Scleroderma is a chronic autoimmune condition that affects the connective tissues in the body. It is characterized by the hardening and tightening of the skin, as well as the potential involvement of internal organs such as the lungs, heart, and kidneys. If you or a loved one is living with scleroderma, it is essential to understand the condition and learn how to manage it effectively.
Understanding Scleroderma
Scleroderma, also known as systemic sclerosis, is a rare autoimmune disease that results in the overproduction of collagen, a protein that forms the basis of connective tissues in the body. This excess collagen buildup leads to thickening and hardening of the skin and other connective tissues, causing symptoms such as tightness, pain, and limitations in movement.
Scleroderma is a complex condition that can have a significant impact on a person’s quality of life. Understanding the different types of scleroderma, its causes, and risk factors is crucial in managing the disease effectively.
Types of Scleroderma
Scleroderma can manifest in different ways, and there are two main types: localized scleroderma and systemic scleroderma. Localized scleroderma primarily affects the skin and underlying tissues, while systemic scleroderma can involve not only the skin but also internal organs.
Localized scleroderma typically presents as patches of thickened and hardened skin, which may appear shiny and have a waxy texture. This type of scleroderma usually does not affect internal organs and tends to have a milder course compared to systemic scleroderma.
Systemic scleroderma, on the other hand, can be further classified into two subtypes: limited cutaneous systemic sclerosis and diffuse cutaneous systemic sclerosis. Limited cutaneous systemic sclerosis primarily affects the skin on the face, hands, and feet, while diffuse cutaneous systemic sclerosis involves widespread skin involvement, often affecting the arms, legs, and trunk.
In addition to skin changes, systemic scleroderma can cause complications in various organs, including the lungs, heart, kidneys, and gastrointestinal tract. These complications can lead to a range of symptoms and require specialized management.
Causes and Risk Factors of Scleroderma
The exact cause of scleroderma is still unknown. However, both genetic and environmental factors are believed to play a role in its development. It is thought that certain individuals may have a genetic predisposition to the disease, making them more susceptible to developing scleroderma when exposed to certain triggers.
Environmental factors, such as exposure to certain chemicals and toxins, have been implicated in the development of scleroderma. For example, certain occupational exposures, such as silica dust and organic solvents, have been associated with an increased risk of developing the disease.
In addition, certain viral infections, such as Epstein-Barr virus and cytomegalovirus, have been suggested as potential triggers for scleroderma. These viruses may activate the immune system and contribute to the abnormal collagen production seen in the disease.
Furthermore, a family history of autoimmune diseases, such as rheumatoid arthritis or lupus, can increase the likelihood of developing scleroderma. This suggests a genetic component to the disease, although the specific genes involved have not yet been fully identified.
It is important to note that while these risk factors may increase the likelihood of developing scleroderma, not everyone exposed to them will develop the disease. The interplay between genetic susceptibility and environmental triggers is complex and not fully understood.
Overall, understanding the various types of scleroderma, as well as its causes and risk factors, is crucial in advancing our knowledge of this complex disease. Ongoing research aims to unravel the underlying mechanisms and develop more effective treatments for individuals living with scleroderma.
