POTS, or postural orthostatic tachycardia syndrome, is a condition that affects the autonomic nervous system. The autonomic nervous system controls many of the body’s automatic functions, such as heart rate, blood pressure, and digestion. People with POTS have trouble regulating their blood pressure and heart rate when they stand up, which can cause lightheadedness, dizziness, fainting, and fatigue. A POTS flare-up is a period when symptoms are worse than usual.
The trouble starts when you stand up. Normally, when you do, gravity causes blood to pool in your leg veins. This pooling makes it harder for your heart to pump blood back up to your brain. To make up for this drop in blood pressure, your autonomic nervous system signals your heart to beat faster and narrows the arteries that carry blood to your brain. In people with Postural Orthostatic Tachycardia Syndrome, these compensatory mechanisms don’t work properly. As a result, blood pressure falls, and not enough blood reaches the brain. This can cause lightheadedness, dizziness, fainting, and fatigue.[1]
Table of Contents
- What causes POTS?
- How do you get a proper diagnosis?
- What is the long-term outlook for people with POTS?
- What are the symptoms of POTS?
- What are common treatments for POTS?
- What are some tips for managing POTS?
- What causes a POTS Flare-Up?
- What does a POTS flare feel like?
- How can you prevent a POTS flare up?
- What should you do during a POTS Flare Up?
- What if your POTS symptoms are getting worse?
- How To Record POTS Symptoms & Flare-Ups
- The Tilt Table Test
- POTS vs OTS
- What kind of diet is recommended for postural orthostatic tachycardia syndrome?
- How do POTS patients develop this chronic health condition?
- Types of POTS diagnosis?
- How long does a POTS episode last?
- Can POTS symptoms come and go?
- What are the long-term effects of Postural Orthostatic Tachycardia Syndrome?
- Managing Your POTS Flare Up
What causes POTS?
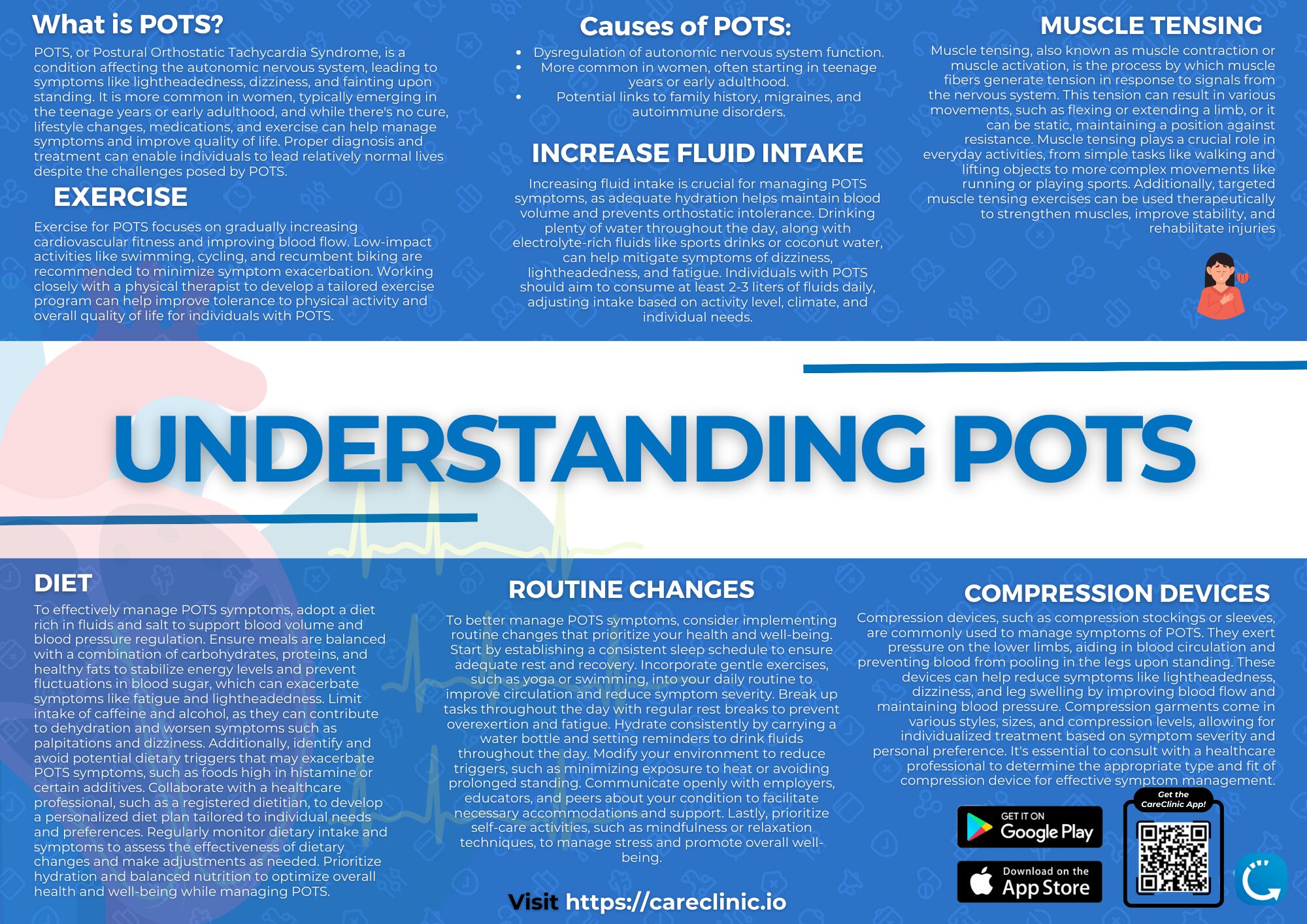
The exact cause is unknown, but it is thought to be due to a problem with the autonomic nervous system. It is more common in women, and often starts in the teenage years or early adulthood. It is estimated that POTS affects between 1 and 3 million Americans. Additionally, there does not seem to be a link to family history, but some research suggests that POTS may be more common in families with a history of migraines or autoimmune disorders such as lupus or multiple sclerosis.[2][3][4]
How do you get a proper diagnosis?
