Does your family of a history of strokes? Are you worried about your risk level? Has someone in your family experienced a stroke? Are you overwhelmed with keeping track of their medications and nutritional requirements? Having an all-in-one app to help keep track of all these changes would help tremendously. Keep reading below to find out about the different assessments and scales such as the Stroke Impact Scale (SIS), the motor activity log (MAL), fatigue severity scale (FSS), SS-QOL, MFS, and even the ADL for stroke patients.
Table of Contents
- What is a Stroke?
- What are the Common Types of Strokes?
- What is a Cryptogenic Stroke?
- Symptoms & Risk Factors Associated with Stroke
- What are the Complications that Arise from Strokes?
- When Should you See a Doctor?
- Stroke Rehabilitation
- What is a Stroke Symptom Log?
- Stroke Impact Scale
- The Motor Activity Log
- The Fatigue Severity for Stroke Impact Scale
- The Stroke-Specific Quality of Life Scale
- The Motor Functioning for Stroke Impact Scale
- App for Stroke Impact Scale Health
- CareClinic helps manage post-stroke impact scale
What is a Stroke?
A stroke is a cerebrovascular disease. It occurs when the blood supply to part of your brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients. Your brain cells begin to die in minutes. Strokes are the fifth most common cause of death in the United States. Approximately 800,000 people have a stroke each year. Strokes can be fatal. When you experience a stroke, it can cause dizziness. This is because the stroke can damage the part of the brain that controls balance. Dizziness can also be a side effect of certain medications used to treat stroke.
What are the Common Types of Strokes?
There are three main types of strokes: Ischemic, Hemorrhagic and Transient Ischemic Attack (TIA). Each type of stroke is detailed below:
- Ischemic Stroke – This is the most common type of stroke. Approximately 87% of all people who experience strokes, will experience an ischemic stroke. A stroke occurs when a blood clot prevents oxygen from reaching the brain.
- Hematologic Disorders – these disorders involve the blood and include problems with red blood cells, white blood cells, platelets, bone marrow, lymph nodes, and the spleen.
- Hemorrhagic Stroke – This type of stroke occurs when a blood vessel ruptures. This causes blood to leak into the brain. Hemorrhagic strokes are usually the result of aneurysms or arteriovenous malformations (AVMs).
- Transient Ischemic Attack (TIA) – This type of stroke occurs when blood flowing to a part of the brain becomes inadequate for a brief period of time. Usually, normal blood flow resumes after a short period of time and symptoms disappear on their own. Most people call this a ministroke. A TIA is a warning sign of potential future strokes.
What is a Cryptogenic Stroke?
Another type of stroke that is less common is called a cryptogenic stroke. This means the stroke has an unknown cause despite extensive testing. About 1 in 3 strokes are cryptogenic in nature. There are some hidden causes that can lead to a cryptogenic stroke:
- Irregular heartbeat (atrial fibrillation) – Atrial Fibrillation (AFib) is a quivering or irregular heartbeat that can lead to blood clots, strokes and other complications.
- Heart structure problems – people born with holes in their hearts can have strokes if a blood clot forms between the walls of their arteries. For most people even with blood leaking from one atrium to another their lives remain unaffected. Due to the hole, however, blood clots and not filtered before the blood pumps into the circulation causing complications.
- Hardening of arteries (Large Atherosclerosis and cholesterol) – plaque or fatty deposits made up of cholesterol build up in your arteries. This causes the walls of your blood vessels to thicken and reduces blood flow. If the blocked artery supplies the heart or brain, a lack of oxygen and nutrients will lead to a stroke.
- Blood clotting disorder (Thrombophilia) – This is when your body causes excessive blood clotting or hypercoagulation. The clots form in the arteries or travel to them causing blockages. This ultimately can lead to a heart attack or stroke. The disorder can either be caused by excessive smoking, obesity, pregnancy or other external factors, or it is genetic.
