Lupus flares occur in people with lupus when the symptoms of the disease worsen. Flare ups can occur suddenly and last from days to weeks. Flare ups are not dangerous but can make lupus uncomfortable and limit your ability to work, play, or have fun with friends and family. Thankfully, there are ways to prevent lupus flare ups, as well as ways to treat them when they occur.
Lupus flare ups are caused by a number of things. Sometimes, they can be brought on by stress or infection. Other times, they may be the result of taking certain medications or exposure to the sun. Flare ups can also occur when the body is fighting off an illness or injury.
Table of Contents
- Firstly, What is Lupus?
- Causes of Lupus Flares
- Traits of Chronic autoimmune disease
- Before a Lupus Flare Up Occurs
- What does a Lupus Flare feel like
- Treatment for Symptoms During a Lupus Flare
- Melatonin vs. Cymbalta for Reducing Symptoms
- Menstrual Cycle and Lupus Flares
- Triggers that can cause a Lupus Flare
- Discovering Triggers & Tracking Lupus
- How long does a lupus flare last
- What is a Lupus fever?
- How often do Lupus flares occur
- Managing Daily Life with Lupus Symptoms
Firstly, What is Lupus?
The National Institute of Arthritis and Musculoskeletal and Skin Diseases, a division of the National Institutes of Health, states that lupus is an autoimmune disorder in which the body’s immune system mistakenly attacks healthy tissue. It can affect many different organs in the body, including skin, joints, kidneys, heart and lungs. Lupus is also described as being fairly prevalent with more than 300,000 people diagnosed with lupus in the United States alone. Symptoms associated with lupus include things like recurring skin rashes or sores over joints or around fingernails or toes.
Causes of Lupus Flares
A lupus flare up is an exacerbation of the symptoms of lupus. The cause of the flare up may be due to a variety of triggers that can range from environmental factors (temperature changes) to medications such as oral contraceptives or antibiotics. Lupus flares are also known as a bout or attack of lupus because it can come and go quickly. Lupus flares usually last for days with recovery periods in between them but for some people, it could be minutes if not hours.
But what causes Lupus flares? There are many different causes. Many experts believe that there isn’t one thing in particular that causes lupus flares, but rather many different things combined. Some triggers include drugs, infections like mono or bladder infection, stress, excessive sun exposure, too much heat and cold exposure, certain foods like dairy products or caffeine; heavy menstruation; other autoimmune diseases; infectious diseases like Lyme disease; and even pregnancy.
Traits of Chronic autoimmune disease
Chronic autoimmune disorders are characterized by periods of remission and relapse. The main goal of treatment is to relieve symptoms of lupus and protect organs from further damage. The most common ones include: Celiac disease, Crohn’s disease, Multiple sclerosis, Psoriasis, and Rheumatoid arthritis. All of these diseases share some common symptoms which include:
- Inflammation: This is when the body’s immune system mistakenly attacks healthy tissue in the body. This can cause redness, swelling, and pain.
- Autoantibodies: These are proteins that attack the body’s healthy cells by mistake.
- Immune system dysfunction: This is when the body’s immune system doesn’t work properly and can’t fight off infections or other foreign invaders like it should.
The most common symptoms include: fatigue, joint pain, rash, and fever. Lupus flares are periods of time when lupus symptoms get worse for a few days or weeks. There are many factors that cause lupus flares but thankfully there are some ways of preventing and treating these flare ups.
Before a Lupus Flare Up Occurs
During a flare up, the symptoms are often debilitating for lupus patients. Lupus flares can last for weeks or months at a time with no obvious sign that they’re coming to an end. You may experience joint pain and fever alongside your other symptoms or even without any additional symptoms. It’s also possible that these bouts of inflammation are not lupus flares but instead another infection like a bladder infection.
To get the most accurate diagnosis you should see your doctor as soon as possible to get them started on some antibiotic treatment. Once diagnosed with lupus you’ll need to be pro-active in preventing future flare ups by maintaining a healthy lifestyle. Eating healthy meals full of fresh fruits and vegetables along with following an exercise routine will help keep you on track for overall health!
What does a Lupus Flare feel like
The type of lupus flare that you experience will depend on which kind of lupus you have. Symptoms for Systemic Lupus Erythematosus (SLE) can be flu-like symptoms such as chills, fever, body aches, nausea and malaise. Skin involvement is usually the most serious sign. Lupus erythematosus discoid has similar symptoms but they are only localized to the skin. Neither type of lupus flare should be taken lightly as it could lead to complications or kidney damage if not monitored appropriately.