If you think you may have POTS, it is important to see a doctor who is familiar with the condition. Several tests can be done to diagnose POTS. Once diagnosed, several treatments can help improve symptoms and quality of life.
There is no cure for POTS, but treatments can help improve symptoms. These treatments can be divided into three categories:
- Lifestyle changes: These include increasing salt and water intake, avoiding prolonged standing, and wearing compression stockings.
- Medications: There are several medications that can help improve symptoms, such as beta-blockers, diuretics, and fludrocortisone.
- Exercise: Exercise is an important part of treatment for POTS. A physical therapist can help create an exercise program that is tailored to your needs and abilities.
Lifestyle changes, medications, and exercise can all help improve symptoms of Postural Orthostatic Tachycardia Syndrome. It is important to work with a doctor to find the best treatment plan for you.[5][6][7]
What is the long-term outlook for people with POTS?
The long-term outlook for people with POTS is generally good. With proper treatment, most people can live normal, active lives. A small percentage of people with POTS develop a more severe form of the condition called chronic orthostatic intolerance (OI). OI can lead to disability and is more difficult to treat.
Even with proper treatment, some people with Postural Orthostatic Tachycardia Syndrome continue to have symptoms. For these people, symptom management is the focus of treatment which the CareClinic app can help manage.
What are the symptoms of POTS?
The most common symptom is fatigue. Other symptoms include:
- Lightheadedness (caused by low blood pressure)
- Dizziness (also caused by low blood pressure)
- Fainting (caused by low blood pressure)
- Brain fog (difficulty thinking clearly, see how you can get rid of it here.)
- Headaches (can be caused by low blood pressure or dehydration)
- Heart palpitations (abnormal heart rhythms)
- Shortness of breath (can be caused by low blood pressure or deconditioning)
- Sweating (can be caused by increased heart rate or anxiety)
- Nausea (can be caused by low blood pressure or anxiety)
- Exercise intolerance (fatigue with activity)
- Sleep problems (difficulty falling or staying asleep, or unrefreshing sleep)
- Anxiety and depression (can be caused by chronic symptoms)
These symptoms can vary from person to person and may come and go. They may be worse when you are standing up, after eating, or during exercise. They may also be worse when you are under stress.[8][9][10][11][12][13][14]
What are common treatments for POTS?
There is no cure for POTS, but there are treatments that can help lessen the symptoms. Common treatments include increasing salt and water intake to help with blood volume issues. Wearing compression stockings helps with blood pooling in the legs. Exercise training helps increase blood flow and reduce fatigue. Medications to help with symptoms such as nausea, dizziness, and fainting.[15]
What are some tips for managing POTS?
There are a few things that can help you manage your POTS and keep your symptoms under control: Stay hydrated by drinking plenty of fluids, especially water. Avoid standing for long periods of time. If you have to stand, take breaks often and move around. Exercise regularly to help increase blood flow and reduce fatigue. Wear loose-fitting clothing and avoid clothes that are tight around the waist or chest. Elevate your head and legs when you sleep. Avoid hot showers or baths, saunas, or hot tubs. Avoid caffeine and alcohol. Manage stress with relaxation techniques such as yoga or meditation.[16][17][18][19][20][21]
What causes a POTS Flare-Up?
POTS flare ups can be caused by many things, including stress, illness, certain medications, and changes in weather or altitude. People with POTS often don’t know what triggers their flare-ups, but there are some things that can be done to prevent or lessen the symptoms. Treatment for POTS flare-ups usually involves managing symptoms and trying to identify and avoid triggers. In severe cases, medical help may be needed.[22][23][24][25][26]
What does a POTS flare feel like?
People with POTS can experience different symptoms during a flare-up, but some of the more common ones are fatigue, brain fog, lightheadedness, dizziness, fainting, headaches, and gastrointestinal problems. These symptoms can make it hard to do everyday activities. As an example POTS patients find it hard to exercise, or even sleep because of the symptoms. The quality of life during a POTS flare can be significantly decreased.
How can you prevent a POTS flare up?
There is no one-size-fits-all answer to preventing POTS flare-ups, but there are some general things that can help. Staying hydrated, eating a healthy diet, and getting enough exercise are all important for keeping the autonomic nervous system functioning properly.
