Do you ever have difficulty breathing or chronically cough up sputum? Do your usual symptoms get worse when someone is smoking cigarettes around you or even when taking a deep breath? Chronic Obstructive Pulmonary Disease (COPD) affects millions of people worldwide and severely decreases the quality of life of those affected by it. It can be a challenging and frustrating disease to manage, especially when dealing with flare-ups that can be both uncomfortable and dangerous. As someone with COPD, or someone who knows someone with COPD, you know firsthand how important it is to understand this disease and its potential complications.
In this article, we will cover both COPD and its flareups. First, we will discuss the basics of COPD, including what it is, how it develops, who is at risk, and how it’s treated. Then, we will also into COPD flare ups, including what they are, why they occur, and how they can be managed and prevented. Whether you’re living with COPD or caring for someone who is, this article will provide you with valuable information to help you better understand and manage this chronic lung disease.[1][2][3][4]
COPD: The Basics
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease that makes it difficult to breathe. While it comes with many symptoms, such as coughing and difficulty breathing, the long term effect it has on one’s daily life is what makes it such an important condition. The two main types of COPD are chronic bronchitis and emphysema, both of which are characterized by chronic inflammation and narrowing of the airways.
What is COPD
Chronic obstructive pulmonary disease is a long-term lung disease that affects millions of people worldwide. It is typically caused by long-term exposure to irritants such as cigarette smoke, air pollution, and occupational dust and chemicals. COPD gradually damages the airways and lung tissue, making it difficult to breathe.
There are two main types of COPD:
- Chronic bronchitis: Chronic bronchitis is characterized by inflammation and irritation of the bronchial tubes, which are the tubes in which air travels to and from the lungs. People with chronic bronchitis often have a persistent cough and produce excess mucus, which can make it difficult to breathe.
- Emphysema: This type of COPD involves damage to the air sacs in the lungs, which can make it difficult for the lungs to absorb oxygen and release carbon dioxide. People with emphysema often experience shortness of breath and may feel like they can’t catch their breath. This occurs even when they’re at rest, rather than just after an intense workout.
Both types of COPD can cause significant damage to the lungs over time, leading to a decreased quality of life and an increased risk of respiratory infections and other complications. COPD is most commonly caused by long-term exposure to irritants such as secondhand smoke, air pollution, and occupational dust and chemicals. However, keep in mind that this is just a general rule: not everyone who is exposed to these irritants will develop COPD, and some people who have never smoked or been exposed to irritants can still develop the disease.
How does it develop?
COPD develops over time as a result of long-term exposure to irritants such as cigarette smoke, including secondhand smoke, and air pollution. The irritation and inflammation caused by these irritants can damage the airways and lung tissue, leading to the characteristic symptoms common signs of COPD.
To understand how COPD develops in more detail, it’s important to understand that the condition is a result of chronic inflammation and damage to the airways and lung tissue. In healthy lungs, the airways and tiny air sacs called alveoli are flexible and expand easily to allow air to flow in and out. However, in individuals with COPD, the airways and alveoli become inflamed and narrowed, making it harder to breathe.
The inflammation and narrowing of the airways in COPD are caused by an immune response to inhaled irritants, such as cigarette smoke, air pollution, and occupational dust and chemicals. These irritants can trigger an inflammatory response in the lungs, causing the airways to become swollen and producing excess mucus. Over time, the inflammation and mucus production can lead to scarring and permanent damage to the airways and alveoli.
Who is at risk?
There are several risk factors for a person developing COPD. Some of them are listed below.
- Smoking
 or a history of smoking is the primary risk factor for COPD, and long-term exposure to secondhand smoke is the leading cause of the disease.
or a history of smoking is the primary risk factor for COPD, and long-term exposure to secondhand smoke is the leading cause of the disease. - Exposure to occupational dust and chemicals, such as silica, cadmium, and asbestos, can increase the risk of COPD, especially in individuals who work in jobs with high exposure levels.
- Air pollution, both indoor and outdoor, can contribute to the development of COPD.
