
Pain from underlying conditions can flare up for a variety of reasons. Sometimes, an increase in pain may be due to a change in your condition. Other times, it may be the result of overdoing it or not getting enough rest. With proper pain management techniques and a plan in place, you can help to prevent or lessen the intensity of these flares. There are a few things you can do to help manage your pain and keep it under control. Continue reading below as we describe some tips to help you during a pain flare-up.[1]
Table of Contents
- Types of Pain
- What is chronic pain?
- What causes chronic pain flares?
- How can CareClinic help with my pain treatment?
- What is a chronic pain flare?
- What does a pain flare up feel like?
- What are the most common medications to manage pain?
- What can I do to prevent or reduce chronic pain flares?
- How long do pain flare up’s last?
- What can I do to relieve pain during a flare up?
- How does sitting affect pain flare-ups?
- Can weather changes affect pain flare-ups?
- Which foods cause pain flare ups?
- How do you measure the intensity of your pain?
- Other ways chronic pain reduces your quality of life
- Ways of managing your stress levels
- Awareness develops with experience
Types of Pain
There are different types of pain, but most can be classified as either nociceptive or neuropathic. Nociceptive pain is caused by damage to tissues and is the most common type of pain. It can be acute (short-term) or chronic (long-term). Neuropathic pain is caused by damage to the nervous system and is less common. It can be either acute or chronic. Most pain is the result of nociceptive pain, which occurs when tissues are damaged. This type of pain can be acute (short-term) or chronic (long-term).[2]
What is chronic pain?
Chronic pain is defined as pain that lasts for more than three months. It can be the result of an injury, such as a sprained ankle, or it can be the result of a chronic condition, such as inflammatory arthritis, back pain, cancer, fibromyalgia, headaches, multiple sclerosis, neuropathy, and more. Chronic pain can be debilitating and hurt your quality of life. It is important to seek medical help if you are experiencing chronic pain, as it may be the result of an underlying condition. Chronic pain will not go away on its own and will often require treatment. Patients often require a combination of medication, physical therapy, and psychological support to manage their chronic pain.
h2,h3 { display: inline-block; }
Which arthritis condition causes pain and why?
There are many types of arthritis, but the two most common are osteoarthritis and rheumatoid arthritis. Osteoarthritis is caused by the breakdown of cartilage, which is the cushioning between bones in your joints. This can lead to pain, stiffness, and swelling in the affected joints. Rheumatoid arthritis is an inflammatory condition that causes pain, stiffness and swelling in the joints. It can also lead to joint damage.
Back Pain
Back pain flares can also be caused by a muscle strain, herniated disc, degenerative disc disease, spinal stenosis or other conditions. This type of pain is usually nociceptive pain and can be acute or chronic.
What causes chronic pain flares?
There are many possible triggers for chronic pain flares, including injury or trauma, changes in weather, fatigue, infection, and stress. Some common reasons for these triggers include:
– Stress as it can worsen pain.
– Lack of sleep as fatigue can make pain worse.
– Poor diet as certain foods can contribute to inflammation.
– Weather changes as barometric pressure changes can affect pain levels.
– Infection as it can cause inflammation.
– Hormonal changes as they can affect pain perception.
The most common reason reported by patients is “overdoing it.” This includes physical activity such as yard work, housework, or even exercise. Overexertion can cause muscles to become fatigued and lead to pain. It is important to listen to your body and take breaks when needed.