Avoiding triggers is also key. If you know what causes your flare-ups, try to avoid those things. If you’re not sure what triggers your flare-ups, keeping a symptom diary can help you identify patterns. The CareClinic helps you determine your triggers and can even alert you of upcoming flare-ups based on historical data. Read on to learn more about how to track all aspects of your treatment, and then monitor and act on key findings from the CareClinic App.
Can stress trigger a POTS episode and why?
Stress is a common trigger for POTS episodes. When you’re stressed, your body releases hormones that can affect the autonomic nervous system. This can lead to symptoms like increased heart rate, sweating, and headaches. For people with POTS, stress can also trigger a drop in blood pressure, which can cause lightheadedness and dizziness.[29][30][31][32][33]
What should you do during a POTS Flare Up?
If you have a POTS flare-up, the first thing you should do is sit or lie down. This will help your blood pressure and heart rate stabilize. Drink plenty of fluids, especially water, and avoid caffeine and alcohol. If you’re feeling dizzy or lightheaded, try to raise your head higher than your heart. You can do this by propping yourself up on pillows or sitting in a recliner. Taking a hot bath or shower can also help. If your symptoms are severe, call 911 or go to the emergency room.
POTS flare-ups can be unpredictable and frustrating, but there are things you can do to manage your symptoms and prevent triggers. With the CareClinic app, you can track all aspects of your health in one place so you can identify patterns and get the information you need to make informed decisions about your care.[34][35]
