If you’re dealing with chronic pain, logging your symptoms daily could change everything. Most people rely on memory or vague descriptions when talking to their doctor. But pain is complex. It shifts in intensity, location, and triggers. A pain log removes the guesswork by helping you document exactly how you feel, when symptoms appear, and what might be causing them.
A pain log, also called a pain diary, is a structured way to track your pain over time. You can record details like time of onset, pain severity, affected area, potential triggers, and relief strategies. This information becomes crucial for identifying patterns, evaluating whether treatments are working, and making faster, more informed medical decisions.
Whether you are managing migraines, joint pain, endometriosis, or fibromyalgia, using a pain log app like CareClinic makes it easy to track your symptoms daily. The app turns your notes into visual pain charts and progress reports that can be shared with your doctor. Instead of repeating symptoms from memory, you bring real data. That is what leads to better outcomes.
In this guide, you will learn how to use a pain log effectively, what to track, and how to get the most out of your entries, even if you have never tracked anything before.
Why You Should Monitor Your Pain with a Daily Log
Monitoring your pain daily gives you control. When pain becomes chronic, it is no longer just a symptom. It affects your energy, your decisions, your relationships, and your mental health. Logging your pain each day builds a clear, objective record of what you are going through, instead of relying on vague memory when speaking to your doctor.
A pain log helps you identify patterns that are easy to miss. For example, you might discover that pain spikes around certain meals, during specific times of day, or after poor sleep. You can also log emotional triggers like stress or anxiety, which often increase pain intensity. These details matter. They give your care team insights that lab tests cannot.
- A daily pain log can include:
- Pain location (back, joints, head, abdomen)
- Pain type (burning, stabbing, throbbing)
- Pain level using a 1 to 10 scale
- Onset and duration (when it started and how long it lasted)
- Associated symptoms (nausea, fatigue, swelling)
- Triggers and relief methods (food, medication, weather, posture)
Using a pain tracking app like CareClinic makes this easier. You can build a custom care plan, set reminders, and link your pain entries to the medication tracker, symptoms, and daily habits. Over time, the app generates reports and charts you can share with your doctor or specialist. These pain reports support diagnosis, help justify treatment changes, and document progress for insurance.
If you already use a pain diary, upgrading to a structured pain log app gives you more accuracy and fewer missed entries. CareClinic offers printable logs, calendar tracking, and a private space to record your health journey, including other conditions like arthritis, endometriosis, or migraines.
In short, monitoring your pain with a daily log gives you clarity, improves communication with your care team, and helps you take control using data. The more consistent your entries are, the faster you will learn what works and what does not.
How to Start Your Daily Pain Log
Logging pain is only useful if it is done right. Most people start tracking pain but stop because it feels confusing, inconsistent, or too much work. If your log is messy or vague, your doctor cannot use it. But when done properly, a daily pain log becomes a powerful tool for making decisions about your care.
Start with a system you can stick to. Use a pain log app like CareClinic that lets you record your symptoms quickly, organize entries by condition, and export reports without having to build spreadsheets or templates manually.
Here is how to do it properly:
1. Create a personalized care plan: Inside the app, start by setting your condition, goals, and what you want to improve. This creates structure and keeps the log focused.
2. Add your medications and treatments: Input any pills, supplements, or therapies you are using for pain. You will later connect your pain entries to these treatments to see what works.
3. Log each pain episode in real time: As soon as pain begins, open the app and log what you feel. Select pain type, intensity, duration, and body location. Use a scale from 1 to 10. If you delay logging, the details will fade.
4. Note what may have triggered it: Track what happened before the pain started. This could be food, movement, weather, stress, sleep issues, or missed medication. These triggers are often what doctors are looking for.
5. Record what you did for relief: Did you take a painkiller, stretch, rest, use heat, or do nothing at all? This helps identify which methods actually reduce your pain and which are not effective.
6. Review your progress weekly: CareClinic will generate graphs, pain timelines, and printable logs that you can review or bring to appointments. These reports show trends that are impossible to see without data.
A strong pain tracking routine only takes a few minutes a day, but it can give you years of your life back. No more guessing. No more repeating the same story at every visit. Just data that speaks for itself.
How to Share Your Pain Log With Your Doctor and Get Results
A pain log is only as valuable as the action it leads to. Logging pain daily is great, but if your doctor cannot use that data, it is just another habit with no ROI. The goal is to turn your notes into results.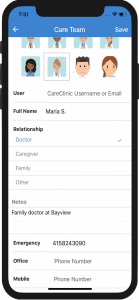
With the CareClinic app, you can export a complete pain report that includes pain frequency, intensity patterns, medication use, and related symptoms. This gives your physician or specialist the full context without needing to ask follow-up questions or guess what you meant.
Here is how to make your pain log useful in every appointment:
- Print or export your pain report before the visit. CareClinic allows you to generate a PDF pain log that includes all relevant data. Print it or send it to your provider securely. This saves time and shows that you are serious about your health.
- Highlight trends or concerns. Use the report to point out what is working and what is not. For example, “Pain worsens after 3 PM every day,” or “No change after switching meds last month.”
- Use the log to validate symptoms. Doctors need objective data to justify treatments, escalate care, or approve referrals. Your log builds that paper trail.
- Share relevant sections with your family or care team. You can give others access to view symptoms, missed doses, or changes in condition. This helps with accountability, support, and coordination.
Many patients struggle to explain their pain clearly. They forget dates, misjudge severity, or downplay what is happening. With a log, there is no confusion. You bring the facts. And when you bring data, you get better decisions, faster treatment, and less trial and error.
What Types of Pain Should You Track in a Daily Pain Log?