Identify your triggers, and keep a journal of when your pain flares up and what you were doing beforehand. This can help you to identify possible triggers and avoid them in the future. If you have chronic pain, it is important to be aware of your triggers and to manage them as best as you can.[4][5]
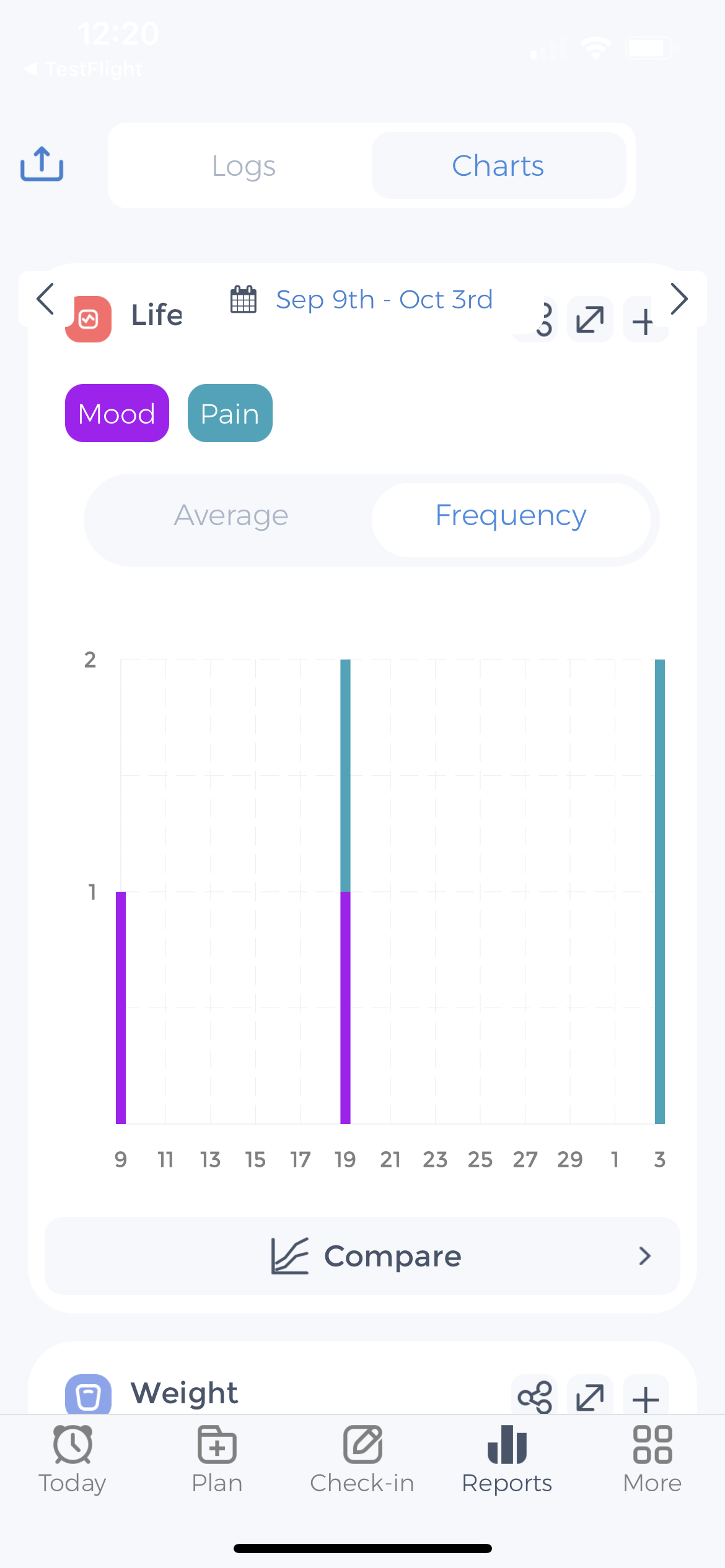
How can CareClinic help with my pain treatment?