What if your POTS symptoms are getting worse?
If your POTS symptoms are getting worse, it’s important to talk to your doctor. They may need to adjust your medication or recommend other treatment options. In some cases, hospitalization may be necessary. You may need your treatment adjusted, or you may already be taking the following medications:
- Beta blockers: help to slow the heart rate and improve blood flow
- ACE inhibitors: help to lower blood pressure and improve blood flow
- Diuretics: help to reduce fluid retention and improve blood flow
- SSRIs: help to improve mood and relieve anxiety
- IVIG: helps to boost the immune system
- Hospitalization may be necessary if you:
- Have a severe drop in blood pressure
- Have a heart rate that is too high or too low
- Have difficulty breathing
- Are dehydrated
- Have an infection
- Are pregnant and have Postural Orthostatic Tachycardia Syndrome
If you have any of these symptoms, call 911 or go to the nearest emergency room.[36][37][38]
How To Record POTS Symptoms & Flare-Ups
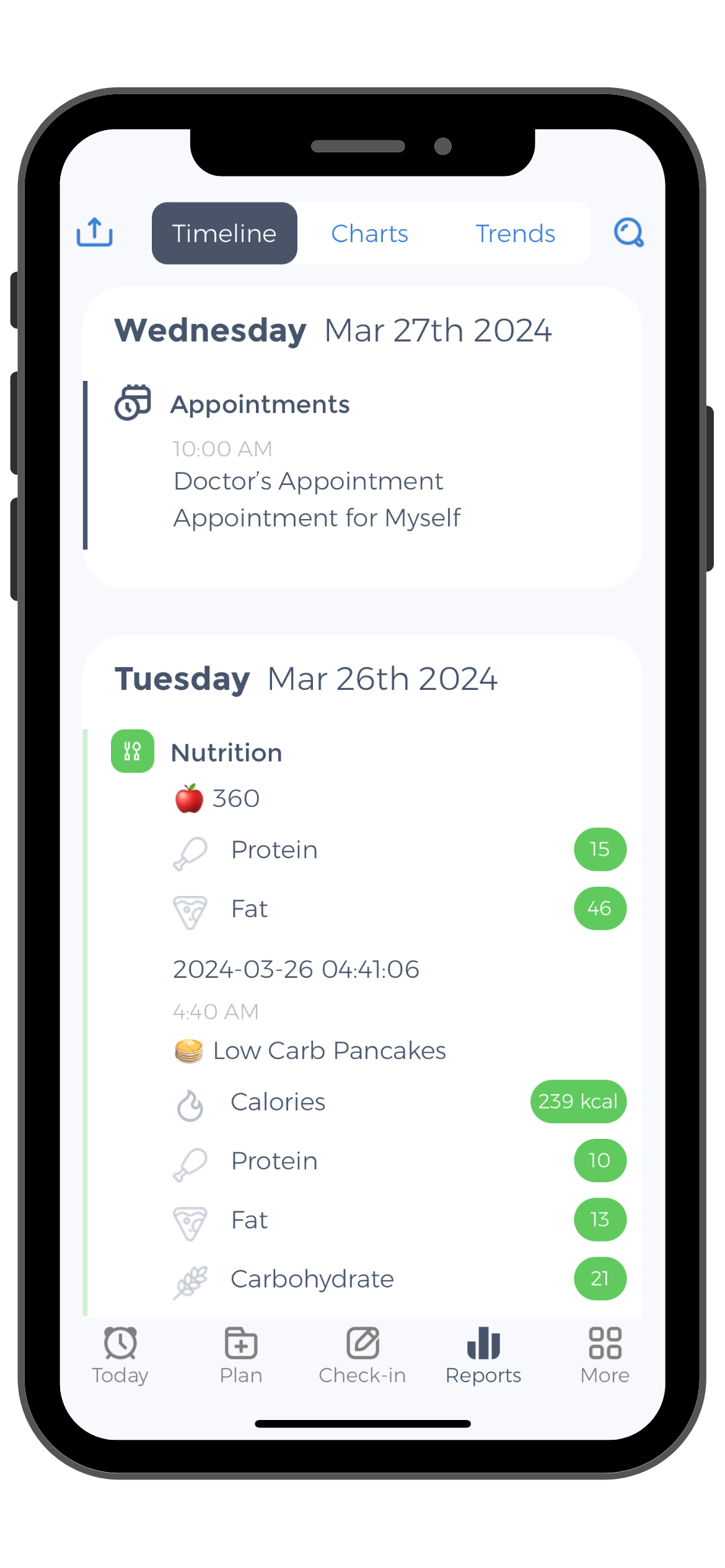
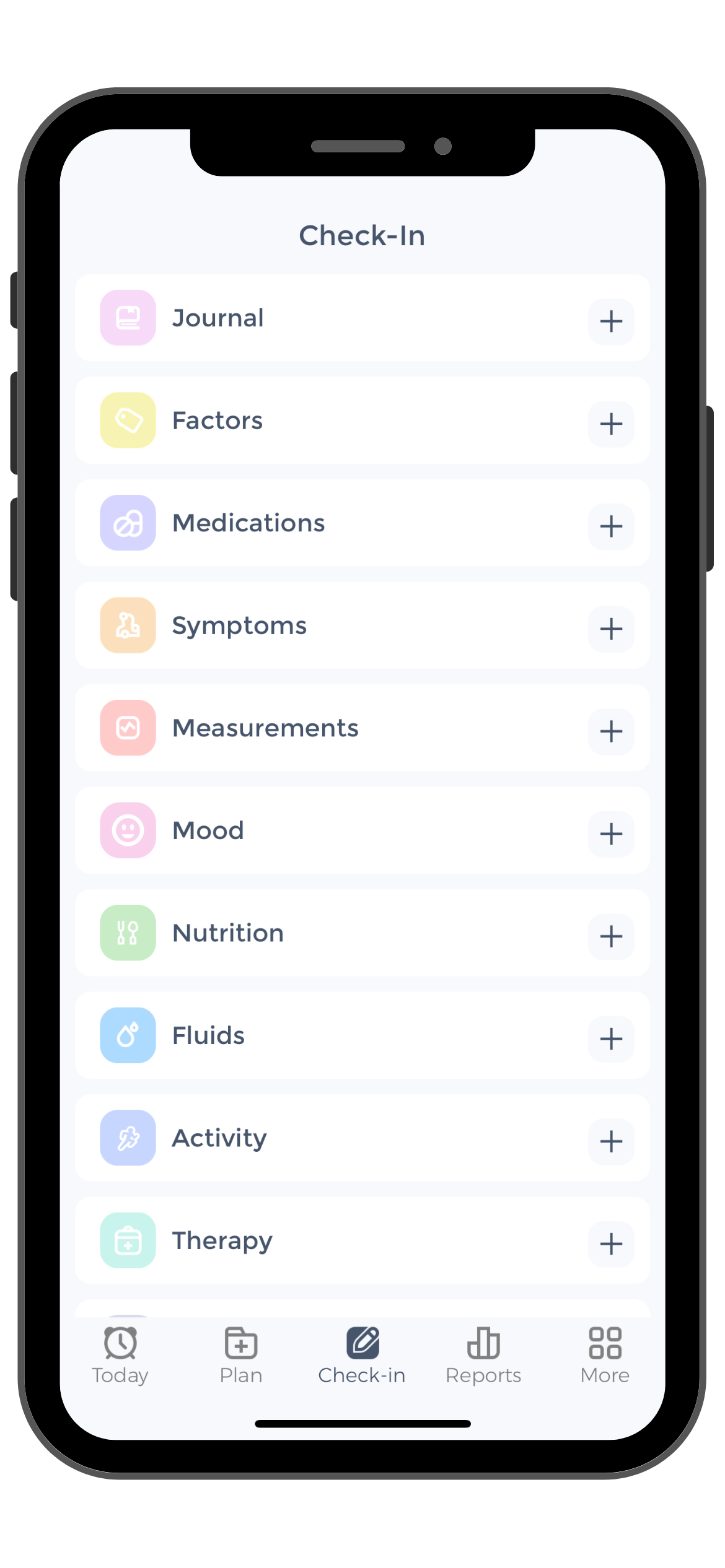
The first step is to download the free CareClinic app from the App Store or Google Play. Once you have the app, create an account and then log in.
Once you’re logged in, you’ll see the main dashboard. Here, you can see all of your upcoming appointments, medications, and health goals. To track your POTS symptoms, click on the “Symptoms Tracker” or Check-in button at the bottom of the screen.
