Thoracic Outlet Syndrome (TOS) is a condition that affects the nerves and blood vessels in the upper body. It occurs when the thoracic outlet, a narrow space between the neck and shoulder, becomes compressed or irritated. This can lead to a variety of symptoms and potentially impact a person’s daily life. By understanding the symptoms of TOS, individuals can seek early diagnosis and appropriate treatment to manage the condition effectively.[1]
What is Thoracic Outlet Syndrome?
Thoracic Outlet Syndrome (TOS) refers to a group of disorders caused by the compression or irritation of the nerves and/or blood vessels in the thoracic outlet region. The thoracic outlet is a small space located between the collarbone (clavicle) and the first rib. It serves as a passageway for important structures, including nerves, blood vessels, and muscles.
When the nerves or blood vessels in this area become compressed or irritated, it can lead to a range of symptoms. The three main types of TOS include neurogenic TOS, vascular TOS, and non-specific or disputed TOS.
The Anatomy of the Thoracic Outlet
The thoracic outlet is a complex area that consists of several structures. It includes the brachial plexus, a network of nerves that originates from the neck and supplies sensation and movement to the upper extremities. The subclavian artery and vein, which provide blood supply to the arm, also pass through this area. Additionally, several arm and shoulder muscles, including the scalenes and pectoralis minor, play a role in stabilizing and moving the shoulder and arm.
Let’s take a closer look at the brachial plexus. It is formed by the union of the ventral rami (branches) of the lower four cervical nerves (C5-C8) and the first thoracic nerve (T1). These nerves come together to form a complex network that gives rise to various branches, which then innervate different muscles and provide sensation to specific areas of the upper limb. The brachial plexus is a vital component of the nervous system, allowing us to perform intricate movements and perceive sensations in our arms and hands.
Now, let’s focus on the subclavian artery and vein. The subclavian artery is a major blood vessel that arises from the aorta, the largest artery in the body. It travels through the thoracic outlet before continuing into the arm, where it branches off into smaller arteries that supply oxygenated blood to various tissues. The subclavian vein, on the other hand, is responsible for returning deoxygenated blood from the arm back to the heart. Together, the subclavian artery and vein ensure proper blood circulation in the upper limb.
Common Causes of Thoracic Outlet Syndrome
There are a variety of risk factors that can contribute to developing Thoracic Outlet Syndrome [1]. In many cases, it is caused by anatomical variations or abnormalities that can compress or irritate the nerves and blood vessels in the thoracic outlet. These may include:
- Abnormal cervical ribs or extra ribs
- Tightening of muscles in the neck and shoulder region
- Trauma or injury to the area
- Poor posture
Let’s delve deeper into the causes of TOS. Abnormal cervical ribs or extra ribs refer to additional ribs that may develop in the cervical (neck) region. These extra ribs can put pressure on the nerves and blood vessels in the thoracic outlet, leading to symptoms of TOS. It is important to note that not everyone has these extra ribs, and they are considered a variation of normal anatomy.
Tightening of muscles in the neck and shoulder region can also contribute to TOS. When these muscles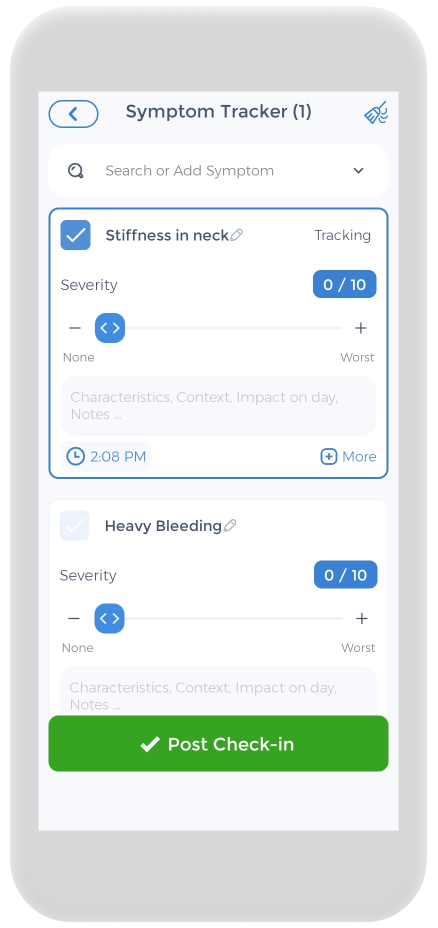 become overly tense or contracted, they can compress the nerves and blood vessels in the thoracic outlet. This can occur due to various reasons, such as prolonged poor posture, repetitive movements, or muscle imbalances. It is crucial to maintain proper posture and engage in regular stretching and strengthening exercises to prevent muscle tightness in this area.