Lupus nephritis is a kidney inflammation that occurs in people with lupus. Lupus nephritis occurs when the body’s immune system starts to attack the kidneys. The symptoms of lupus nephritis can range from mild to severe, and they can also lead to kidney failure. Kidney disease is a common complication in patients with lupus. Lupus can cause damage to the small blood vessels in the kidneys, which can lead to inflammation and kidney scarring. Kidney disease can also be caused by other factors, such as high blood pressure or diabetes.
Lupus patients can feel emotionally and physically taxing to go through. A person would feel an overwhelming sense of fatigue, joint pain, fever and other debilitating symptoms. Additionally, the person may feel isolated as not many people understand what it’s like to go through a flare up. Flare ups can also be emotionally draining as they are often unpredictable and come without warning.
Lupus flares can be extremely frustrating to deal with, but it’s important to remember that there are things you can do to prevent them. Maintaining a healthy lifestyle, managing stress levels and avoiding triggers are all key in preventing lupus flares.
Treatment for Symptoms During a Lupus Flare
It’s important to learn how to treat a lupus flare up when it comes on. Some common treatments for the symptoms of a lupus flare are anti-inflammatory medications or NSAIDs such as ibuprofen or naproxen. Prescription drugs such as prednisone can be prescribed for more severe flares where the disease is active in the bloodstream.
There are other non-prescription options including taking over-the-counter medications like acetaminophen or an oral decongestant such as pseudoephedrine. Keeping hydrated with fluids throughout the day can also help you get relief from some of your symptoms. Avoiding things that make your condition worse (such as tobacco smoke) and getting plenty of rest are also important in helping you recover from a lupus flare.
Lupus rashes are caused by the body’s immune system attacking its own cells. They can be red, scaly and itchy and can vary in size and shape. They can also spread quickly so it’s important to seek medical attention if you are experiencing worse clinical signs.
Lupus flares can be difficult to deal with even with moderate flares for people with Lupus. There are things you can do to manage your symptoms and feel better. Work with your doctor to come up with a treatment plan that’s right for you and make sure to avoid triggers that
Melatonin vs. Cymbalta for Reducing Symptoms
 Two drugs are commonly used for reducing lupus symptoms, they are Cymbalta and melatonin. While Cymbalta is a medication prescribed by doctors for severe lupus symptoms, melatonin is more of a supplement that you can use if you experience mild flare ups and want to take care of the situation at home. Here’s a look at how each one works and what we know about which one is better.
Two drugs are commonly used for reducing lupus symptoms, they are Cymbalta and melatonin. While Cymbalta is a medication prescribed by doctors for severe lupus symptoms, melatonin is more of a supplement that you can use if you experience mild flare ups and want to take care of the situation at home. Here’s a look at how each one works and what we know about which one is better.
Cymbalta (antidepressant):
Cymbalta has been shown to work as well as other medications in people with moderate to severe Lupus and it also improves sleep problems. However, there have been some concerns that this drug may cause liver damage or heart problems among those who already have such conditions. It also causes sexual side effects in men who take it. Women should not take it because of the potential risk of birth defects. It’s important to note that this medicine does not cure lupus, but it does help ease some of the pain and discomfort associated with it.
Melatonin (supplement):
This hormone is naturally produced by your body during periods of darkness so that you can fall asleep. Your doctor will prescribe melatonin only when taking other medicines has not worked; they recommend using them only when absolutely necessary since they are considered experimental treatments. One benefit? Melatonin does not have as large of negative side effects as Cymbalta does! For example, the incidence of nausea and vomiting due to Cymbalta was 9% while with melatonin, it was 0%.
In addition, you need a prescription for Cymbalta but all you need is your health insurance card to get melatonin. Studies show that melatonin may be as effective as Cymbalta in easing symptoms and improving quality of life. So why do patients take Cymbalta over melatonin?
The answer depends on personal preference and your doctor’s advice! Studies show that both medications reduce pain and improve sleep quality. Some prefer a pill taken once per day, while others find supplements easier. If you’re experiencing depression or anxiety alongside your lupus flares, talk to your doctor about combining Cymbalta with another antidepressant treatment.
Menstrual Cycle and Lupus Flares
It is not uncommon for women with Lupus to experience flares in connection with their menstrual cycle. This can include worsening symptoms as well as the exacerbation of the disease process. There is evidence that hormones may play a role in the severity of lupus flares, though not all experts are convinced. Lupus flares typically last 1-3 weeks in length and improve once menstruation begins again.
Estrogen-based contraceptives should be avoided since they may worsen symptoms. If you are on hormonal therapy such as birth control pills or progesterone injections, speak with your doctor about switching to another type of birth control. And if you take an antidepressant (such as Zoloft) or blood pressure medication (such as Norvasc), talk to your doctor about possible changes in these medications.