On the symptoms tracker, you’ll see a list of common POTS symptoms. Select all of the symptoms that you’re currently experiencing from the dropdown menu. Once you’ve added all of your symptoms to the tracker, you’ll then be able to add more details about your symptoms, such as how long you’ve been experiencing them, how severe they are, and any other notes that you want to include. Once you’re done, click on the “Post Check-in” button.
How to Use the Check-In Feature
You can either post a check-in or add other modalities to your check-in such as any medications or health measurements you may want to track. If you’re posting a medication, start by clicking on the “Medication Tracker” button. This will bring up a list of common medications used to treat POTS. If you don’t see your medication on the list, you can type it in manually. Once you’ve added all of your medications, tap on “Post Check-in”.
You can view all of your recorded symptoms by clicking on the “Reports” tab at the bottom of the screen. Here, you can see a list of all of your recorded symptoms, as well as when they occurred. You can also see a graph of your symptoms over time. If you want to share your reports with your doctor, you can do so by clicking on the “Share” button to add them as a caregiver or you can export your data so you can print it as well.
The CareClinic app is a helpful tool for managing POTS symptoms and flare-ups. By tracking all aspects of your health in one place, you can identify patterns and get the information you need to make informed decisions about your care. One additional beneficial functionality is the “Correlations” functionality which is rendered when you compare two different modalities such as Symptoms to Medications or Activity to Medications.
You’ll be provided with a list of positive and negative correlations, such as “Whenever you engage in x activity, your symptoms tend to get worse.” and be provided how strong that correlation is. It really seems like magic but it using statistical analysis to help you quickly determine what may be a potential trigger for your flares.
The Tilt Table Test
The Tilt Table Test is a diagnostic tool used to assess the cause of dizziness and fainting. It is performed by lying on a table that tilts you from a horizontal to a vertical position. The test helps to diagnose dysautonomia, which is the abnormal functioning of the autonomic nervous system. This test can also be used to diagnose other conditions that may cause dizziness or fainting, such as heart arrhythmias.
To prepare for the test, you should wear loose-fitting clothing and avoid eating or drinking for at least two hours before the test. You should also avoid smoking and taking any medications that can affect your blood pressure, such as beta-blockers.
During the test, you will be connected to a heart monitor, and your blood pressure and heart rate will be monitored while you lie on the table. The table will then be tilted to a vertical position for five minutes. You may feel lightheaded or dizzy during this time, but it is important to stay still. After five minutes, the table will be returned to the horizontal position, and you will be monitored for another 30 minutes.
The results of the test will help your doctor diagnose or rule out dysautonomia or other conditions that may be causing your symptoms. If you are diagnosed with dysautonomia, there are treatments available that can help to improve your symptoms.
The CareClinic app can be a helpful tool in managing your dysautonomia and any other chronic illness. By tracking all aspects of your health in one place, you can identify patterns and get the information you need to make informed decisions about your care.[39][40][41]
POTS vs OTS
POTS and OTS are both forms of dysautonomia, but they have different causes. The POTS is caused by abnormal functioning of the autonomic nervous system, while OTS is caused by a structural abnormality in the heart. POTS can be treated with medications and lifestyle changes, while OTS requires surgery to correct the structural abnormality.
What kind of diet is recommended for postural orthostatic tachycardia syndrome?
 There is no specific diet that is recommended for postural orthostatic tachycardia syndrome (POTS), but there are some general dietary guidelines that may help to improve symptoms. These include avoiding triggers such as caffeine, alcohol, and large meals; eating small, frequent meals; and increasing your intake of salt and fluids. You should also avoid lying down for at least two hours after eating. These dietary changes may help to improve your symptoms and help you to better manage your condition.
There is no specific diet that is recommended for postural orthostatic tachycardia syndrome (POTS), but there are some general dietary guidelines that may help to improve symptoms. These include avoiding triggers such as caffeine, alcohol, and large meals; eating small, frequent meals; and increasing your intake of salt and fluids. You should also avoid lying down for at least two hours after eating. These dietary changes may help to improve your symptoms and help you to better manage your condition.
To track your sodium intake with CareClinic, you can create a custom measurement in the CareClinic app. To do this, go to the “Measurements” in the check-in screen and click on the “+” icon. Give your measurement a name (e.g. “Sodium Intake“). You can then set the goals for your daily sodium intake and start tracking! The measurement unit for sodium should be in “mg”.
Why is salty food recommended for POTS?
Salty food is recommended for POTS because it can help to increase blood volume and blood pressure. This can be helpful in managing symptoms such as lightheadedness, dizziness, and fatigue. It is important to talk to your doctor before making any changes to your diet, as some people with POTS may need to limit their sodium intake. Salt tablets are also available by prescription for people with POTS.
What to do if POTS symptoms keep getting worse?
If your symptoms are getting worse, it is important to talk to your doctor. There are a number of different treatment options available, and your doctor will be able to help you find the best one for you. In some cases, medication may be necessary to help control your symptoms. In other cases, physical therapy or lifestyle changes may be recommended.
If you are tracking your symptoms with the CareClinic app, you can use the “Trends” feature to see how your symptoms have changed over time. To do this, go to the “Check-in” screen and click on the “Trends” button. Here, you will be able to see a graph of your symptoms over time. If you notice that your symptoms are getting worse, be sure to talk to your doctor about it![42][43][44]
How do POTS patients develop this chronic health condition?