Pain is not just pain. There are different types, intensities, and causes, and each requires a different approach to treatment. One of the most common mistakes people make when using a pain diary is not being specific enough. General entries like “bad pain today” are too vague to help your doctor. To get real answers and the right treatment, your pain log needs to include details across five key areas.
1. Location-Based Pain
Recording exactly where the pain occurs helps your care provider narrow down possible causes and decide whether imaging, blood work, or referrals are needed.
Use plain language like:
- Lower back pain
- Behind the eyes
- Lower right abdomen
- Left shoulder blade
- Pelvic pain
- Ear pain from migraine
Avoid simply writing “back pain” if you can be more specific. The CareClinic app includes a body map that allows you to tap and log the precise area. This becomes even more valuable over time when multiple areas are affected. If pain shifts location over days or weeks, that detail may help rule out or confirm certain diagnoses.
2. Type or Quality of Pain
Pain has a texture, and how it feels tells your provider something about what may be going on underneath. Use words that describe the actual sensation:
- Burning or tingling pain may suggest nerve involvement.
- Throbbing or pulsing could relate to blood flow or inflammation.
- Sharp or stabbing pain is often mechanical, triggered by movement or pressure.
- Dull or achy pain is usually muscular or joint-related.
Try to choose one or two descriptors that best match what you are feeling. If it changes throughout the day, note that. For example, it may start dull in the morning and become sharp in the evening. These shifts can reveal how your body is responding to stress, posture, or medication.
3. Intensity and Duration
Use a consistent 1 to 10 pain scale. For example:
- 1 = barely noticeable
- 5 = distracting but manageable
- 10 = cannot function or needs emergency care
Record how long each pain episode lasts. Does it fade in minutes or linger for hours? Also, track how often it returns. Is it constant or episodic?
Many people discover their pain has a time pattern, like increasing in the afternoon or during specific physical activities. These observations are powerful. Doctors can use this data to fine-tune medications or explore deeper causes like hormonal fluctuations, sleep cycles, or inflammatory response.
4. Triggers and Contributing Factors
Sometimes, pain is not random. It may be linked to what you ate, how you slept, your stress level, or even the weather. Logging potential triggers helps reveal patterns over time.
Consider tracking:
- Foods or drinks consumed before the pain
- Emotional stress or panic episodes
- Sleep quality the night before
- Exercise, overuse, or physical exertion
- Menstrual cycle phase or hormonal changes
This information becomes more useful the longer you track. For example, someone might realize that neck pain flares up after poor sleep and high-stress meetings. Another person may find migraines are tied to skipped meals or specific foods. These are insights you cannot get from memory alone.
5. Response to Treatment or Interventions
Always log what you did to manage the pain. Whether it worked or not, this tells your provider what should stay in your plan and what should be changed.
Log details like:
- Medications taken (name and dose)
- Physical therapy exercises
- Rest, stretching, or hot/cold therapy
- Position changes or mobility adjustments
- The time it took for the pain to reduce
Do not just say “felt better.” Note how long it took to get relief and how long the relief lasted. If the same treatment provides inconsistent results, that matters too. For example, if a medication helps for 2 hours one day but has no effect the next, it might point to tolerance or a separate issue.
Why This Matters
Doctors make decisions based on evidence. Your log becomes that evidence. The more precise and consistent your entries, the easier it is for your care team to find patterns, avoid trial and error, and prescribe the right interventions. Over time, this process can reduce pain severity, improve daily function, and give you back a sense of control.
What Else Should You Remember When Tracking Pain?
Consistency matters more than perfection. A pain log is only useful if you build the habit of tracking regularly. You do not need to write a novel each time. Simple, accurate entries made at the right time are what give you useful patterns.
This is especially true for people managing conditions like fibromyalgia, arthritis, endometriosis, or chronic back pain. These are not conditions that follow a simple script. The pain can change daily or even hourly. A clear, detailed record makes it easier for your care team to adjust treatment quickly. If you are also looking for reviews of the best pain app to use, see this CareClinic vs Painscale review that we did.
Track Pain in Real Time
Track your symptoms as close to real time as possible. When pain strikes, log the details right away or use voice-to-text if typing is difficult. The longer you wait, the more you forget. Even small details like what you ate, your mood, or the time of day can become meaningful if tracked consistently.
Use Clear, Consistent Data
Use a standard pain scale. Pick one method and stick with it. Whether it is a 1 to 10 scale or a color-coded visual scale, your doctor will be able to interpret results faster if you use the same format across all entries.
Describe your pain clearly. Avoid vague terms like “bad pain” or “the usual.” Instead, use specific language: burning, dull, stabbing, or sharp. Write where the pain is, how it started, and how long it lasted. For people with migraines, this level of detail can help spot triggers like light, noise, or stress.
Include what you did to manage the pain. Note any medications, rest periods, movement, or therapies. Did it help? How long did it take? Even if a treatment failed, that is still valuable information for your care provider.
Track your pain in context. Pain does not exist in isolation. It is often influenced by sleep, food, hormones, stress, hydration, and physical activity. People with autoimmune conditions often report that stress and poor sleep worsen pain. The more of these variables you track, the better your chances of uncovering patterns.
Build a Habit That Works
Use a digital pain log or app to stay organized. Apps like CareClinic can remind you to log, store everything in one place and generate printable reports. You will never lose your records, and you can always bring the latest updates to appointments.
Logging your pain should not feel like a chore. Done right, it becomes a daily check-in that helps you spot what is working and what is not. Over time, your pain log becomes more than just notes. It becomes evidence, a guide, and a tool to help you take back control.