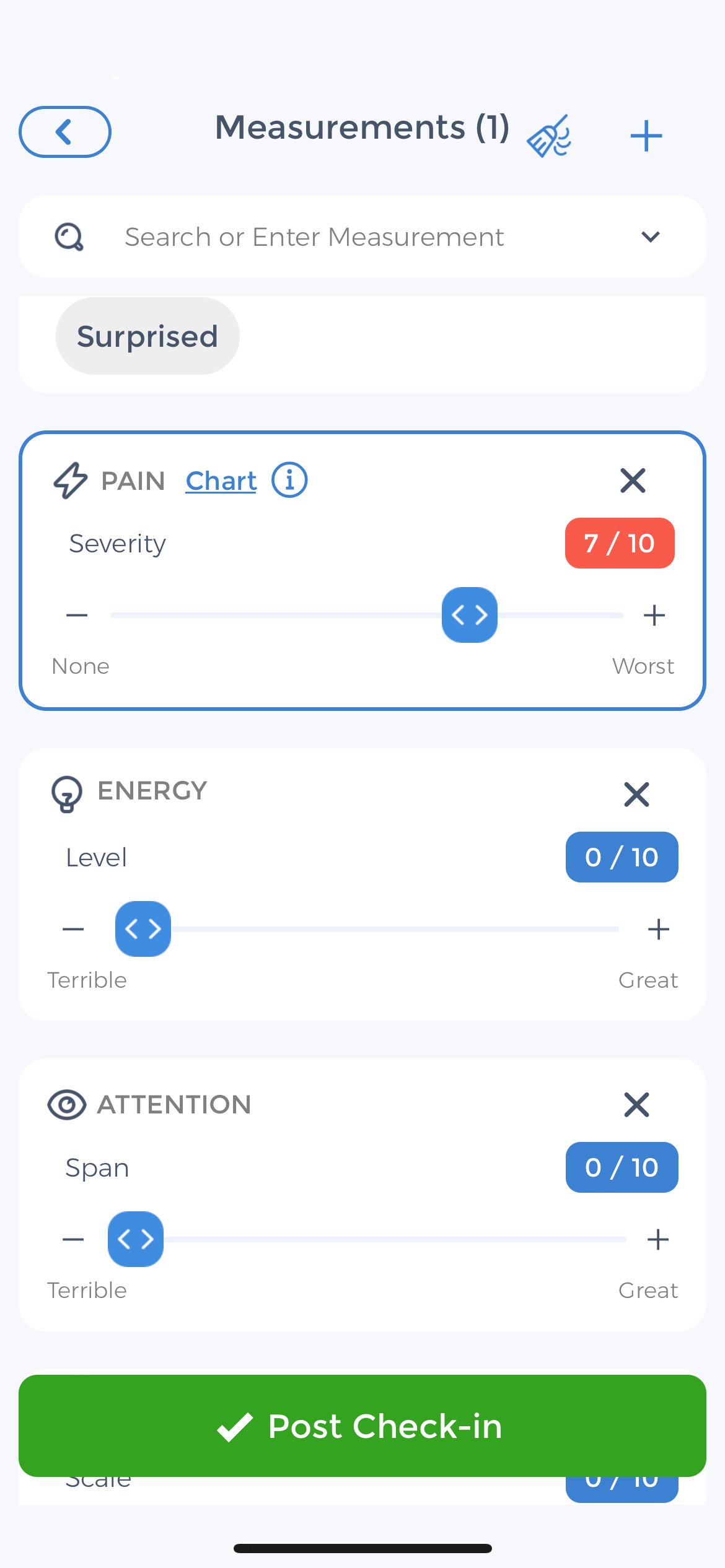
- Tracking your pain levels
- Keeping track of your medications
- Identifying your triggers by discovering patterns
- Setting goals
- Sharing your progress with your doctor
Using CareClinic to record your symptoms, and pain triggers can help you to better manage your chronic pain because you will have a better understanding of what works for you and what doesn’t. Additionally, sharing your progress with your doctor can help them to provide you with the best possible care.
Here’s a review by a patient with Sciatica
I have suffered from Sciatica for years and it has gotten progressively worse. I was at the point where I could barely walk, and the pain was so bad that I was taking Vicodin every day just to function. My wife suggested that I start using CareClinic to track my pain levels, medication, and triggers. This has been a game-changer for me! I am now able to see patterns in my pain, and I have been able to identify my triggers. I have also been able to work with my doctor to find a medication that works better for me. I am now pain-free most days, and I am off of Vicodin. I am so grateful to CareClinic for helping me to get my life back!
If you suffer from chronic pain, download CareClinic today and start tracking your symptoms to take control of your pain.
What is a chronic pain flare?
A chronic pain flare is a sudden, intense increase in pain that can last for days or weeks. flares can be unpredictable and often occur without warning. Many people with chronic pain experience flares regularly. If you experience pain flaring up, it’s important to take quick action to help reduce the pain. Pain can include cramps, throbbing, or sharp shooting sensations.[6][7]
What does a pain flare up feel like?