There are many possible causes of POTS, and doctors often cannot determine the exact cause for an individual patient. However, some possible causes include:
- Autoimmune disorders: Some patients with POTS have underlying autoimmune disorders such as lupus or Sjogren’s syndrome.
- Nerve damage: Damage to the autonomic nervous system (which controls involuntary body functions) can lead to Postural Orthostatic Tachycardia Syndrome. This damage can be caused by physical trauma, infection, or certain medications.
- Problems with blood vessels: Some patients with POTS have abnormalities in the blood vessels that return blood from the legs back to the heart. This can cause pooling of blood in the legs and low blood pressure when standing.
- Dehydration: Dehydration can cause or worsen POTS symptoms.
- Hormone problems: Changes in hormone levels, such as during pregnancy or puberty, can trigger or worsen POTS symptoms.
- Mitral valve prolapse: This is a condition in which the valve between the left atrium and left ventricle of the heart does not close properly. It is thought to be a cause of POTS in some patients.
- Other medical conditions: Some other medical conditions, such as diabetes, thyroid disease, and sleep apnea, can also cause or contribute to POTS.
Types of POTS diagnosis?
There are several different types of POTS, each with its own set of symptoms and causes. The most common types of POTS are neuropathic POTS, which is caused by damage to the nervous system, and hyperadrenergic POTS, which is characterized by increased levels of norepinephrine. Other types of POTS include idiopathic POTS, which has no known cause, and secondary POTS, which is caused by another condition such as diabetes or pregnancy.
Hypovolemic pots, which are low blood volume, can also occur. Low blood volume can be due to dehydration from not drinking enough fluids or from severe diarrhea or vomiting. It can also be caused by blood loss, such as from heavy menstrual bleeding or a gastrointestinal bleed.
What is the difference between POTS and orthostatic hypotension?
POTS and orthostatic hypotension are both forms of dysautonomia, but they have different symptoms. POTS is characterized by an increase in heart rate when standing, while orthostatic hypotension is characterized by a drop in blood pressure when standing. Both conditions can cause symptoms such as lightheadedness, dizziness, and fatigue. POTS can be treated with medications and lifestyle changes, while orthostatic hypotension may require more aggressive treatment such as IV fluids or blood pressure medications.
What is secondary POTS?
Secondary POTS is Postural Orthostatic Tachycardia Syndrome, which is caused by another underlying medical condition. The most common cause of secondary POTS is diabetes. Other causes include:
- Autoimmune disorders
- Nerve damage
- Problems with blood vessels
- Hormone problems
- Mitral valve prolapse
- Other medical conditions
- What is hyperadrenergic POTS?
Hyperadrenergic POTS is a form of POTS that is characterized by increased levels of norepinephrine. Norepinephrine is a hormone that is released in response to stress. People with hyperadrenergic POTS may have symptoms such as anxiety, palpitations, and sweating. Treatment for hyperadrenergic POTS may include medications such as beta-blockers or calcium channel blockers. Lifestyle changes such as stress reduction and increased salt and fluid intake may also be helpful.[48][49][50]
How long does a POTS episode last?
The length of a POTS episode can vary from patient to patient. Some patients have frequent episodes that last for several days or weeks, while others may only have occasional episodes that last for a few hours.
Can POTS symptoms come and go?
POTS symptoms can come and go. Some patients may have symptom-free periods for months or years between episodes, while others may have daily symptoms.
What are POTS seizures?
POTS seizures are a type of seizure that can occur in patients with POTS. These seizures are typically brief and may cause shaking, sweating, and dizziness. They do not typically cause loss of consciousness.
Can these symptoms cause neurological problems or damage?
There is no evidence that POTS causes neurological problems or damage. However, some patients with POTS may also have other medical conditions that can cause these problems.[51][52]
What are the long-term effects of Postural Orthostatic Tachycardia Syndrome?
The long-term effects of POTS can vary depending on the severity of symptoms and how well the condition is controlled. Some patients may experience fatigue, fainting episodes, difficulty with exercise or daily activities, and decreased quality of life. In severe cases, POTS can lead to heart failure or stroke. However, many patients with POTS are able to manage their symptoms and live normal, active lives.
Is there a link between chronic fatigue and POTS?
There is no clear link between chronic fatigue and POTS. However, many patients with POTS do experience fatigue as a symptom. Additionally, some patients with chronic fatigue syndrome (CFS) may also have POTS. More research is needed to determine if there is a connection between these two conditions. The best way to manage fatigue may just be to limit activity during symptom flare-ups and to focus on getting enough rest.[53][54][55]
Managing Your POTS Flare Up
 Postural Orthostatic Tachycardia Syndrome (POTS) is a condition that can cause lightheadedness, dizziness, and fatigue. It is caused by a drop in blood pressure when standing. POTS can be treated with medications and lifestyle changes. Secondary POTS is POTS that is caused by another underlying condition, such as diabetes. Hyperadrenergic POTS is a form of POTS characterized by increased levels of norepinephrine. Symptoms of POTS can come and go and may last for days or weeks. There is no evidence that POTS causes neurological problems or damage. The long-term effects of POTS can vary depending on the severity of the symptoms. There is no clear link between chronic fatigue and POTS, but many patients with POTS do experience fatigue.