Triggers that can cause a Lupus Flare
A person may experience flare ups for any number of reasons. Medications used to treat Lupus are known triggers for exacerbations; this is due to the extreme effect these medications have on dampening the immune system. Certain infections can also lead to flare-ups such as colds or other respiratory infections. Physical activity has been found to be correlated with lower numbers of flares as well, likely because it causes an increase in metabolism that decreases inflammation.
Environmental factors such as extreme temperatures, smoke from fires or too much sunlight have been shown in studies to have the potential for triggering flare ups or worsening existing conditions. Your menstrual cycle may often be cited as a trigger. There does not seem to be evidence of causation between the two conditions. It could be that women who experience flare ups around their period are simply more aware of the symptoms during this time period and therefore notice them more often than at other times.
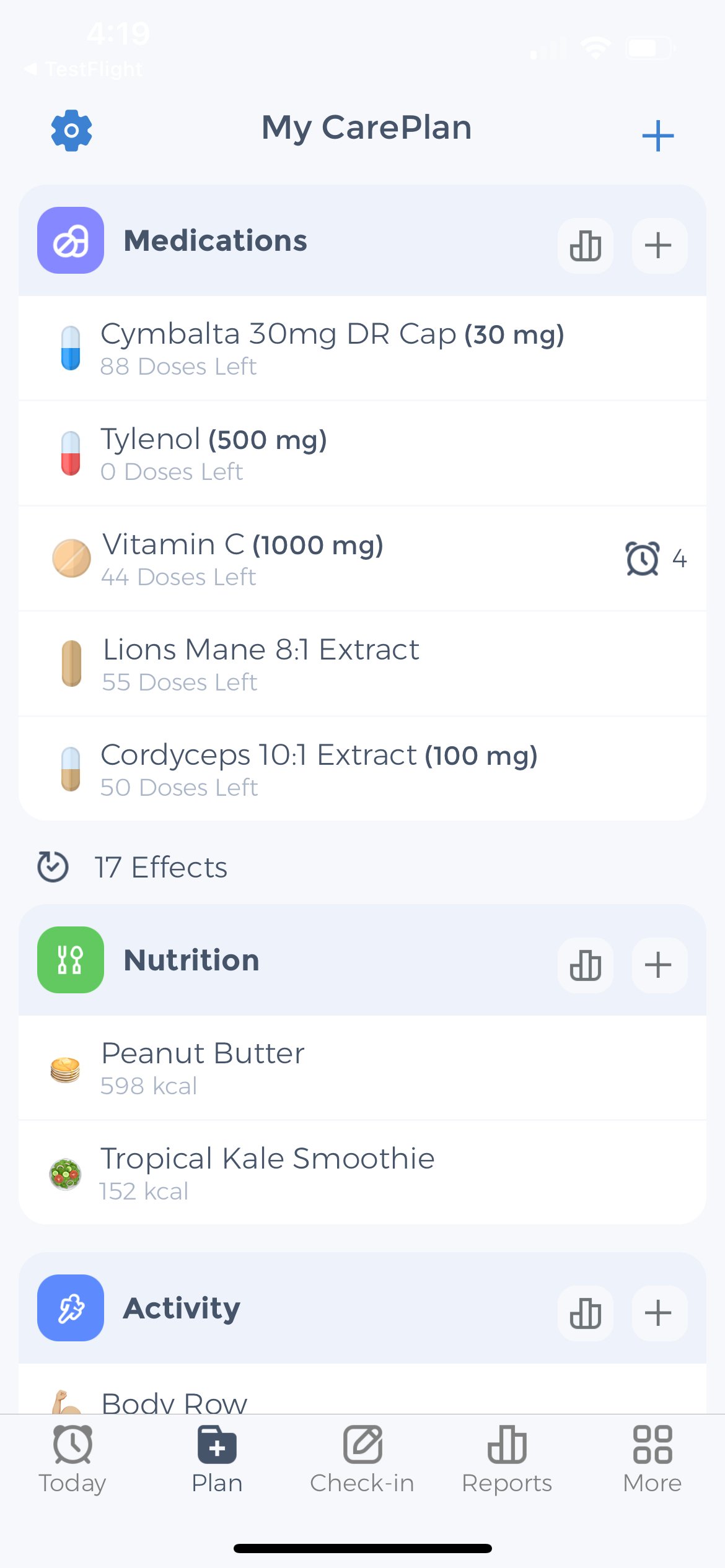
Some people think that using melatonin can cause lupus flare-ups, but research has not supported this claim. More information needs to be gathered before making definitive statements about the relationship between melatonin use and lupus flares. You can always use the CareClinic app to record environmental factors, medications, activities and measurements. Then “compare” them within the app’s chart screen to get a list of correlations that may be your triggers.