become overly tense or contracted, they can compress the nerves and blood vessels in the thoracic outlet. This can occur due to various reasons, such as prolonged poor posture, repetitive movements, or muscle imbalances. It is crucial to maintain proper posture and engage in regular stretching and strengthening exercises to prevent muscle tightness in this area.
Trauma or injury to the thoracic outlet can result in TOS. This can happen due to accidents, falls, or repetitive activities that put excessive strain on the area. In some cases, the trauma may cause structural damage, such as fractures or dislocations, which can directly compress or irritate the nerves and blood vessels.
Poor posture is another common cause of TOS. Slouching or hunching forward can lead to a forward head position and rounded shoulders, which can put pressure on the thoracic outlet. Maintaining good posture, with the head aligned over the shoulders and the shoulders back and relaxed, can help alleviate stress on the nerves and blood vessels in this area.[2][3]
Recognizing the Symptoms of Thoracic Outlet Syndrome
The symptoms of Thoracic Outlet Syndrome can vary depending on the type and severity of the condition. It is important to recognize these symptoms to seek appropriate medical attention and management strategies. The two main types of TOS, neurogenic and vascular, present with distinct sets of symptoms.
Neurogenic Thoracic Outlet Syndrome Symptoms
Neurogenic Thoracic Outlet Syndrome occurs when the nerves in the thoracic outlet are compressed or irritated. This can result in symptoms such as:
- Pain or aching in the neck, shoulder, or arm
- Numbness or tingling in the fingers or hand
- Weakening grip strength
- Muscle wasting in the hand
- Difficulty performing fine motor tasks
When the nerves in the thoracic outlet are compressed or irritated, it can cause a range of symptoms that can significantly impact an individual’s daily life. The pain or aching sensation experienced in the neck, shoulder, or arm can vary in intensity and duration. Some individuals may only experience mild discomfort, while others may have severe and persistent pain that affects their ability to perform routine tasks.
In addition to pain, neurogenic Thoracic Outlet Syndrome can also lead to numbness or tingling in the fingers or hand. This sensation, known as paresthesia, can be intermittent or constant, and it may affect one or more fingers. The affected area may feel “asleep” or have a pins-and-needles sensation, making it challenging to perform delicate tasks or handle objects with precision.
Weakening grip strength is another common symptom of neurogenic Thoracic Outlet Syndrome. Individuals may find it difficult to grasp objects firmly or maintain a strong grip, which can impact their ability to perform tasks that require manual dexterity. This symptom can be especially frustrating and limiting for individuals whose work or hobbies involve fine motor skills.
In some cases, neurogenic Thoracic Outlet Syndrome can lead to muscle wasting in the hand. This occurs when the compressed nerves are unable to adequately transmit signals to the muscles, resulting in muscle weakness and atrophy. As a result, individuals may notice a visible decrease in muscle mass, particularly in the affected hand.
Furthermore, neurogenic Thoracic Outlet Syndrome can make it challenging to perform fine motor tasks. Activities that require precise hand movements, such as writing, typing, or playing a musical instrument, may become difficult or impossible due to the pain, numbness, and weakness experienced in the affected arm.