Symptoms & Risk Factors Associated with Stroke
There are many symptoms and risk factors associated with strokes. Some of them are avoidable or changeable and some are not.
Symptoms for Stroke
- Trouble speaking and understanding what others say – you can experience confusion in understanding, slur your words or have difficulty talking
- Paralysis or numbness of the face, arm or leg – you can develop sudden numbness, weakness or even paralysis. This often affects only one side of your body and may cause that side to droop.
- Problems seeing in one or both eyes – you can suffer from blurred or blackened vision. You can also suffer from double vision.
- Headaches – you can experience a sudden, severe headache, which may be accompanied by vomiting or dizziness.
- Trouble walking – you can stumble or lose your balance. This can be caused by sudden dizziness or loss of coordination.
Risk Factors for Stroke
There are multiple categories of risk factors associated with strokes. From lifestyle to medical, these are some of the most common risks to keep in mind.
Lifestyle Factors
- Being overweight (obese)
- Being physically inactive
- Heavy (binge) drinking
- Use of illegal drugs such as cocaine, methamphetamine etc.
- Smoking cigarettes or inhaling second-hand smoke
Medical Factors
- High blood pressure
- High cholesterol
- Diabetes
- Obstructive sleep apnea
- Cardiovascular problems – heart failure, heart defects, heart infection, arrhythmia or atrial fibrillation
- Family history of stroke
- Personal history of stroke
Other Risks Related to Stroke
- Age – People above the age of 55 have a higher risk of stroke than younger people
- Race – The African-American community has a higher risk of stroke than other races
- Sex – Men have a higher risk of stroke than women. Women, however, usually experience strokes when they are older and hence are more likely to die of strokes than men
- Hormones – Using contraceptives such as birth control pills or hormone therapy increases the risk of stroke. Specifically, it is an increase in estrogen that causes an increased risk.
What are the Complications that Arise from Strokes?
Strokes cause complications. Many strokes have similar complications that arise. The most common of these are:
- Brain edema – Swelling of the brain
- Pneumonia – Causes breathing problems arising from a person’s inability to move.
- Urinary Tract Infection (UTI) – When stroke survivor loses control of their bladder, doctors place a urinary catheter to help them urinate. This catheter can cause infections.
- Seizures. – Commonly occurring in larger strokes, result from electrical activity in the brain, leading to convulsions.
- Clinical Depression – Changes and loss of movement can cause patients to experience unwanted emotional sadness.
- Bedsores – Being unable to move causes pressure ulcers to form.
- Deep Vein Thrombosis (DVT) – Blood clots form in the veins of legs due to immobility.
The best way to keep track of these complications is to use a stroke symptom activity tracker. A really great tracker is the CareClinic app that is multi-functional. The second half of the article will go into detail about the different features that will make tracking symptoms easier.
When Should you See a Doctor?
You must seek immediate attention if you notice any of the below-mentioned symptoms. Do not be fooled into thinking the stroke has disappeared if the symptoms recede after a point. Stroke symptoms are usually lingering. The best way to remember how to identify the symptoms is through the acronym “FAST”.
- Face – Ask the person to smile. Does one side of their face droop?
- Arms – Ask the person to raise both arms. Does one arm drop downwards or can they not raise one arm?
- Speech – Ask the person to repeat a simple sentence or phrase. Is their speech slurred or strange in any way?
- Time – If you observe one or a combination of these symptoms, call 911 immediately and request emergency medical assistance.
It is important to note when symptoms first appear. The best way to do that is to use a stroke symptom activity log. This information helps providers determine the best treatment moving forward. By keeping this acronym in mind and following the aforementioned steps, you could be saving someone’s life.
