Ulcerative colitis flare-ups, a hallmark of this chronic inflammatory bowel disease, involve the immune system mistakenly attacking the colon and rectum tissues, causing inflammation and ulcers. Environmental factors like diet and stress contribute to these flare-ups, with certain foods and psychological stress often worsening the symptoms. To combat these disruptions, understanding how to manage UC is critical. Annually, 10 to 24 per 100,000 people receive a UC diagnosis. Managing flare-ups is crucial for these patients. This guide explores UC flare-ups’ development, symptoms, diagnosis, and treatment. It provides insights and advice for the affected individuals.[1][2][3]
Pathogenesis of UC Flare-Ups
Understanding the causes and symptoms of UC flare-ups is crucial for those living with this challenging condition. Experts believe a complex interplay of genetic and environmental factors triggers an immune response that leads to inflammation within the intestinal lining, although the exact cause remains elusive.
The immune system and gut microbiome significantly impact UC flare-ups. This microbiome contains trillions of bacteria essential for gut balance. In UC patients, dysbiosis—an imbalance—often occurs. There’s a decrease in beneficial bacteria and a rise in harmful ones. Dysbiosis triggers an abnormal immune response. This response causes inflammation and intestinal lining damage. Such damage is what leads to a UC flare-up.
Pro-inflammatory cytokines like TNF-alpha and IL-6 are also implicated in UC flare-ups. Immune cells produce these cytokines when environmental triggers occur. They are pivotal in starting and worsening UC inflammation. During a flare-up, cytokine production rises, aggravating UC symptoms.
In addition to immune dysregulation and cytokine production, other elements may contribute to UC flare-ups, like the use of nonsteroidal anti-inflammatory drugs (NSAIDs), which may induce intestinal inflammation. Stress can also be a trigger for UC flare-ups, as it can alter gut microbiota composition and increase inflammation. Dietary factors, such as high-fat, low-fiber diets, have been linked to a higher risk of UC flare-ups.[4][5][6]
Ulcerative Colitis Flare Up Symptoms
UC symptoms can differ from person to person and range in severity. Some may experience mild symptoms, while others might require hospitalization. During a UC flare-up, symptoms can worsen, and new ones may appear. Here are some common symptoms of UC flare-ups:
- Abdominal pain and cramping: Ranging from mild discomfort to severe pain, abdominal pain is a common symptom, often accompanied by cramping.
- Diarrhea: A hallmark symptom of UC flare-ups, diarrhea may be accompanied by urgency – the sudden and intense need to have a bowel movement.
- Rectal bleeding: Ranging from mild to severe, rectal bleeding can be visible in the stool or on toilet paper.
- Weight loss: A decrease in appetite, malabsorption, and loss of nutrients through diarrhea may lead to weight loss during a flare-up.
- Fatigue: Inflammation, anemia, and poor sleep quality due to frequent bathroom trips can cause fatigue.
- Joint pain: Though less common, painful and swollen joints may occur due to inflammation.
- Skin rash: Skin rashes may develop during a flare-up, potentially due to skin inflammation.
- Eye inflammation: Uveitis, or inflammation in the eye, may occur during a flare-up.
Individuals with UC need proper medical care to manage symptoms and prevent complications. Understanding the causes and symptoms of UC flare-ups is crucial. Patients can then collaborate with healthcare providers to tailor a treatment plan. This collaboration aims to maintain a better quality of life.
Diagnosis of UC Flare-Ups
The diagnosis of UC flare-ups typically begins with a thorough medical history and physical exam by a healthcare provider. The healthcare provider will ask about the patient’s symptoms, medical history, and family history, as well as perform a physical exam that may include a rectal exam to assess for signs of inflammation and ulceration in the rectum.
If UC flare-ups are suspected based on the patient’s symptoms and physical exam, the healthcare provider may order several diagnostic tests to confirm the diagnosis and assess the severity of the disease. These may include:
- Blood tests: Blood tests can help to detect signs of inflammation and anemia (low red blood cell count) which may occur during a UC flare-up.
- Stool tests: Stool tests can help to rule out other conditions that may cause similar symptoms, such as infections.
