients to communicate any side effects to their healthcare provider so that appropriate management strategies can be implemented. The healthcare provider may adjust the dosage or prescribe additional medications to help alleviate the side effects.
Understanding the Risk of Dependency
While buprenorphine carries a lower risk of addiction compared to other opioids, there is still a potential![]() for physical dependence. It’s important for patients to be aware of this risk and to work closely with their healthcare provider to develop a safe and effective pain management plan.
for physical dependence. It’s important for patients to be aware of this risk and to work closely with their healthcare provider to develop a safe and effective pain management plan.
Physical dependence occurs when the body becomes accustomed to the presence of buprenorphine and requires it to function normally. Abrupt discontinuation of buprenorphine can lead to withdrawal symptoms, which can be uncomfortable and distressing for patients. Symptoms of withdrawal may include anxiety, restlessness, muscle aches, and insomnia.
To minimize the risk of withdrawal symptoms, healthcare providers may recommend a gradual tapering of the medication if it is no longer needed. This involves gradually reducing the dosage over a period of time until the patient can safely stop taking buprenorphine. It is important for patients to follow their healthcare provider’s instructions closely and to communicate any concerns or difficulties during the tapering process.
By being aware of the potential risks and side effects of buprenorphine, both patients and healthcare professionals can work together to ensure safe and effective pain management. Regular communication and close monitoring are essential in order to address any concerns and optimize the benefits of this medication.[15]
The Future of Buprenorphine in Pain Management
As research into buprenorphine continues to evolve, there are exciting possibilities on the horizon.
Ongoing Research
Researchers are actively exploring additional applications for buprenorphine in pain management. Studies are underway to investigate its effectiveness in conditions such as neuropathic pain, migraine, and even cancer-related pain. The results from these studies have the potential to further expand the use of buprenorphine and provide even more options for patients in need of effective pain relief.
Potential New Applications for Buprenorphine
Beyond pain management, buprenorphine is also being investigated for its uses in other areas of medicine. Researchers are exploring its potential in the treatment of psychiatric conditions such as depression and post-traumatic stress disorder. These potential new applications demonstrate the far-reaching impact that buprenorphine may have in improving patient outcomes across multiple healthcare domains.
In conclusion, buprenorphine holds great promise as a safe and effective option for pain management. Its unique properties make it an attractive choice for patients who are seeking pain relief while minimizing the risks of addiction and other opioid-related complications. The growing body of evidence supporting its use, alongside the positive patient perspectives, further solidifies buprenorphine’s role in improving the lives of individuals living with pain. As research into buprenorphine continues, we eagerly anticipate the potential new discoveries and applications that lie ahead.
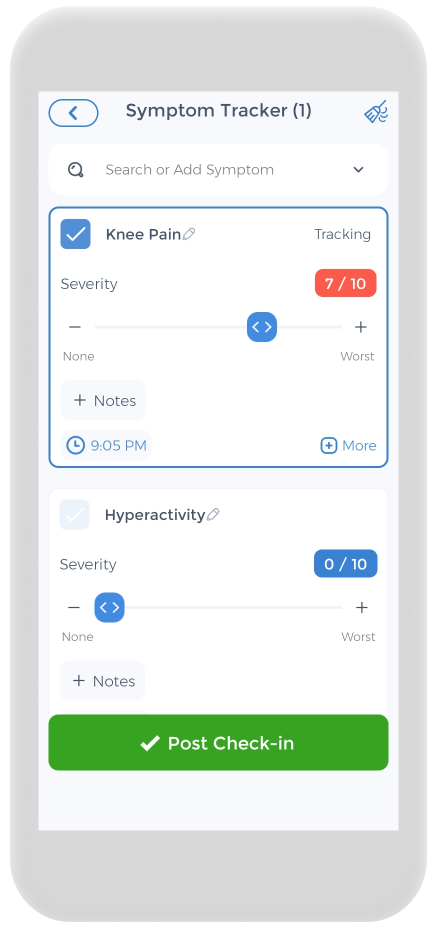
Using the CareClinic App to Manage Pain
Keeping a pain journal is essential for your health, and the CareClinic app can assist you with this. The app can be used as a health and clinical journal. Simply go to the app’s pain diary section and record your daily symptoms, meds, and other triggers as they occur. There are other parts of the app dedicated to tracking each of these. This can assist you in recognizing early warning symptoms. The app is designed to help you better your chronic low back pain and acute pain-related health, whether you suffer from chronic low back pain, neck pain, acute injuries or traumatic injuries, common knee injuries, autoimmune illness, acute inflammation, meniscus tear, or reactive arthritis.