Stroke Rehabilitation
In some instances strokes are beatable. Rehabilitation is key to achieving a long and healthy life. Rehabilitation will take time so remember to celebrate the small victories along the way. There are many comprehensive guides to help stroke rehabilitation. From help with walking and talking, to easy-to-swallow food recipes, there are hundreds of stroke rehabilitation techniques to get you back on your feet. Some of the most common stroke rehabilitation techniques suggested by doctors are:
- Range of motion exercises & physical therapy
- Frequently turning in bed to prevent bedsores from forming
- Bladder training programs
- Swallowing and respiratory therapy such as deep breathing exercises
The most efficient way to keep track of how rehabilitation is going is through a stroke symptom activity log. By tracking changes in symptoms doctors will be able to tweak rehabilitation exercises with the most accuracy. This will help stroke survivors recover quicker and with higher chances of a full recovery.
What is a Stroke Symptom Log?
A stroke symptom activity log is a tracker that allows patients and caregivers the ability to track multiple areas related to strokes. Some of the most common areas to track are:
- Weight – losing weight lowers the risk of repeated stroked.
- Blood pressure – normal blood pressure helps lower cholesterol levels.
- Exercise Monitoring – regular exercise lowers the risk of heart disease which in turn lowers the risk of stroke.
- Communication – tracking slurred or strange speech can alert caregivers to signs of stroke faster.
- Orientation – dizziness or sudden disorientation can alert caregivers to signs of stroke faster.
- Plans can be customized for individual patients according to their needs.
Every stroke symptom activity log has the same functionality in many regards. CareClinic however goes above and beyond by adding a medication tracker, diary feature and so much more within the app. It has been mentioned a few times in the article already and by now you must be wondering, what is CareClinic? Keep reading to find out.
Stroke Impact Scale
The Stroke Impact Scale (SIS) is a 36-item patient-reported outcomes measure that assesses the physical, emotional, and social consequences of stroke. It has demonstrated its reliability and validity as a measure of stroke-related disability, with good convergent, discriminant, and known-groups validity. The Scale has found application in various stroke populations, including those with first-ever strokes, recurrent strokes, and ischemic or hemorrhagic strokes.
The Stroke Impact Scale measures the impact of stroke on patients’ daily lives and tracks changes in disability over time. It also compares the relative impact of stroke on different subgroups of patients, such as those with different types of strokes or different levels of disability. Additionally, the SIS assesses the efficacy of rehabilitation interventions and compares the outcomes of different treatments.
The SIS consists of 36 items that are clustered into three subscales: physical, emotional, and social. Each item is rated on a 5-point scale, with higher scores indicating a greater impact. The physical subscale assesses the effects of stroke on patients’ physical functioning, including activities of daily living, mobility, and pain. The emotional subscale assesses the effects of stroke on patients’ mood and emotions, including depression, anxiety, and frustration. The social subscale assesses the effects of stroke on patients’ social functioning, including communication, social activities, and relationships.
The SIS exhibits good psychometric properties and allows measuring the impact of stroke on patients’ daily lives. It is a reliable and valid measure of stroke-related disability, enabling the tracking of changes in disability over time, comparing the relative impact of stroke on different subgroups of patients, and assessing the efficacy of rehabilitation interventions. CareClinic comes with built-in health assesments and individual trackers which allow you to measure various health indicators individually as well. Such as a Symptom tracker, Mood tracker and even the IADL and ADL assessments required for stroke patients. They can also be viewed remotely without errors by the caregiver or the dependent. This is why we recommend trying the CareClinic app.
The Motor Activity Log
Motor Activity Log is a structured observation measure that assesses the frequency and severity of motor impairments following a stroke. The MAL has good inter-rater reliability and convergent validity with other measures of motor functioning. The MAL is a useful tool for assessing motor impairments following stroke and tracking changes in motor functioning over time.
The Motor Activity Log consists of three subscales: the Motor Impairment Scale (MIS), the Frequency Scale (FS), and the Severity Scale (SS). The MIS assesses the frequency of motor impairments, including incoordination, tremor, spasticity, and dysarthria. The FS assesses the severity of motor impairments, including strength, range of motion, and dexterity. The SS assesses the severity of motor impairments, including balance, gait, and coordination.