- Colonoscopy: A colonoscopy is a procedure that involves inserting a flexible tube with a camera into the rectum and colon to examine the lining of the intestine. During a colonoscopy, biopsies (small tissue samples) may also be taken to confirm the diagnosis of UC and assess the severity of the disease.
- Imaging tests: Imaging tests, such as CT scans or MRI, may be used to evaluate the extent and severity of inflammation in the colon and rectum.
Once a diagnosis of UC flare-ups is confirmed, the healthcare provider will work with the patient to develop a treatment plan based on the severity of the disease and the patient’s individual needs. Treatment may involve medications, lifestyle modifications, or surgery in more severe cases.
Individuals with UC need to receive regular check-ups and monitoring to manage their symptoms and prevent flare-ups. This may involve regular colonoscopies to assess the extent of the disease and monitor for signs of complications.[7][8][9][10][11]
How to Manage UC Flare Up Symptoms
The management of UC flare-ups involves a combination of medication and lifestyle modifications. The goals of treatment are to reduce inflammation, relieve symptoms, and prevent complications.
Medications
 The mainstay of treatment for UC flare-ups is medications that help to reduce inflammation and manage symptoms. The choice of medication depends on the severity of the disease, the location of the inflammation in the colon, and the patient’s individual needs.
The mainstay of treatment for UC flare-ups is medications that help to reduce inflammation and manage symptoms. The choice of medication depends on the severity of the disease, the location of the inflammation in the colon, and the patient’s individual needs.- Aminosalicylates: Aminosalicylates are a first-line treatment for mild to moderate UC flare-ups. These are anti-inflammatory medications that are used to treat mild to moderate UC flare-ups. They work by reducing inflammation in the colon and rectum. Examples include mesalamine, sulfasalazine, and olsalazine.
- Corticosteroids treat moderate to severe UC flare-ups as powerful anti-inflammatory medications. They suppress the immune system and reduce inflammation in the colon and rectum, providing relief during more severe flare-ups. Prednisone and budesonide are examples of such corticosteroids.
- Immunomodulators: These are medications that work by suppressing the immune system to reduce inflammation in the colon and rectum. Examples include azathioprine and 6-mercaptopurine.
- Biologic agents: These are medications that target specific proteins in the immune system that are responsible for inflammation. Examples include infliximab, adalimumab, and vedolizumab. Immunomodulators and biological agents are used in more severe or refractory cases.
Diet
High-Fiber Foods
Healthcare providers often recommend high-fiber foods for individuals with ulcerative colitis (UC) as they promote regular bowel movements and can reduce inflammation in the digestive tract. However, it’s crucial to recognize that these same high-fiber foods may trigger symptoms in some UC patients, particularly during flare-ups.
Here are some examples of high-fiber foods that may be beneficial for people with UC:
- Fruits and vegetables: These are rich in fiber, vitamins, and minerals. Some examples include apples, bananas, oranges, broccoli, carrots, and sweet potatoes.
- Whole grains: These are high in fiber and other nutrients. Some examples include brown rice, quinoa, oatmeal, and whole-grain bread.
- Legumes: These are a good source of plant-based protein and fiber. Some examples include lentils, chickpeas, and black beans.
It is important to note that not all high-fiber foods are created equal. Some people with UC may be more sensitive to certain types of fiber, such as insoluble fiber found in wheat bran and some vegetables. In general, it is best to introduce high-fiber foods slowly and in small quantities and to monitor your symptoms closely to see how your body reacts.
Low-Residue Diet
A low-residue diet is a dietary approach that limits the intake of foods that are high in fiber and difficult to digest. It is best for people with ulcerative colitis during flare-ups, as it can help reduce inflammation in the digestive tract and alleviate symptoms such as diarrhea and abdominal pain.
Diet Guidelines
- Limit high-fiber foods: Foods that are high in fiber, such as fruits, vegetables, whole grains, and legumes, should be limited or avoided. Instead, choose low-fiber alternatives such as white rice, white bread, and refined cereals.
- Choose low-fat foods: High-fat foods can exacerbate UC symptoms, so it is best to choose lean proteins and low-fat dairy products.
- Avoid spicy foods: Spicy foods can irritate the digestive tract and worsen UC symptoms, so it is best to avoid them during flare-ups.
- Cook fruits and vegetables: Cooking fruits and vegetables can help make them easier to digest, so it may be beneficial to choose cooked or canned fruits and vegetables instead of raw.