Postural Orthostatic Tachycardia Syndrome (POTS) is a condition that can cause lightheadedness, dizziness, and fatigue. It is caused by a drop in blood pressure when standing. POTS can be treated with medications and lifestyle changes. Secondary POTS is POTS that is caused by another underlying condition, such as diabetes. Hyperadrenergic POTS is a form of POTS characterized by increased levels of norepinephrine. Symptoms of POTS can come and go and may last for days or weeks. There is no evidence that POTS causes neurological problems or damage. The long-term effects of POTS can vary depending on the severity of the symptoms. There is no clear link between chronic fatigue and POTS, but many patients with POTS do experience fatigue.
The CareClinic app is a great way to keep track of your POTS symptoms and flare-ups. You can use the app to record your symptoms, medications, and appointments. The app can also help you track your progress and share information with your doctor. You can download it now for Android or iOS by tapping the banner below.[56][57]
References
- “POTS: Causes, Symptoms, Diagnosis & Treatment”. https://my.clevelandclinic.org/health/diseases/16560-postural-orthostatic-tachycardia-syndrome-pots
- “POTS: Understanding Symptoms, Causes, and Treatment – Open Medicine Foundation”. https://www.omf.ong/what-is-pots/
- “Postural orthostatic tachycardia syndrome”. https://en.wikipedia.org/wiki/Postural_orthostatic_tachycardia_syndrome
- “Navigating Complexity in Postural Orthostatic Tachycardia Syndrome – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC11352109/
- “Postural Tachycardia Syndrome (POTS) | Circulation”. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.112.144501
- “Treatment Strategies for Patients With Postural Orthostatic Tachycardia Syndrome – Decisions in Dentistry”. https://decisionsindentistry.com/article/treatment-strategies-for-patients-with-postural-orthostatic-tachycardia-syndrome/
- “Exercise and non-pharmacological treatment of POTS – PubMed”. https://pubmed.ncbi.nlm.nih.gov/30001836/
- “Recognizing POTS | NIH News in Health”. https://newsinhealth.nih.gov/2023/09/recognizing-pots
- “Postural Tachycardia Syndrome (POTS) | National Institute of Neurological Disorders and Stroke”. https://www.ninds.nih.gov/health-information/disorders/postural-tachycardia-syndrome-pots
- “PoTS: what is postural tachycardia syndrome? – BHF”. https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/ask-the-experts/pots
- “Postural orthostatic tachycardia syndrome (PoTS) | NHS inform”. https://www.nhsinform.scot/long-covid/postural-orthostatic-tachycardia-syndrome-pots/
- “POTS Symptoms — Awareness for POTSies”. https://www.awarenessforpotsies.org/pots-symptoms
- “Postural Orthostatic Tachycardia Syndrome (POTS) | Chiari Fund”. https://www.chiarifund.org/disorders/postural-orthostatic-tachycardia-syndrome-%28pots%29
- “Symptoms – POTS AWARENESS”. https://www.potsawareness.org/symptoms.html
- “Diagnosis and management of postural orthostatic tachycardia syndrome – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC8920526/
- “Nursing made Incredibly Easy”. https://journals.lww.com/nursingmadeincrediblyeasy/fulltext/2020/07000/dysautonomia__getting_a_handle_on_pots.4.aspx
- “12 Lifestyle Modifications which work in POTS – Dr Sanjay Gupta Cardiologist”. https://drsanjayguptacardiologist.com/blog/12-lifesyle-modifications-which-work-in-pots/
- “7 tips for POTS Postural Orthostatic Tachycardia Syndrome”. https://internationalpain.org/7-tips-for-living-with-pots/
- “Managing POTS: Simple Lifestyle Changes for Improved Health — Ultima Replenisher”. https://www.ultimareplenisher.com/blogs/blog/simple-lifestyle-tips-to-help-manage-pots
- “Living with Postural Orthostatic Tachycardia Syndrome (POTS) | Lurie Children's”. https://www.luriechildrens.org/en/blog/living-with-pots/
- “POTS tips from Pediatric Partners | Children's Mercy Pediatric Partners Inc | Overland Park, KS | Olathe, KS”. https://pediatricpartnerskc.com/POTS-tips-from-Pediatric-Partners
- “Understanding POTS Symptoms: Signs, Causes, and Management Strategies”. https://avicennacardiology.com/blog/pots-symptoms/
- “Navigating Flare-ups — Awareness for POTSies”. https://www.awarenessforpotsies.org/managing-flare-ups
- “A Guide to POTS and How to Manage the Symptoms”. https://brand.education/a-guide-to-pots-and-how-to-manage-the-symptoms/
- “How to Prevent Flare-Ups in POTS/Dysautonomia”. https://www.accessibledaytrips.com/post/how-to-prevent-flare-ups-in-pots-dysautonomia
- “What are some of the most common POTS triggers? | Empirical Health”. https://www.empirical.health/blog/common-pots-triggers