The MAL is a useful tool for assessing motor impairments following stroke and tracking changes in motor functioning over time. The MAL allows comparing the relative severity of motor impairments in different subgroups of patients, assessing the efficacy of rehabilitation interventions, and tracking changes in motor functioning over time. CareClinic also includes a structured observation tool for tracking Motor Activity, which serves the same purpose. This tool is linked with the exercises section, enabling patients to log their progress and observe improvements over time.
The Fatigue Severity for Stroke Impact Scale
The Fatigue Severity Scale (FSS) is a 9-item self-report measure of fatigue severity. FSS has good reliability and validity and can be used to assess fatigue in a variety of populations, including stroke patients. The FSS asks patients to rate the severity of their fatigue on a 7-point scale, with higher scores indicating greater fatigue severity. It has three subscales: the Physical Fatigue Scale (PFS), the Mental Fatigue Scale (MFS), and the Activity Level Scale (ALS). The PFS assesses the physical symptoms of fatigue, including tiredness, weakness, and muscle pain. The MFS assesses the mental symptoms of fatigue, including forgetfulness, difficulty concentrating, and feeling mentally exhausted. The ALS assesses the impact of fatigue on patients’ daily activities, including work, leisure activities, and social interactions.
The FSS provides a reliable and valid measure of fatigue severity that enables tracking changes in fatigue over time, comparing the relative severity of fatigue in different subgroups of patients, and assessing the efficacy of rehabilitation interventions. CareClinic also offers a fatigue tracker that measures and tracks changes in fatigue over time. The fatigue tracker is linked to the exercises section, allowing patients to log their progress and observe improvements over time.
The Stroke-Specific Quality of Life Scale
The Stroke-Specific Quality of Life Scale (SS-QOL) is a 28-item self-report measure of the quality of life following a stroke. The SS-QOL has good reliability and validity and can be used to assess the quality of life in a variety of populations, including stroke patients.
The SS-QOL consists of four subscales: the Physical Health Scale (PHS), the Emotional Well-Being Scale (EWS), the Social Functioning Scale (SFS), and the Stroke-Specific Concerns Scale (SSCS). The PHS assesses physical health, including mobility, self-care, and pain. The EWS assesses emotional well-being, including depression, anxiety, and mood. The SFS assesses social functioning, including leisure activities and interpersonal relationships. The SSCS assesses stroke-specific concerns, such as worry about having another stroke and fear of disability.
The SS-QOL is a reliable and valid measure of the quality of life following a stroke. You can use it to track changes in quality of life over time, compare the relative severity of different domains of quality of life in different subgroups of patients, and assess the efficacy of rehabilitation interventions. CareClinic also features a structured observation tool for tracking Quality of Life, which serves the same purpose. This tool is linked with the exercises section, allowing patients to log their progress and observe improvements over time.
The Motor Functioning for Stroke Impact Scale
The Motor Functioning Scale (MFS) is a 12-item self-report measure of motor functioning following a stroke. The MFS has good reliability and validity and can be used to assess motor functioning in a variety of populations, including stroke patients.
The MFS consists of three subscales: the Motor Activity Scale (MAS), the Motor Coordination Scale (MCS), and the Strength and Endurance Scale (SES). The MAS assesses patients’ ability to perform basic motor activities, such as reaching, grasping, and turning. The MCS assesses patients’ ability to coordinate their movements, such as when dressing or eating. The SES assesses patients’ strength and endurance, including their ability to walk and stand.
The MFS is a reliable and valid measure of motor functioning following a stroke. You can use it to track changes in motor functioning over time and compare the relative severity of different domains of motor functioning in different subgroups of patients. CareClinic also offers an observation tool for tracking Motor Functioning, which serves the same purpose.
The CareClinic platform provides a range of tools for assessing motor, cognitive, and emotional functioning following a stroke. These tools enable tracking changes in functioning over time, comparing the relative severity of impairments in different subgroups of patients, and assessing the efficacy of rehabilitation interventions.