You’ll know when you’re experiencing a pain flare-up because the pain will be sudden and intense. It can feel like a sharp, stabbing pain, jabbing or throbbing aching pain. The pain may be constant or it may come and go.
You may also experience other symptoms, such as fatigue, headaches, muscle aches, stiffness and tension. The symptoms can be managed, but the pain can be debilitating.[8]
What are the most common medications to manage pain?
Non-steroidal anti-inflammatory drugs (NSAIDs): NSAIDs are a type of medication that can be used to reduce inflammation and pain. Examples of NSAIDs include ibuprofen, naproxen, and aspirin.
Opioids: Opioids are a type of medication that can be used to relieve severe pain. Opioids work by binding to pain receptors in the brain, which blocks the perception of pain. Examples of opioids include morphine, codeine, and oxycodone.
Antidepressants: Antidepressants are a type of medication that can be used to treat both pain and depression. Antidepressants work by affecting the levels of certain chemicals in the brain, which can help to reduce pain. Examples of antidepressants include amitriptyline and duloxetine.
Anticonvulsants: Anticonvulsants are a type of medication that can be used to treat seizures and pain. Anticonvulsants work by reducing the activity of certain chemicals in the brain, which can help to reduce pain. Examples of anticonvulsants include gabapentin and pregabalin.
Corticosteroids: Corticosteroids are a type of medication that can be used to reduce inflammation and pain. Corticosteroids work by reducing the activity of the immune system, which can help to reduce inflammation. Examples of corticosteroids include prednisone and dexamethasone.
Your doctor will work with you to determine which type of medication is best for you based on your individual needs.
What can I do to prevent or reduce chronic pain flares?
There is no guaranteed way to prevent chronic pain flares, but there are some things you can do to help reduce your risk:
- Stay on top of your pain management. This means taking your medications as prescribed and keeping up with any other treatment plans, such as physical therapy.
- Avoid triggers. If you know certain activities or situations trigger your pain, try to avoid them.
- Get enough rest. Fatigue can make pain worse, so make sure you’re getting enough sleep.
- Eat a healthy diet. Eating nutritious foods can help reduce inflammation, which can lead to pain.
- Exercise regularly. Exercise can help improve your overall health and increase your pain tolerance.
- Reduce stress. Stress can make pain worse, so finding ways to relax and de-stress is important.
How long do pain flare up’s last?
Some people may only experience a pain flare up for a few hours, while others may have pain that lasts for days or weeks. The average length of a pain episode is about three days. This means that even if you’re only dealing with pain flares a few times a year, they can still have a big impact on your life.
What can I do during a chronic pain flare?
If you’re experiencing a pain flare up, there are some things you can do to help ease the pain:
– Take your pain medication as prescribed.
– Apply heat or cold packs to the painful area.
– Try relaxation techniques, such as deep breathing or progressive muscle relaxation.
– Get some exercise. While it may be the last thing you feel like doing, gentle exercise can help to reduce pain.
– Avoid trigger activities or situations.
– Take a hot bath or shower.
– Sleep. Getting enough rest is important when you’re in pain.
Having a flare management plan can greatly help you manage flares. Use the CareClinic app to track your pain levels, medications, and other symptoms so you can quickly identify when a flare is starting and take action to prevent it from getting worse. During a flare, focus on taking a deep breath and taking care of yourself. Pain flares are not your fault and you are not alone. Many people live with chronic pain, so reach out to a support group or caregiver.
What can I do to relieve pain during a flare up?
There are several things you can do to help relieve pain during a flare up:
- Take your pain medication as prescribed.
- Apply heat or cold to the painful area.
- Try relaxation techniques, such as deep breathing or progressive muscle relaxation.
- Get some exercise. While it may be difficult to exercise when you’re in pain, moderate activity can help to reduce pain.
How does sitting affect pain flare-ups?