- “Understanding POTS: Symptoms, Diagnosis, and Effective Management Strategies — Dazzle Health”. https://dazzlehealth.me/dazzle-blog/understanding-pots-symptoms-management-strategies
- “Key POTS Symptoms You Should Know”. https://aclsnow.com/blog/symptoms-signs-of-pots-syndrome/
- “Lifestyle Modifications | Standing Up To POTS”. https://www.standinguptopots.org/POTSlifestylemodifications
- “Nursing made Incredibly Easy”. https://journals.lww.com/nursingmadeincrediblyeasy/Fulltext/2020/07000/Dysautonomia__Getting_a_handle_on_POTS.4.aspx
- “Exercise and Non-Pharmacological Treatment of POTS – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC6289756/
- “Lifestyle Adaptations for Postural Orthostatic Tachycardia Syndrome (POTS) | The EDS Clinic”. https://www.eds.clinic/articles/lifestyle-adaptations-for-pots
- “POTS DIET AND NUTRITION: WHAT WORKS BEST FOR SYMPTOM MANAGEMENT — Athleisure Mag™ | Athleisure Culture”. https://www.athleisuremag.com/the-latest/2025/2/11/pots-diet-and-nutrition-what-works-best-for-symptom-management
- “Top 3 Lifestyle Changes to Treat POTS — Kristin McConnell, OTD, OTR/L”. https://www.kristinmcconnell.com/blog/top-3-lifestyle-changes-to-treat-pots
- “POTS: Causes, Symptoms, Diagnosis & Treatment”. https://my.clevelandclinic.org/health/diseases/16560-postural-orthostatic-tachycardia-syndrome-pots%26lt
- “Evaluating and managing postural tachycardia syndrome | Cleveland Clinic Journal of Medicine”. https://www.ccjm.org/content/86/5/333
- “Postural orthostatic tachycardia syndrome in primary care: diagnosis, treatment and a case of African-American man presenting with POTS – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC6754633/
- “Medication – PoTS UK”. https://www.potsuk.org/managingpots/medication-2/
- “Tilt-Table Test – Professional Heart Daily | American Heart Association”. https://professional.heart.org/en/health-topics/heart-attack/diagnosing-a-heart-attack/tilt-table-test
- “Tilt Table Testing | Johns Hopkins Medicine”. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/tilt-table-testing
- “Tilt Table – StatPearls – NCBI Bookshelf”. https://www.ncbi.nlm.nih.gov/books/NBK482320/
- “PoTS: How can a dietitian help to support those with Postural Tachycardia Syndrome? – BDA”. https://www.bda.uk.com/resource/how-can-a-dietitian-help-to-support-those-with-postural-tachycardia-syndrome.html
- “Lifestyle Measures | Vanderbilt Autonomic Dysfunction Center”. https://www.vumc.org/autonomic-dysfunction-center/lifestyle-measures
- “COVID-19 Increases the Prevalence of Postural Orthostatic Tachycardia Syndrome: What Nutrition and Dietetics Practitioners Need to Know – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC9186518/
- “Autoimmunity and postural orthostatic tachycardia syndrome: Implications in diagnosis and management | Cleveland Clinic Journal of Medicine”. https://www.ccjm.org/content/90/7/439
- “What are the Mechanisms of POTS & other forms of Dysautonomia? – POTS – Dysautonomia Information Network (DINET)”. https://www.dinet.org/info/pots/what-are-the-mechanisms-of-pots-other-forms-of-dysautonomia-r97/
- “Living with POTS: Common Symptoms, Flare-Ups, and Effective Treatments for Women — Dr. McKenzy Brewer, DC”. https://www.drmckenzybrewer.com/blog/pots-explained-common-symptoms-flare-ups-and-treatment-for-women
- “Causes and Classification – PoTS UK”. https://www.potsuk.org/about-pots/classification/
- “Reversible postural orthostatic tachycardia syndrome – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC4517341/
- “KoreaMed Synapse”. https://synapse.koreamed.org/articles/1145419
- “Misdiagnosed Seizure-Like Activity in a Patient With Postural Orthostatic Tachycardia Syndrome: A Case Report – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC10292221/
- “Postural Tachycardia Syndrome: A Heterogeneous and Multifactorial Disorder – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC3547546/
- “Postural Orthostatic Tachycardia Syndrome – StatPearls – NCBI Bookshelf”. https://www.ncbi.nlm.nih.gov/books/NBK541074/
- “Postural orthostatic tachycardia syndrome is an under-recognized condition in chronic fatigue syndrome – PubMed”. https://pubmed.ncbi.nlm.nih.gov/18805903/
- “Neurohumoral and haemodynamic profile in postural tachycardia and chronic fatigue syndromes – PubMed”. https://pubmed.ncbi.nlm.nih.gov/21906029/
- “Long-COVID-19 Patients Are Getting Diagnosed With Little-Known Illnesses Like POTS”. https://time.com/6051767/long-covid-19-rare-disease-pots/
- “5 Top tips for managing postural orthostatic tachycardia syndrome (POTS) symptoms – Medicine.com”. https://www.medicine.com/health/5-top-tips-managing-pots-symptoms