- Drink plenty of fluids: It is important to stay hydrated while on a low-residue diet, so be sure to drink plenty of water and other fluids.
Hydration
Hydration is important for people with ulcerative colitis, especially during flare-ups. Diarrhea, a common symptom of UC flare-ups, can cause dehydration, which can worsen symptoms and lead to other health problems.
It is recommended that people with UC drink plenty of fluids, such as water, herbal tea, and clear broths, throughout the day to maintain hydration. Sports drinks and electrolyte solutions may also be beneficial for those experiencing severe dehydration. It is important to avoid drinks that are high in sugar or caffeine, as they can further aggravate symptoms.
In addition to drinking fluids, eating water-rich foods such as fruits and vegetables can also help maintain hydration. People with UC should aim to consume at least 8-10 glasses of fluids per day or more if they are experiencing diarrhea or other symptoms that increase fluid loss.
Different types of colitis can affect your digestive system in similar ways. If you have lymphocytic colitis, you might find that certain foods trigger your symptoms just like with UC. Learning about a lymphocytic colitis diet can help you understand which foods to avoid and which ones might actually help reduce inflammation.
It is important to consult with a healthcare provider to determine the appropriate fluid intake for your individual needs.
Stress Management
Stress can exacerbate symptoms during UC flare-ups, so stress management techniques such as relaxation exercises, meditation, and therapy may help manage symptoms.
- Relaxation exercises: Techniques such as deep breathing, progressive muscle relaxation, and guided imagery can help to reduce stress and manage symptoms during UC flare-ups.
- Meditation: Mindfulness meditation can help to reduce stress and promote relaxation, which can improve symptoms of UC flare-ups.
- Therapy: Talking to a therapist can help to manage stress and anxiety related to UC, which can improve overall well-being and reduce symptoms.
Surgery
Surgeons perform colectomy, the removal of the colon and rectum, as a last resort for ulcerative colitis (UC) patients with severe symptoms or complications unresponsive to medical treatment. This surgery comes in two primary forms:
Proctocolectomy with ileostomy: This procedure involves removing the entire colon and rectum and creating a stoma in the abdominal wall. The surgeon brings the end of the small intestine through this stoma, and an external pouch collects waste.
Proctocolectomy with ileal pouch-anal anastomosis (IPAA): Here, surgeons remove the colon and rectum but connect a newly created pouch from the small intestine to the anus, preserving normal waste elimination.
Enhanced Quality of Life: Post-surgery, many UC patients experience a significant improvement in quality of life, no longer having to deal with the constant worry and discomfort of flare-ups, although adapting to life with an ileostomy or internal pouch may take time and adjustment.
Long-term Support: Postoperative care includes support from dietitians, stoma care nurses, and psychologists to help patients adjust to the changes in their bodies and lifestyles, ensuring they have the resources for a smooth transition post-surgery.
Surgery, while effective at alleviating UC symptoms and potentially serving as a cure, is complex and requires considerable recovery time, with risks like bleeding, infection, and blockages.
Regular Check-Ups
Appointments
Here are some of the key aspects of regular check-ups for people with UC:
- Symptom assessment: During check-ups, your healthcare provider will ask you about any new or worsening symptoms, such as abdominal pain, diarrhea, or rectal bleeding. They may also ask about other symptoms that can be associated with UC, such as joint pain or skin rashes.
- Physical exam: Your healthcare provider will perform a physical exam to assess your overall health and check for signs of inflammation or other complications related to UC. They may also perform a digital rectal exam to check for inflammation or other abnormalities in the rectum.
- Diagnostic tests: Depending on your symptoms and disease activity, your healthcare provider may order diagnostic tests to assess the extent of inflammation in your colon and rectum. These tests may include stool tests, blood tests, imaging studies, and endoscopies.
- Treatment adjustment: Based on the results of your check-up, your healthcare provider may adjust your treatment plan to manage your symptoms and prevent further flare-ups. This may include changes to your medication regimen, adjustments to your diet, or recommendations for stress management techniques.