Vascular Thoracic Outlet Syndrome Symptoms
Vascular Thoracic Outlet Syndrome occurs due to blood vessel compression or restriction. This can include venous thoracic outlet syndrome (venous TOS) and arterial thoracic outlet (arterial TOS) syndrome lead to symptoms including:
- Swelling or discoloration of the arm
- Coldness or paleness in the arm or hand
- Weak or absent pulse in the affected arm
- Arm fatigue with use
- Blood clots
- Poor circulation and reduced blood flow
When the blood vessels in the thoracic outlet are compressed or restricted, it can cause a range of symptoms that can significantly impact an individual’s daily life. One of the primary symptoms experienced by individuals with vascular Thoracic Outlet Syndrome is swelling or discoloration of the affected arm. The arm may appear visibly swollen, and the skin may take on a bluish or purplish hue. This swelling and discoloration can be alarming and may cause discomfort or pain.
In addition to swelling and discoloration, individuals with vascular Thoracic Outlet Syndrome may experience coldness or paleness in the affected arm or hand. The restricted blood flow can lead to a decrease in temperature, causing the arm or hand to feel noticeably colder than the rest of the body. The affected area may also appear paler than usual, indicating a lack of proper blood circulation.
Another symptom of vascular Thoracic Outlet Syndrome is a weak or absent pulse in the affected arm. The compression or restriction of the blood vessels can interfere with the normal flow of blood, leading to a weakened or even non-existent pulse. This absence of a pulse can be concerning and may require immediate medical attention to address the underlying cause.
Individuals with vascular Thoracic Outlet Syndrome may also experience arm fatigue with use. Activities that require repetitive or prolonged use of the affected arm, such as carrying heavy objects or performing overhead movements, can lead to increased fatigue and discomfort. This symptom can significantly impact an individual’s ability to engage in physical activities or perform tasks that require arm strength and endurance.
It is important to note that the symptoms of Thoracic Outlet Syndrome can vary from person to person, and some individuals may experience a combination of both neurogenic and vascular symptoms. If you suspect you may have Thoracic Outlet Syndrome, it is essential to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan.[4]
The Impact of Thoracic Outlet Syndrome on Daily Life
Thoracic Outlet Syndrome (TOS) is a condition that affects the nerves and blood vessels in the thoracic outlet, which is the space between the collarbone and the first rib. This syndrome can have a significant impact on a person’s daily life, causing a range of physical and emotional challenges that can be difficult to navigate.
Physical Limitations and Challenges
 Individuals with TOS often experience physical limitations and challenges that can hinder their ability to perform everyday tasks [2]. Simple activities like lifting heavy objects or participating in sports activities may become incredibly difficult or even impossible. The constant pain and discomfort associated with TOS can make it challenging to maintain certain postures for extended periods, leading to a decrease in overall mobility and functionality.
Individuals with TOS often experience physical limitations and challenges that can hinder their ability to perform everyday tasks [2]. Simple activities like lifting heavy objects or participating in sports activities may become incredibly difficult or even impossible. The constant pain and discomfort associated with TOS can make it challenging to maintain certain postures for extended periods, leading to a decrease in overall mobility and functionality.
These physical limitations can have a profound impact on various aspects of life. For example, individuals with TOS may find it challenging to perform their job duties, especially if their work involves manual labor or repetitive movements. Additionally, hobbies and recreational activities that were once enjoyed may need to be modified or avoided altogether due to the potential strain they can put on the affected area.
Emotional and Psychological Effects
The physical limitations and chronic pain associated with TOS can also take a toll on a person’s emotional and psychological well-being. Living with constant pain can be incredibly frustrating and can lead to feelings of helplessness and despair. The inability to engage in activities that were once enjoyed can result in a sense of loss and isolation.
Furthermore, the emotional and psychological effects of TOS can extend beyond frustration and sadness. Chronic pain has been linked to an increased risk of developing anxiety and depression. The constant discomfort and the uncertainty of when or if the pain will subside can create a significant amount of stress and anxiety in individuals with TOS.