Diagnosing Scleroderma
Symptoms of Scleroderma
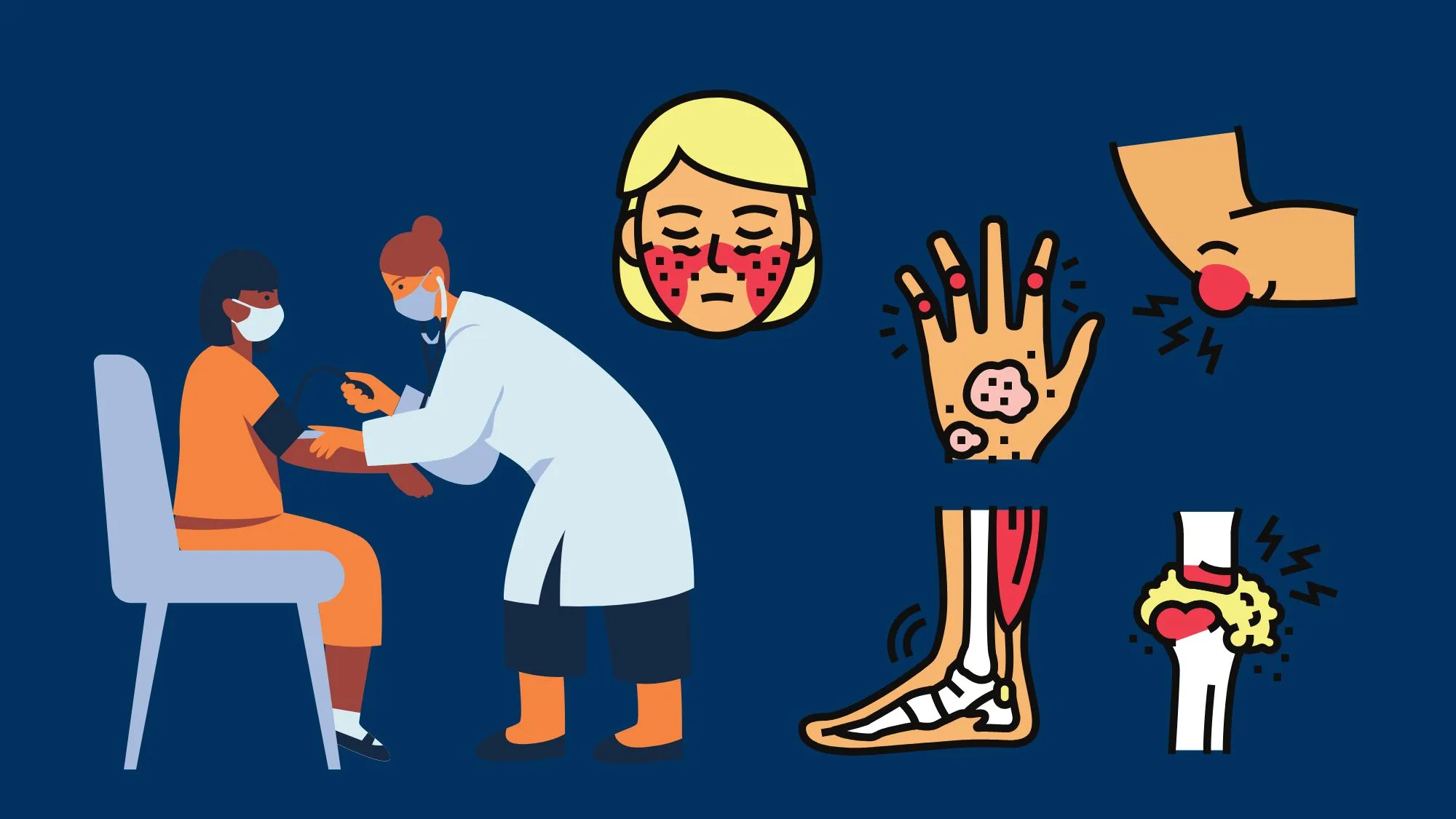
Scleroderma presents with a wide range of symptoms that may vary from person to person. Common symptoms include thickening and hardening of the skin, joint pain and stiffness, fatigue, muscle weakness, digestive issues, and Raynaud’s phenomenon, characterized by color changes in the fingers and toes in response to cold or stress.
Thickening and hardening of the skin, known as fibrosis, is a hallmark symptom of scleroderma. This can affect various parts of the body, such as the face, hands, arms, and legs. The skin may become tight, shiny, and difficult to move, leading to limited mobility and potential disfigurement.
Joint pain and stiffness are common complaints among individuals with scleroderma. This can make everyday tasks challenging and affect the quality of life. The joints may become swollen, tender, and difficult to bend or straighten, causing discomfort and limitations in movement.