Sources
- https://www.ninds.nih.gov/health-information/disorders/pain
- https://painbc.ca/health-professionals/education/OT-workshop
References
- “Twelve reasons for considering buprenorphine as a frontline analgesic in the management of pain”. https://pubmed.ncbi.nlm.nih.gov/22809652/
- “Buprenorphine: Another Tool in the Analgesic Toolbox? | AAHPM”. https://aahpm.org/publications/aahpm-quarterly/issue-archive/spring-2020/spring-20-feature/
- “Anesthesia & Analgesia”. https://journals.lww.com/anesthesia-analgesia/fulltext/2023/07000/analgesic_effect_of_buprenorphine_for_chronic.6.aspx
- “Pharmacology of medicines available for the treatment of opioid dependence – Guidelines for the Psychosocially Assisted Pharmacological Treatment of Opioid Dependence – NCBI Bookshelf”. https://www.ncbi.nlm.nih.gov/books/NBK143173/
- “Chapter 3D: Buprenorphine – Medications for Opioid Use Disorder – NCBI Bookshelf”. https://www.ncbi.nlm.nih.gov/books/NBK574909/
- “Buprenorphine for opioid dependence | Mental Health Clinician”. https://meridian.allenpress.com/mhc/article/3/6/286/37195/Buprenorphine-for-opioid-dependence
- “Efficacy and adverse effects of buprenorphine in acute pain management: systematic review and meta-analysis of randomised controlled trials – British Journal of Anaesthesia”. https://www.bjanaesthesia.org.uk/article/S0007-0912%2817%2954081-7/fulltext
- “Buprenorphine induces ceiling in respiratory depression but not in analgesia – PubMed”. https://pubmed.ncbi.nlm.nih.gov/16547090/
- “Buprenorphine: a treatment and cause of opioid-induced respiratory depression”. https://pubmed.ncbi.nlm.nih.gov/34996591/
- “Transdermal buprenorphine in the management of persistent pain – safety aspects – PMC”. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1661652/
- “Efficacy and Safety of Transdermal Buprenorphine for Acute Postoperative Pain: A Systematic Review and Meta-analysis – PubMed”. https://pubmed.ncbi.nlm.nih.gov/37442403/
- “Safety And Efficacy Of The Unique Opioid Buprenorphine For The Treatment Of Chronic Pain”. https://pubmed.ncbi.nlm.nih.gov/31997882/
- “Buprenorphine transdermal system in adults with chronic low back pain: a randomized, double-blind, placebo-controlled crossover study, followed by an open-label extension phase”. https://pubmed.ncbi.nlm.nih.gov/20685494/
- “Buprenorphine for acute post-surgical pain: A systematic review and meta-analysis – PMC”. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10077784/
- “”. https://www.nhs.uk/medicines/buprenorphine-for-pain/side-effects-of-buprenorphine/
- “Neuropathic Pain in Cancer: What Are the Current Guidelines? – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC11416366/
- “Experts Make the Case for Buprenorphine Use in Cancer-Related Pain Management”. https://www.oncnursingnews.com/view/experts-make-the-case-for-buprenorphine-use-in-cancer-related-pain-management
- “Buprenorphine: prospective novel therapy for depression and PTSD”. https://pubmed.ncbi.nlm.nih.gov/32204739/
- “Observational Evidence for Buprenorphine's Impact on Posttraumatic Stress Symptoms in Veterans With Chronic Pain and Opioid Use Disorder”. https://www.psychiatrist.com/jcp/buprenorphine-and-ptsd/