- Genetic factors can also play a role in COPD risk, as some people may have a genetic predisposition that makes them more susceptible to the disease.
Additionally, certain demographic factors may also increase the risk of COPD, including:
- Age: COPD most commonly affects people over the age of 40, with the risk increasing as a person ages.
- Gender: Women who smoke may be at a greater risk of developing COPD compared to men who smoke.
- Family history: People that have family members that have COPD may have a higher risk of developing the disease.
It’s important to note that while these factors can increase the likelihood of developing COPD, anyone can develop the disease, regardless of their age, gender, or other risk factors. Furthermore, while some of these factors are unavoidable, such as genetics, recognizing the importance of healthy lifestyle factors is important. Lifestyle factors are often overlooked, but limiting or quitting smoking, for example, can severely decrease your risk of getting COPD and decrease symptoms if you the disease.
How is it diagnosed?
To diagnose COPD, a doctor will typically start by taking a detailed medical history, including information on smoking history, exposure to irritants, and any respiratory symptoms. They may also ask about symptoms like a sore throat or trouble sleeping. They will then conduct a physical examination, listening to the patient’s lungs for any wheezing, coughing or crackling sounds.
The most important tool for diagnosing COPD is pulmonary function testing, which involves a series of tests that measure how well the lungs are functioning. These tests include spirometry, which measures how much air a person can exhale in one breath, and a test to measure the diffusion capacity of the lungs, which shows how well oxygen moves from the lungs into the bloodstream.
In addition to these tests, a chest X-ray or CT scan may be used to look for any other warning signs of structural abnormalities in the lungs, such as emphysema or lung cancer.
Overall, a combination of medical history, physical examination, and pulmonary function tests is used to make a diagnosis of COPD and to determine the severity of the disease. Early diagnosis is important to help prevent further damage to the lungs and to improve treatment outcomes.
How is it treated?
While there is no cure for COPD, there are several treatments available to help manage symptoms and slow the progression of the disease. These may include medications such as bronchodilators and steroids, oxygen therapy, and pulmonary rehabilitation. In severe cases, surgery may be necessary to remove damaged lung tissue.
- Bronchodilators are medications that relax the muscles around the airways, making it easier to breathe. They may be taken in pill form or inhaled through a nebulizer or inhaler.
- Steroids are medications that reduce inflammation in the airways, making breathing easier. They may also be taken in pill form or inhaled, like oral corticosteroids.
- Oxygen therapy involves using supplemental oxygen to help ensure that the body is getting enough oxygen. This may involve using a small portable oxygen tank or an oxygen concentrator, which removes nitrogen from the air and delivers oxygen-rich air to the patient.
- Pulmonary rehabilitation is a comprehensive program that includes exercise training, breathing techniques, and education on COPD management. This type of therapy can help improve lung function, increase exercise tolerance, and improve quality of life.
- In severe cases of COPD, surgery may be necessary to remove damaged lung tissue. This procedure, known as lung volume reduction surgery, can help improve lung function and reduce symptoms.
Treatment plans will vary depending on the individual and the severity of their COPD. A healthcare provider will work with the family members and patient to create a personalized treatment plan.
COPD Flare Ups: Dangerous COPD Exacerbations
 A COPD flare up, also known as an exacerbation, is a sudden worsening of COPD symptoms that can last for days or even weeks. During a flare up, a person may experience increased breathing difficulties, coughing, wheezing, chest pain and tightness, and more mucus- production. Flare ups can be caused by a variety of factors and can range in severity from mild to life-threatening.
A COPD flare up, also known as an exacerbation, is a sudden worsening of COPD symptoms that can last for days or even weeks. During a flare up, a person may experience increased breathing difficulties, coughing, wheezing, chest pain and tightness, and more mucus- production. Flare ups can be caused by a variety of factors and can range in severity from mild to life-threatening.
Why do COPD flare ups occur?