Discovering Triggers & Tracking Lupus
The CareClinic app can be used to discover triggers and track Lupus. This is how it works: Download the CareClinic app from the App Store or Google Play. Enter information about your medication, including dosage information, usage frequency, and any notes. Once you’ve entered all of your current meds, add symptoms that you experience often related to your flares.
If you’re already tracking other symptoms on the app, tap on “Check-in” and select Symptoms. Then tap Enter Symptoms or check off those that were already on your list. Select the time frame when each symptom began happening, then add any additional symptoms that may have been associated with those times. You can also add symptom severity to determine which symptoms were more severe for reference. Once done logging your entry, tap “Post Check-in” and see Logs nd charts related to your symptoms to see how your treatment has been progressing.
How long does a lupus flare last
The length of a lupus flare varies from person to person, but they can last up to three weeks. That being said, there are some things you can do that may shorten the amount of time it takes for your flare up to stop. The most important thing is reducing your stress levels by engaging in activities like mindfulness meditation or therapy. The quickest way to reduce the symptoms of a lupus flare is through medication.
These powerful anti-inflammatory drugs rapidly alleviate symptoms like joint pain and muscle aches. Although steroids can effectively treat acute flares, they should be used only when necessary due to their side effects. Such as high blood pressure and weight gain. Additionally, it’s important to note that antibiotics are frequently administered to treat bacterial infections (such as strep throat) triggered by fever during a lupus flare-up.
What is a Lupus fever?
A lupus fever results from inflammation of the brain or central nervous system (CNS). Causing a sudden spike in body temperature. It can be effectively treated with medication and typically does not lead to serious long-term effects. However, if you experience these symptoms for more than a few days, it’s advisable to consult your doctor promptly. If a fever is accompanied by other neurological symptoms, such as headache, nausea, weakness, seizures, or confusion, it may be due to an infection of the meninges surrounding the brain and spinal cord (meningitis) or inflammation of the covering tissue around the heart muscle (pericarditis).
A lupus flare up will typically last about 2 weeks before subsiding on its own. In order to avoid triggering another flare up it’s important to limit sun exposure and stay hydrated. Eating an anti-inflammatory diet rich in vegetables, fruits, whole grains and lean protein will also help ward off flares.
How often do Lupus flares occur
A Lupus flare up can happen anytime at any point in your day or night. They can range from something small like a headache or an upset stomach to a more severe situation. Such as an increased heart rate or hot flashes. Many Lupus flares are usually caused by stress, sun exposure, illness, menstruation cycle, infections etc. It is also possible for certain food products like dairy products or even melatonin supplements to cause a Lupus flare-up as well. There are many methods that one can use to help alleviate the symptoms of their lupus flares from NSAIDs like aspirin and ibuprofen which block the production of prostaglandins (hormones) by the body which triggers inflammation.
To prevent lupus flares, avoiding anything that causes them is key. That includes people who have a lot of different allergies and sensitivities. For example, if you know you have sensitivity to light and pollen then it would be best not to go outside on sunny days or go outside when there’s a lot of pollen in the air. The best way to treat Lupus Flares is with medication but this will depend on what’s causing them as well as what severity they are at currently.
Get additional support
The Lupus Foundation of America (LFA) is a national nonprofit health organization established in 1987. To improve the quality of life for all people affected by lupus through programs of research, education, and advocacy. The LFA provides information about the disease. And its management, support services for people with lupus and their families, and funds research on the causes and treatment of lupus. Clinical trials are also an important part of the LFA’s mission. The LFA has a national network of Lupus Foundation of America-supported clinical trials available to people with lupus. Visit the website for more information on clinical trials and how to find one that might be right for you: www.lupus.org/clinicaltrials.
Managing Daily Life with Lupus Symptoms
There are many questions that come up when it comes to Lupus flare ups. You are now aware of what causes lupus flares, how long they last, if melatonin can cause them, and how to treat them. Lupus flares are periods of time when lupus symptoms get worse for a few days or weeks. Many things can trigger a lupus flare such as: stress, sun exposure, illness, menstruation cycle, infections etc. The best way to prevent lupus flares is by avoiding anything that may trigger them.
Lupus flares can range from something small like a headache or an upset stomach to a more severe situation. Such as an increased heart rate or hot flashes. Many Lupus flares are usually caused by stress, sun exposure, illness, menstruation cycle, infections etc. It is also possible for certain food products like dairy products or even melatonin supplements to cause Lupus flare-ups as well. There are many methods that one can use to help alleviate the symptoms of Lupus from NSAIDs like aspirin and ibuprofen. Luckily managing your medications, and symptoms and discovering triggers can all be done with the help of the CareClinic App which is available for iOS and Android for free. Tap here to give it a try!