When you sit, you’re putting pressure on your spine and the discs in your back. This can lead to pain flare-ups, especially if you have a condition like degenerative disc disease. Sitting also puts pressure on your joints and muscles, which can lead to pain in those areas. If you have a condition like arthritis, sitting can make your pain worse.
Can weather changes affect pain flare-ups?
For some people, weather changes can trigger pain flare-ups. This is most commonly seen in people with conditions like arthritis or fibromyalgia. Cold weather can make pain worse, while warm weather can help to reduce pain.
Which foods cause pain flare ups?
However, some people with chronic pain find that certain foods can trigger or worsen their symptoms. Common triggers include:
- Sugary foods
- Processed foods
- Foods high in fat
- Foods that contain MSG
- Aspartame
The reasoning behind this is that these foods can cause inflammation in the body, which can lead to pain. If you think certain foods may be triggering your pain, it’s important to talk to your doctor so they can help you determine if there’s a connection.
How do you measure the intensity of your pain?
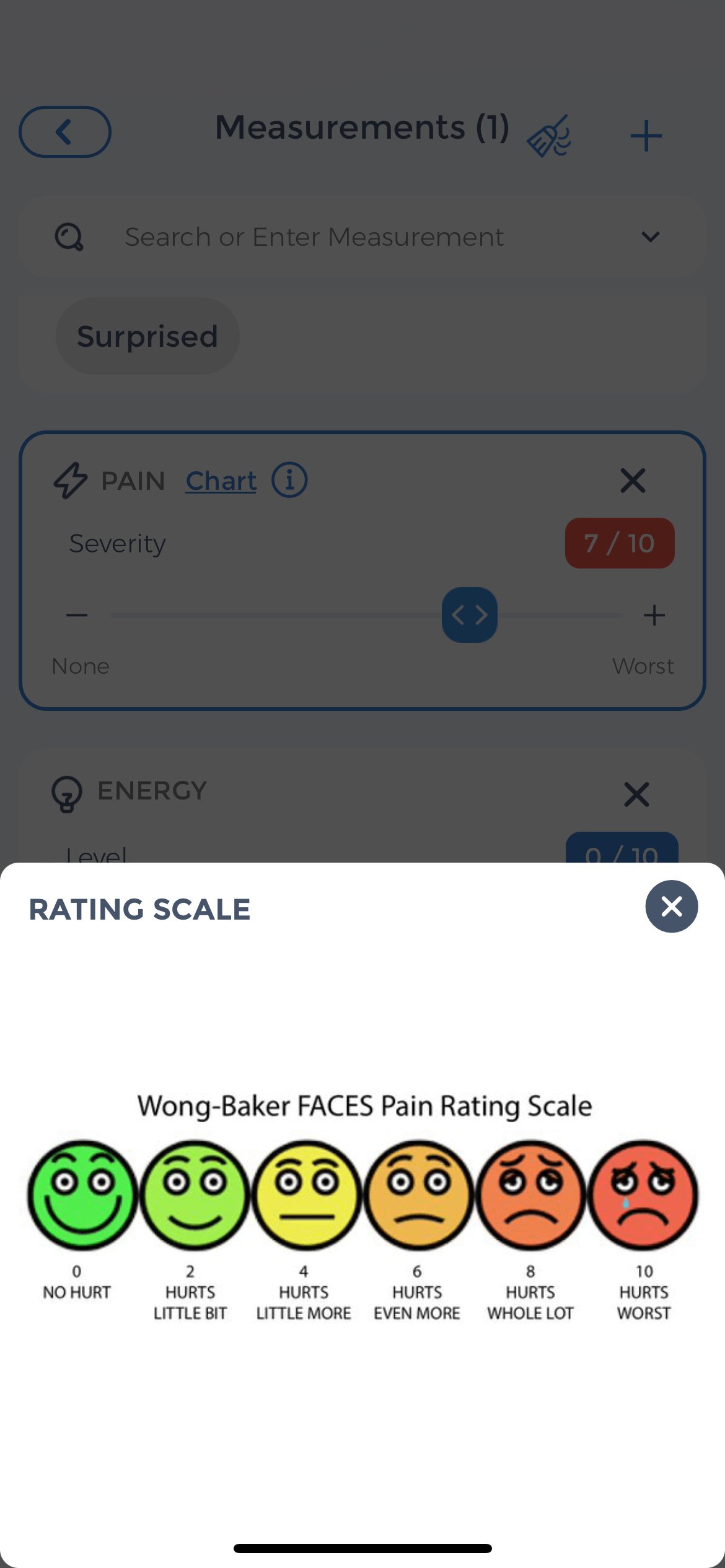
If you’re experiencing a pain flare up, it’s important to keep track of your pain level so you can communicate this to your healthcare team. The CareClinic app can help you track your pain level and other symptoms so you can more easily identify when a flare is starting and take action to prevent it from getting worse.