A COPD flare up can occur for several reasons, including exposure to irritants such as cigarette smoke or air pollution, respiratory infections such as the flu or pneumonia, changes in weather, and even emotional stress. In some cases, the cause of a flare up may be unknown.
What are some common triggers of COPD flare ups?
A COPD flare up can be triggered by a variety of COPD triggers, some of which are listed below:
- Exposure to cigarette smoke or other irritants: The leading COPD triggers are smoking and other irritants. Continued exposure to cigarette smoke can worsen COPD symptoms and trigger flare-ups. Other irritants, such as air pollution and workplace chemicals, can also contribute to the development and exacerbation of COPD.
- Respiratory infections such as the flu or pneumonia: Infections of the respiratory tract can irritate the airways and lungs, leading to inflammation and worsening of COPD symptoms.
- Changes in weather or air quality: Changes in temperature, humidity, and air pollution levels can also trigger COPD flare-ups. Cold air, high humidity, and air pollution can all make breathing more difficult for people with COPD.
- Failure to take prescribed medications: Regular use of medications such as bronchodilators and inhaled steroids can help manage COPD symptoms and prevent flare-ups. However, failing to take prescribed medications or not using them correctly can lead to worsening of symptoms and increased risk of flare-ups.
- Emotional stress or anxiety: Emotional stress and anxiety can also trigger COPD flare-ups. Stress can cause the body to release hormones that can increase inflammation and worsen COPD symptoms.
- Excessive physical activity: While regular exercise is important for people with COPD, overexertion can lead to fatigue and exacerbation of symptoms.
- Gastroesophageal reflux disease (GERD): GERD is a condition in which stomach acid backs up into the esophagus, causing irritation and inflammation. In some cases, GERD can worsen COPD symptoms and trigger flare-ups.
How you can prevent COPD flare ups
While it may not be possible to completely prevent a COPD flare up, there are steps that can be taken to minimize the risk, including:
- Avoiding exposure to cigarette smoke and other irritants. The most important step in preventing COPD flare ups is to avoid exposure to cigarette smoke and other irritants such as air pollution, dust, and chemicals. If you smoke, quitting is the best thing you can do to slow the progression of the disease and reduce the frequency and severity of flare ups.
- Practicing good hand hygiene and avoiding close contact with sick individuals. Respiratory infections such as the flu and pneumonia can trigger COPD flare ups.
- Getting vaccinated against the flu and pneumonia. Vaccination against the flu and pneumonia can help reduce the risk of respiratory infections and prevent flare ups. Talk to your doctor about getting vaccinated if you have not already done so.
- Engaging in regular exercise to improve lung function. Regular exercise can help improve lung function and reduce the risk of flare ups.
- Managing stress through relaxation techniques such as meditation or deep breath exercises. Stress can be a trigger for COPD flare ups. Engaging in relaxation techniques such as meditation or deep breathing exercises can help reduce stress and improve breathing.
Managing COPD flare ups
It’s important to remember that the severity of symptoms can vary from person to person. Mild flare ups may be managed with rest and increased use of prescribed medications. As well as breathing exercises to help improve lung function. However, severe a flare up causing severe shortness of breath may require hospitalization and more intensive treatment. Such as oxygen therapy, bronchodilators, and steroids.
It’s important for individuals with COPD to work closely with their healthcare providers. To develop a plan for managing flare ups that takes into account their individual symptoms and needs. By staying on top of symptoms and following a well-rounded treatment plan with healthcare provider, individuals with COPD can help minimize the impact of flare ups and maintain a better quality of life.
When can COPD flare ups become dangerous?