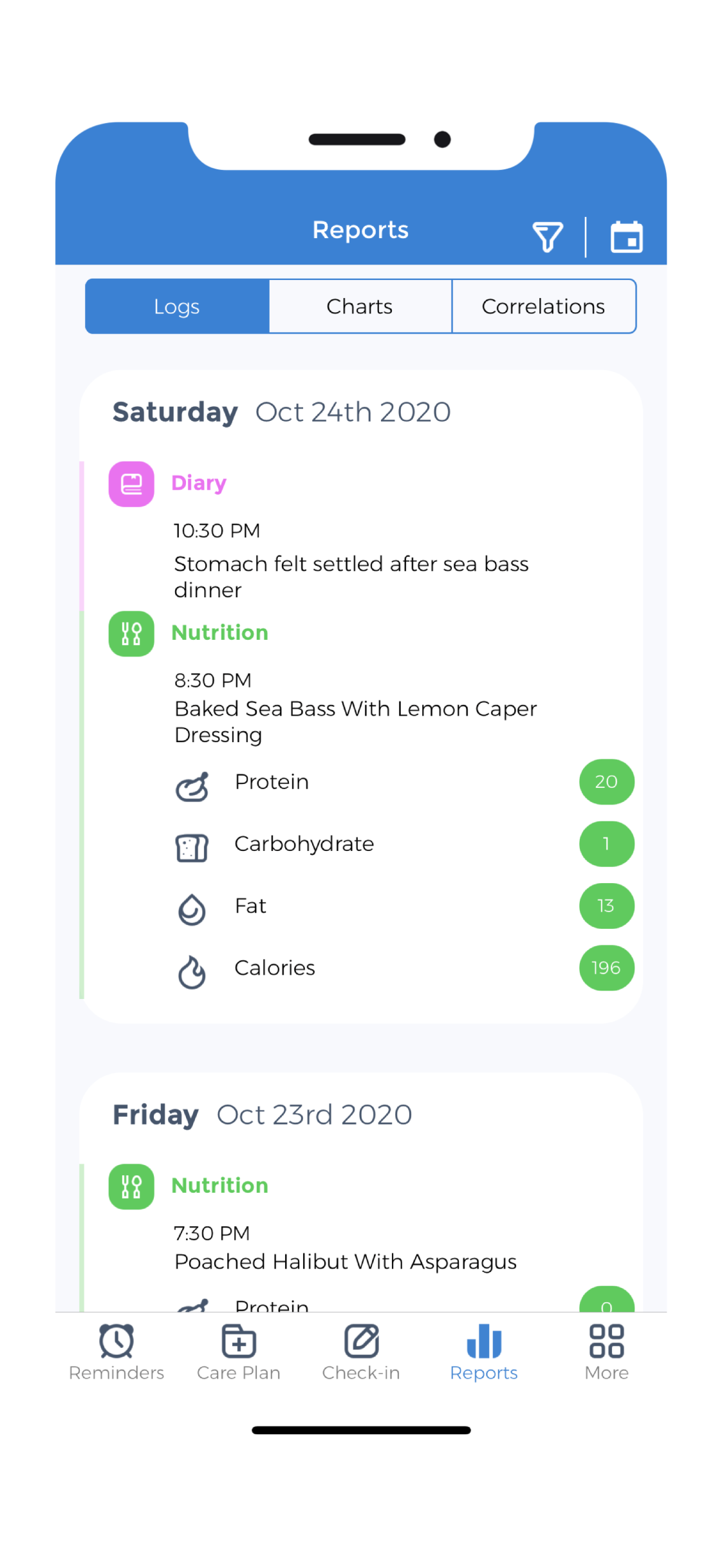
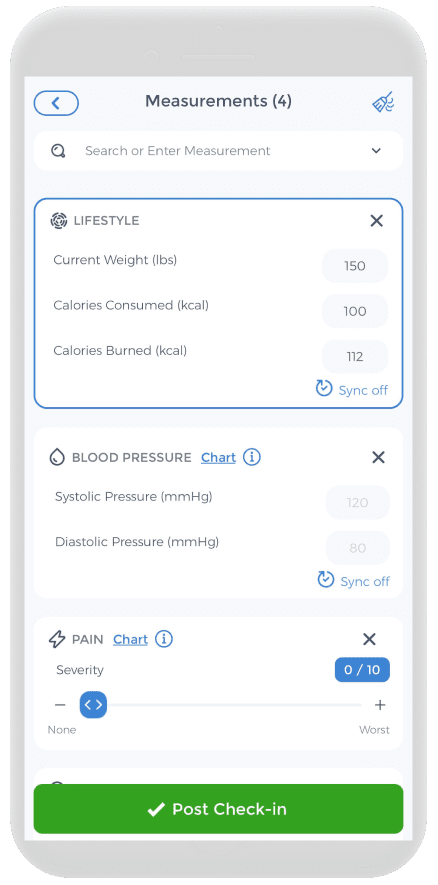
Regular check-ups play a critical role in managing Ulcerative Colitis (UC), enabling you to monitor your symptoms and disease activity closely. If you live with UC, actively collaborating with your healthcare provider to create a personalized check-up schedule is crucial. Using a health tracker app, such as CareClinic, can help you vigilantly observe your symptoms, oversee your diet and medication, and maintain a log of doctor’s visits and test outcomes. This diligent tracking equips you with the information necessary to manage your condition effectively and provides your healthcare team with vital data to guide treatment decisions.