App for Stroke Impact Scale Health
The CareClinic app is an all-in-one care app. Anyone can use and access the interface 24 hours a day. The most important feature of the app is the ability to use a diary, medication tracker, and nutrition tracker. You can also build individualized care plans. A unique feature within the app is the ability to add caregivers and doctors to any care plan you create. This feature allows easy tracking, especially for a stroke symptom activity log, which needs to be constantly monitored and updated, between multiple people. The app helps keep everyone on the same page about overall treatment plans.
Diary Entries for Stroke Impact Scale
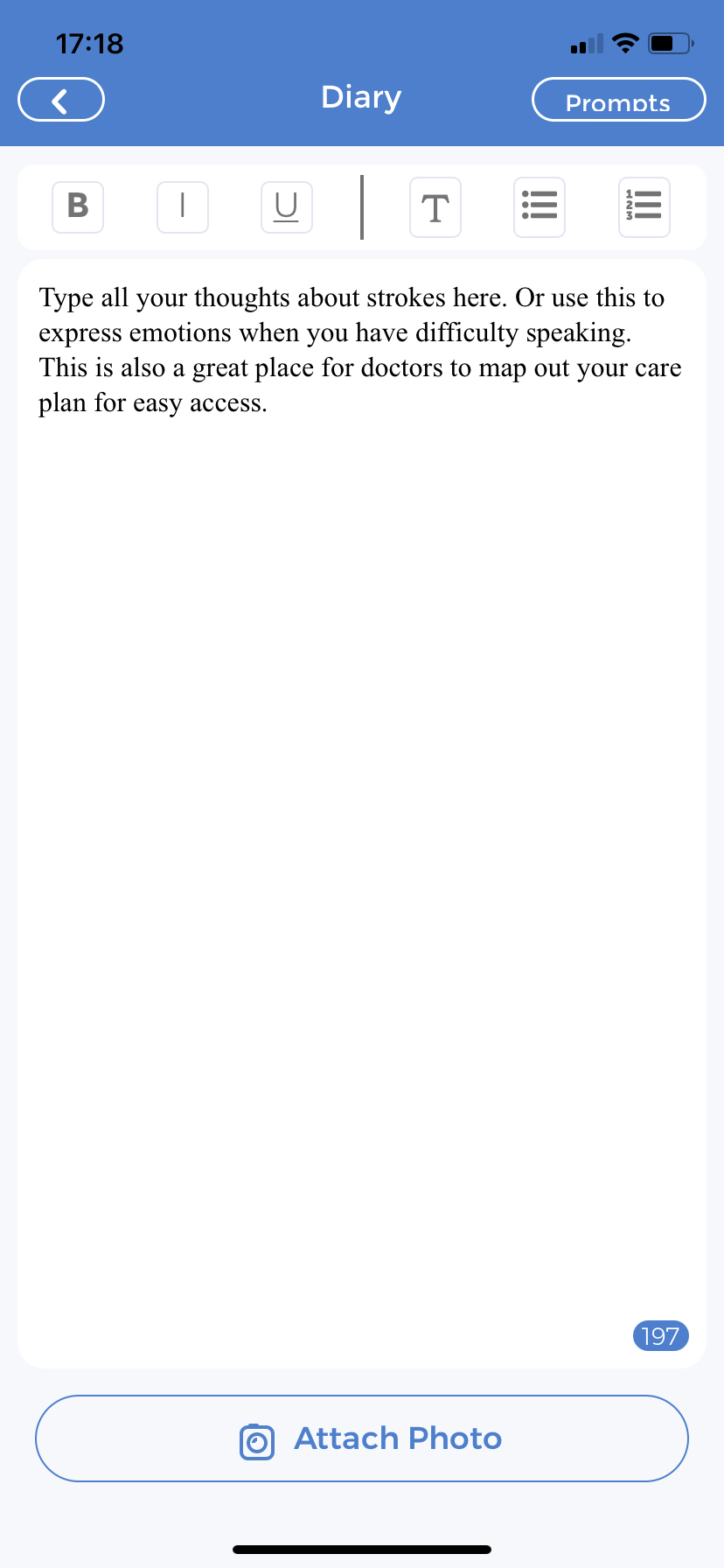 You can type up to 144 words per entry and post an unlimited number of entries per day. This is useful when you need to quickly jot down a new symptom or changes in mood or behavior. Having a stroke can also take a toll on your mental health. The premium account has access to 16 journal prompts, and each prompt focuses on different aspects of mental health. Typing out your thoughts can be a healthy way to deal with your emotions associated with the complications of having a stroke. You can bold, italicize, and underline important statements. Add photos to compare symptoms or alert your doctor to changes in your body that may be caused by the stroke. Pictures are the best way to personalize your entries.