Other ways chronic pain reduces your quality of life
Chronic pain can also lead to other problems that reduce the quality of your life. For example, chronic pain can often make it difficult to sleep. This can lead to fatigue, which can make it difficult to function during the day. Chronic pain can also cause anxiety and depression. These conditions can make it even harder to manage chronic pain. Normal, everyday activities can become difficult or impossible to do when you’re in pain. This can lead to social isolation and a reduced ability to participate in activities you enjoy.
Chronic pain can have a profound impact on your quality of life. It’s important to talk to your doctor about ways to manage your pain so you can live a fuller, richer life.
Ways of managing your stress levels
Chronic stress can make the pain worse and can even trigger pain flare-ups. Luckily, many things can be done to help you manage stress levels in your life. We have written extensively about journaling for stress relief and ways of coping with anxiety, but here are a few other ideas that you may not be doing:
Get a massage: Research has shown that massage can help to reduce stress and pain.
Spend time with friends or family: Spending time with loved ones can help to reduce stress and make pain more bearable.
Listen to music: Music has been shown to have a calming effect on the mind and body, which can help to reduce stress and pain.
Art therapy: Art therapy involves using creative expression to explore and process emotions. It can be a helpful way to deal with stress and pain.
Awareness develops with experience
To summarize, set realistic goals when trying to cope with pain. Choose activities that won’t aggravate your symptoms, such as those that maintain a neutral or healthy posture. Exercising, practicing stress-relieving techniques and journaling can also help you manage your pain levels. Lastly, find a support system to help you through tough times. Friends, family, or a therapist can provide an outlet to express your thoughts and feelings associated with chronic pain flare-ups.
References
- “Coping with a flare up of chronic pain | NHS inform”. https://www.nhsinform.scot/illnesses-and-conditions/brain-nervs-and-spinal-cord/chronic-pain/coping-with-a-flare-up-of-chronic-pain
- “Types of Pain | Pain Management Education at UCSF”. https://pain.ucsf.edu/patients/types-pain
- “Chronic Pain: What It Is, Symptoms, Treatment & Management”. https://my.clevelandclinic.org/health/diseases/4798-chronic-pain
- “Stress, Inflammation and Chronic Pain — Institute for Chronic Pain”. https://www.instituteforchronicpain.org/blog/item/152-55stress-inflammation-and-chronic-pain
- “Can Weather Changes Make Chronic Pain Worse? Understanding the Link – AllCare Health & Pain”. https://www.njallcarepain.com/blog/can-weather-changes-make-chronic-pain-worse-understanding-the-link/
- “What Are Pain Flare-Ups? – The Pain Experts of Arizona”. https://www.thepainexpertsofarizona.com/blog/what-are-pain-flare-ups/
- “Flare-up and setback management | CUH”. https://www.cuh.nhs.uk/patient-information/flare-up-and-setback-management/
- “Fibromyalgia Symptoms | Stanford Health Care”. https://stanfordhealthcare.org/medical-conditions/bones-joints-and-muscles/fibromyalgia/symptoms.html
- “How your diet can combat chronic inflammation | Ohio State Health & Discovery”. https://health.osu.edu/wellness/exercise-and-nutrition/diet-can-combat-chronic-inflammation
- “Prevalence and Characteristics of Flare-ups of Chronic Non-specific Back Pain in Primary Care: A Telephone Survey – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC3414658/