UC Flare Ups
Ulcerative colitis (UC) consistently inflames the bowel, causing abdominal pain, frequent bowel movements, and other symptoms that disrupt daily life. However, active management involving medications, dietary modifications, stress reduction, and regular medical consultations can mitigate these flare-ups and promote better health.
Patients with UC need to work closely with their healthcare team to craft a personalized treatment plan. This plan often combines anti-inflammatory drugs, and specific dietary changes to minimize symptoms and improve nutrient uptake, such as following a low-residue diet, and stress management practices like meditation. Regular check-ups are also vital to monitor the disease’s progression or any arising complications.
Healthcare teams play a vital role in aiding UC patients. They use tools like health tracker apps for better disease management. Patients can thus manage their condition effectively. Despite UC’s incurable nature, treatments are available. These treatments manage symptoms well. They also lower the risks of complications. As a result, patients can enjoy fulfilling, healthy lives.[14]
References
- “Ulcerative Colitis Basics | IBD | CDC”. https://www.cdc.gov/inflammatory-bowel-disease/about/ulcerative-colitis-uc-basics.html
- “”. https://www.nhs.uk/conditions/ulcerative-colitis/
- “Epidemiology of Ulcerative Colitis | Clinical Guidance | Healio”. https://www.healio.com/clinical-guidance/ulcerative-colitis/epidemiology-overview
- “Ulcerative colitis: Recent advances in the understanding of disease pathogenesis – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC7194476/
- “5 Factors That Can Affect Ulcerative Colitis Flares – Clinical Advisor”. https://www.clinicaladvisor.com/news/5-factors-that-can-affect-ulcerative-colitis-flares/
- “Influence of Environmental Factors in the Development and Outcomes of Inflammatory Bowel Disease – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC6469265/
- “Ulcerative Colitis: Therapeutic Management Update”. https://www.uspharmacist.com/article/ulcerative-colitis-therapeutic-management-update
- “Second European evidence-based consensus on the diagnosis and management of ulcerative colitis Part 1: Definitions and diagnosis | Journal of Crohn's and Colitis | Oxford Academic”. https://academic.oup.com/ecco-jcc/article/6/10/965/503827
- “Strategies for the Care of Adults Hospitalized for Active Ulcerative Colitis – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC4226798/
- “Ulcerative colitis – Diagnosis and treatment – Mayo Clinic”. https://www.akamai.mayoclinic.org/diseases-conditions/ulcerative-colitis/diagnosis-treatment/drc-20353331
- “Official journal of the American College of Gastroenterology | ACG”. https://journals.lww.com/ajg/fulltext/2019/03000/acg_clinical_guideline__ulcerative_colitis_in.10.aspx
- “Table: Medications That Reduce Bowel Inflammation Caused by Ulcerative Colitis-Merck Manual Consumer Version”. https://www.merckmanuals.com/home/multimedia/table/medications-that-reduce-bowel-inflammation-caused-by-ulcerative-colitis
- “Ulcerative Colitis – American College of Gastroenterology”. https://gi.org/topics/ulcerative-colitis/
- “Living with | NICS Well”. https://www.nicswell.co.uk/conditions-and-treatments/ulcerative-colitis/living-with