A COPD exacerbation, if not properly managed, can cause irreversible lung damage and be potentially life-threatening. Therefore, it is crucial to seek immediate emergency medical care if you experience severe symptoms such as:
- Severe breathing problems
- Confusion or changes in mental status
- Blue lips or fingers (cyanosis)
- Chest pain or tightness
These symptoms may indicate that you are not getting enough oxygen and that your condition has worsened. In addition, if the symptoms of a flare up do not improve or worsen despite treatment, it is important to consult a healthcare professional. They can evaluate the underlying cause of worsening symptoms and adjust your treatment plan accordingly.[5][6][7]
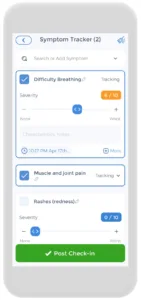
Using an App to Track COPD Flare Ups
 Having a COPD action plan is crucial, and the CareClinic app can help with that. You can use the app as your journal. Just go to the diary section of the app and enter your daily symptoms, medications, and other triggers, as they occur. There are also specific sections on the app to track each of these. This can help you be away of early warning signs. Next time you visit the doctor’s office, this information will be handy in your pocket.
Having a COPD action plan is crucial, and the CareClinic app can help with that. You can use the app as your journal. Just go to the diary section of the app and enter your daily symptoms, medications, and other triggers, as they occur. There are also specific sections on the app to track each of these. This can help you be away of early warning signs. Next time you visit the doctor’s office, this information will be handy in your pocket.
The app also has a medication section. Where you can precisely track the doses you are taking and receive reminders on when to take each medication. We know how difficult but important keeping track of your medications. So we hope to make it as easy and streamlined as possible.
Conclusion
COPD flare ups can be a frightening and debilitating experience for those who suffer from this chronic lung disease. While flare ups are a common occurrence in COPD, they can often be prevented through careful management of the disease and avoidance of triggers. It is important to seek medical attention. If symptoms become severe or do not improve with treatment, as flare ups can become dangerous if left untreated. With the right care and support, individuals with COPD can continue to lead fulfilling and active lives. By working closely with their healthcare providers and taking steps to manage the disease, they can better manage flare ups and minimize their impact on daily life.
Sources:
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. 2022. https://goldcopd.org/2022-gold-reports/.
- American Lung Association. Chronic Obstructive Pulmonary Disease (COPD) Fact Sheet. 2021. https://www.lung.org/lung-health-diseases/lung-disease-lookup/copd/learn-about-copd.
- Wedzicha JA, Miravitlles M, Hurst JR, Calverley PMA, Albert RK, Anzueto A, et al. Management of COPD exacerbations: a European Respiratory Society/American Thoracic Society guideline. Eur Respir J. 2017;49(3):1600791. doi:10.1183/13993003.00791-2016
- Seemungal TA, Donaldson GC, Paul EA, Bestall JC, Jeffries DJ, Wedzicha JA. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157(5 Pt 1):1418-1422. doi:10.1164/ajrccm.157.5.9709032
References
- “Prevent and Recover from a COPD Exacerbation or Flare Up | American Lung Association”. https://www.lung.org/lung-health-diseases/lung-disease-lookup/copd/living-with-copd/prevent-flare-ups
- “COPD flare-ups: MedlinePlus Medical Encyclopedia”. https://medlineplus.gov/ency/patientinstructions/000698.htm
- “What are COPD flare-ups and what can I do to prevent them? – Canada.ca”. https://www.canada.ca/en/public-health/services/chronic-diseases/chronic-respiratory-diseases/what-copd-flare-what-prevent-them.html
- “COPD Flare-Ups: Warning Signs, Prevention, and Management | COPD Foundation”. https://www.copdfoundation.org/COPD360social/Community/COPD-Digest/Article/2107/COPD-Flare-Ups-Warning-Signs-Prevention-and-Management.aspx
- “COPD exacerbations: defining their cause and prevention – The Lancet”. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2807%2961382-8/fulltext
- “Acute exacerbation of chronic obstructive pulmonary disease – Etiology | BMJ Best Practice US”. https://bestpractice.bmj.com/topics/en-us/8/aetiology
- “COPD Exacerbation | University of Utah Health”. https://healthcare.utah.edu/pulmonary/conditions/copd/exacerbation
- “COPD – Living With | NHLBI, NIH”. https://www.nhlbi.nih.gov/health/copd/living-with
- “How to Exercise When You Have COPD”. https://time.com/7097021/copd-exercise-recommendations/