Fatigue and muscle weakness are frequently reported symptoms in scleroderma patients. The underlying mechanisms behind these symptoms are not yet fully understood, but they can significantly impact daily activities and overall well-being. Fatigue may be accompanied by feelings of exhaustion, lack of energy, and difficulty in concentrating.
Individuals with scleroderma often experience digestive issues, such as acid reflux, difficulty swallowing, and bloating. These symptoms can be caused by the hardening and tightening of the esophagus and gastrointestinal tract, leading to complications in the digestion and absorption of food.
Raynaud’s phenomenon is another common symptom of scleroderma. It is characterized by color changes in the fingers and toes in response to cold temperatures or emotional stress. The affected areas may turn white, blue, or purple, and become numb or tingly. Once the blood flow returns, the skin may turn red and throb with pain.
Medical Tests and Procedures
To diagnose scleroderma, your healthcare provider will perform a thorough physical examination, review your medical history, and order specific tests. These may include blood tests to check for certain antibodies associated with scleroderma, imaging studies like X-rays or CT scans to assess organ involvement, and skin biopsies to analyze skin tissue under a microscope.
Blood tests are commonly used to detect specific antibodies that are often present in individuals with scleroderma. These antibodies include anti-nuclear antibodies (ANA), anti-centromere antibodies (ACA), and anti-Scl-70 antibodies. The presence of these antibodies can help confirm the diagnosis and determine the subtype of scleroderma.
Imaging studies, such as X-rays or CT scans, may be ordered to assess the extent of organ involvement in scleroderma. These tests can provide valuable information about the condition of the lungs, heart, and gastrointestinal tract. They can help identify any abnormalities or damage caused by the disease, guiding the treatment plan and monitoring the progression of scleroderma.
Skin biopsies are often performed to analyze skin tissue under a microscope. This procedure involves taking a small sample of affected skin and examining it for characteristic changes associated with scleroderma. The biopsy can help confirm the diagnosis and rule out other skin conditions that may present with similar symptoms.
In addition to these tests, your healthcare provider may also recommend other specialized exams or consultations with specialists, depending on the specific symptoms and organ involvement. These additional evaluations can provide a comprehensive understanding of the disease and its impact on your overall health.
Treatment Options for Scleroderma
Scleroderma is a chronic autoimmune disease that affects the connective tissues in the body. While there is currently no cure for scleroderma, there are various treatment options available to manage its symptoms and slow down disease progression. These treatment options can be categorized into medications, non-pharmacological therapies, and surgical interventions.
Medications for Scleroderma
One of the main approaches in managing scleroderma is through the use of medications. Your doctor may prescribe immunosuppressants, which work by reducing the activity of your immune system. By doing so, these medications can help control the immune response that leads to the thickening and hardening of the skin and other tissues.
In addition to immunosuppressants, anti-inflammatory drugs may also be prescribed to relieve pain and inflammation associated with scleroderma. These medications can help alleviate discomfort and improve overall quality of life for individuals with the condition.
Furthermore, medications that improve blood circulation and manage specific organ complications may be recommended. Scleroderma can affect various organs, such as the lungs, heart, kidneys, and gastrointestinal tract. Therefore, specific medications may be prescribed to address the unique challenges presented by each affected organ.
Non-Pharmacological Therapies
Alongside medications, non-pharmacological therapies can play a crucial role in managing scleroderma. Physical therapy, for example, can help improve joint mobility and muscle strength. Scleroderma can cause stiffness and limited range of motion, making it difficult to perform daily activities. Physical therapy exercises and techniques can help individuals regain and maintain their physical function.
Occupational therapy is another non-pharmacological therapy that can assist individuals in adapting their daily activities to reduce strain on affected areas. Occupational therapists can provide guidance on ergonomics, assistive devices, and energy conservation techniques. These interventions can help individuals with scleroderma continue to engage in meaningful activities and maintain their independence.