You can type up to 144 words per entry and post an unlimited number of entries per day. This is useful when you need to quickly jot down a new symptom or changes in mood or behavior. Having a stroke can also take a toll on your mental health. The premium account has access to 16 journal prompts, and each prompt focuses on different aspects of mental health. Typing out your thoughts can be a healthy way to deal with your emotions associated with the complications of having a stroke. You can bold, italicize, and underline important statements. Add photos to compare symptoms or alert your doctor to changes in your body that may be caused by the stroke. Pictures are the best way to personalize your entries.
The best part? You can write and add as many entries as you want in one day. They will automatically save for you to return and continue the next day. You can also revisit previously written journal entries at any point in time. Every one of them is readily available on the app.
Symptom Tracking for Stroke Impact Scale
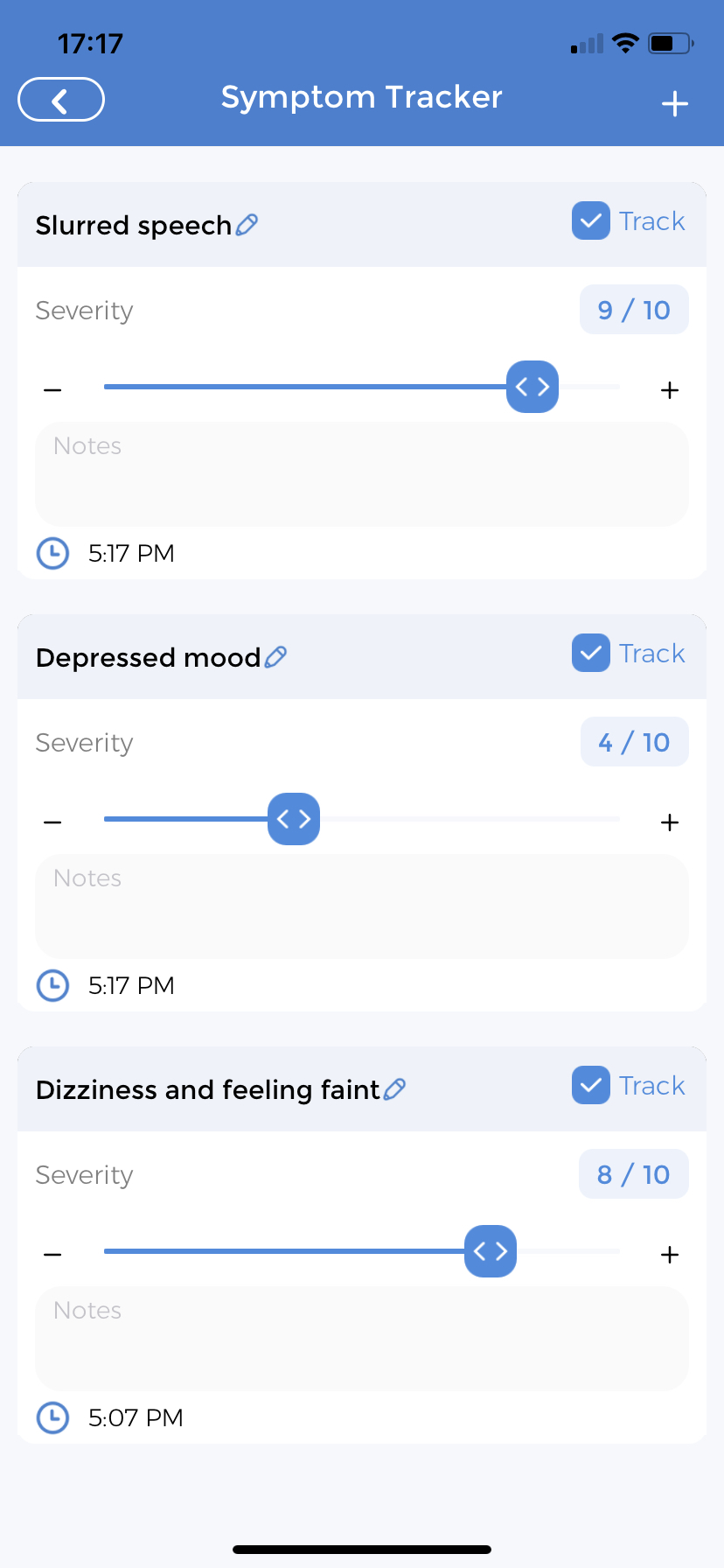
You can add whatever symptoms you would like to track ranging from headaches to sexual dysfunction. The tracker will ask when the symptom first started. You can go back years or add new symptoms experienced every day. The page will then ask to link to an “Existing Care Plan”. Then asks for “Notes” and “Frequency” of symptoms – how many days a week and how many times a day do you feel certain symptoms; headache, slurred speech etc. You can even add a reminder for the app to prompt how you are feeling as often as you’d like.
The app will ask for the severity of the symptom being tracked on a 10-point scale and will allow the addition of additional notes every day. If you do not remember to track something, the app will remind you. The best part you are not the only person with access to the symptom tracker. By giving permission to a trusted caregiver, they too can go into the app on their own phones or tablets and add symptoms as they deem fit. Information is power and the more information your doctor has access to, the better they can treat you.
Nutritional Tracking