Complementary therapies, such as acupuncture, relaxation techniques, and mind-body exercises like yoga or tai chi, may also provide symptom relief and improve overall well-being. These therapies can help manage stress, reduce pain, and promote relaxation, which can be beneficial for individuals living with scleroderma.
Surgical Interventions
In certain cases, surgical interventions may be necessary to address specific complications of scleroderma. For example, if the condition affects the blood vessels in your fingers, amputation of affected areas may be required to prevent further tissue damage. Surgical interventions are typically considered when other treatment options have been exhausted or when there is a significant risk to the individual’s health.
Your healthcare team will assess your individual situation and discuss the potential benefits and risks of surgical interventions. It is important to have open and honest conversations with your healthcare provider to fully understand the treatment options available and make informed decisions about your care.
Living with Scleroderma
Scleroderma is a chronic autoimmune disease that affects the connective tissues in the body. Living with scleroderma requires making adjustments to your daily life to manage symptoms and maintain overall well-being. Here are some practical tips to help you navigate life with this condition:
Daily Life Adjustments
- Protect your skin from excessive sun exposure by wearing sunscreen with a high SPF and protective clothing. The ultraviolet rays from the sun can trigger flare-ups and worsen symptoms in individuals with scleroderma.
- Ensure proper hydration to prevent dryness and cracking of the skin. Drinking an adequate amount of water throughout the day can help maintain the moisture levels in your skin.
- Practice gentle skin care routines, using moisturizers to keep your skin hydrated. Look for products that are specifically formulated for sensitive skin and avoid harsh chemicals that can irritate your skin.
- Avoid extreme temperatures, as both hot and cold environments can worsen symptoms. Extreme heat can cause excessive sweating and lead to dehydration, while cold temperatures can constrict blood vessels and affect circulation.
- Engage in regular physical activity to maintain joint flexibility and overall physical fitness. Low-impact exercises like yoga, tai chi, and swimming can help improve flexibility, reduce stiffness, and promote cardiovascular health.
Emotional and Psychological Support
Living with a chronic condition like scleroderma can take a toll on your emotional well-being. It is important to seek emotional and psychological support to help cope with the challenges of the condition. Support groups, therapy, and counseling can provide a safe space to share experiences, receive guidance, and learn coping strategies. Connecting with others who understand what you are going through can provide a sense of belonging and reduce feelings of isolation.
Nutrition and Exercise Recommendations
A healthy diet and regular exercise are essential components of managing scleroderma. Here are some recommendations:
- Focus on a balanced diet rich in fruits, vegetables, lean proteins, and whole grains. These foods provide essential nutrients that support overall health and well-being.
- Adequate hydration is crucial for maintaining healthy skin and minimizing complications. Aim to drink at least 8 glasses of water per day. Consider incorporating hydrating foods like watermelon, cucumbers, and oranges into your diet.
- Regular exercise, such as low-impact activities like walking or swimming, can help maintain joint mobility and improve cardiovascular health. Consult with your healthcare team. Develop an exercise plan that suits your individual needs and abilities.
Living with scleroderma requires a multidisciplinary approach involving medical management, lifestyle modifications, and emotional support. By actively engaging in self-care and working closely with your healthcare team, you can effectively manage the condition and improve your quality of life. Remember, you are not alone in this journey, and there are resources available to support you every step of the way.
Use the CareClinic App to Manage Scleroderma Symptoms
Managing scleroderma effectively involves careful monitoring of symptoms, medications, and lifestyle adjustments. The CareClinic App is designed to empower you in this journey by providing a comprehensive platform to track your treatment regimen, monitor symptoms, and record your physical activities and dietary intake. With features like medication reminders, symptom tracking, and the ability to generate health reports, CareClinic helps you stay on top of your condition and communicate effectively with your healthcare team. By using CareClinic to track your progress and understand patterns in your health, you can make informed decisions that lead to improved health outcomes. Take control of your scleroderma management today by installing the CareClinic App.