![]() The nutrition tracker allows you to add all food you have consumed throughout the day. By tracking your calories and macronutrients you can ensure a healthy diet. Ensuring a healthy well-balanced diet reduces the risk of heart disease, leads to lower chances of obesity and keeps cholesterol in check. All of these problems are symptoms that add to the likelihood of stroke. Since the app is available 24 hours a day, and right at your fingertips, you can conveniently add foods as you consume them. The nutrition tracker also allows your caregivers and doctors to have a baseline understanding of your diet. How it needs to change to ensure you stay healthy. It also immensely helps with stroke rehabilitation.
The nutrition tracker allows you to add all food you have consumed throughout the day. By tracking your calories and macronutrients you can ensure a healthy diet. Ensuring a healthy well-balanced diet reduces the risk of heart disease, leads to lower chances of obesity and keeps cholesterol in check. All of these problems are symptoms that add to the likelihood of stroke. Since the app is available 24 hours a day, and right at your fingertips, you can conveniently add foods as you consume them. The nutrition tracker also allows your caregivers and doctors to have a baseline understanding of your diet. How it needs to change to ensure you stay healthy. It also immensely helps with stroke rehabilitation.
Individualized Care Plans
One of the most unique features of the CareClinic app is your ability to create an individualized care plan that works best for you. All the features mentioned above become part of the care plan. You can also add medications, sleep cycles, and more. The ability to individualize all these features allows your caregivers and doctors to change any aspect of the care plan at any time. This means the plan will work best for you throughout the course of treatment. Tracking progress is extremely important to recovery and this feature allows you to do just that.
CareClinic helps manage post-stroke impact scale
Dealing with strokes, stroke survivors and family members is hard. By getting in touch with your doctor early and having regular check-ups you can possibly avoid having a stroke. If you have already suffered from one, having a good, reliable logging App will help make your or your dependents’ life easier.