It is crucial for individuals with TOS to seek emotional support and coping strategies to manage these effects. This may involve working with a mental health professional who can provide guidance and support in navigating the emotional challenges associated with living with TOS. Additionally, engaging in relaxation techniques, such as meditation or deep breathing exercises, can help reduce stress and promote overall well-being.
In conclusion, Thoracic Outlet Syndrome can have a profound impact on a person’s daily life. The physical limitations and challenges associated with TOS can hinder one’s ability to perform everyday tasks, impacting work, hobbies, and overall quality of life. The emotional and psychological effects of TOS can also be significant, leading to feelings of frustration, anxiety, and even depression. It is essential for individuals with TOS to seek both physical and emotional support to manage the impact of this condition on their daily lives.[5][6]
How is Thoracic Outlet Syndrome Diagnosed
It can be difficult to diagnose Thoracic Outlet Syndrome due to the complex nature of the condition and the variety of potential causes. However, several diagnostic procedures can help healthcare professionals determine the presence of TOS and its underlying cause.
Physical Examination Findings
A physical exam is usually the first step in diagnosing TOS. During the examination, the healthcare provider may check for signs such as loss of sensation, muscle weakness, and changes in pulse and blood pressure in the affected arm. They may also assess the range of motion of the affected shoulder blade and perform specific maneuvers to provoke symptoms.
For example, the healthcare provider may ask the patient to raise their arms overhead and hold that position for a few minutes. This maneuver, known as the “Roos test,” can help determine if the patient experiences symptoms such as pain, numbness, or tingling in the affected arm. Another common maneuver is the “Adson’s test,” where the healthcare provider checks for a decrease in the pulse in the affected arm while the patient rotates their head to the affected side and takes a deep breath.
In addition to the physical examination, the healthcare provider may also inquire about the patient’s medical history, including any previous injuries or trauma to the neck, shoulder, or arm. They may ask about the nature and duration of the symptoms, such as whether they are constant or intermittent, and if they worsen with certain activities or positions.
Imaging and Other Diagnostic Tests
Imaging tests, such as X-rays, CT scans, or MRI scans, can provide detailed images of the thoracic outlet and help identify any structural abnormalities or compression of nerves and blood vessels. X-rays can reveal bony abnormalities, such as cervical ribs or abnormal clavicles, that may contribute to TOS. CT scans and MRI scans can provide more detailed information about the soft tissues, including the muscles, nerves, and blood vessels in the thoracic outlet.
In some cases, the healthcare provider may recommend additional tests to assess nerve function or blood flow in the region. Nerve conduction studies involve the placement of electrodes on the skin to measure the electrical activity of the nerves. These tests can help determine if there is any nerve damage or dysfunction contributing to the symptoms. Angiograms, on the other hand, involve the injection of a contrast dye into the blood vessels to visualize the blood flow and identify any blockages or abnormalities.
Furthermore, the healthcare provider may also consider other conditions that can mimic TOS, such as cervical spine disorders, brachial plexus injuries, or peripheral nerve entrapment syndromes. They may order additional tests, such as electromyography (EMG), to evaluate the electrical activity of the muscles and rule out these alternative diagnoses.
Overall, the diagnostic procedures for Thoracic Outlet Syndrome involve a comprehensive evaluation of the patient’s symptoms, physical examination findings, and imaging or other diagnostic tests. By combining these different approaches, healthcare professionals can accurately diagnose TOS and determine the most appropriate treatment plan for each individual patient.[7][8][9][10][11][12]
How is Thoracic Outlet Syndrome Treated
The treatment of Thoracic Outlet Syndrome aims to relieve symptoms, improve function, and prevent further complications. The specific treatment approach will depend on the underlying cause, severity of symptoms, and individual patient factors.
Non-surgical treatments are often the first line of management for TOS. These treatments aim to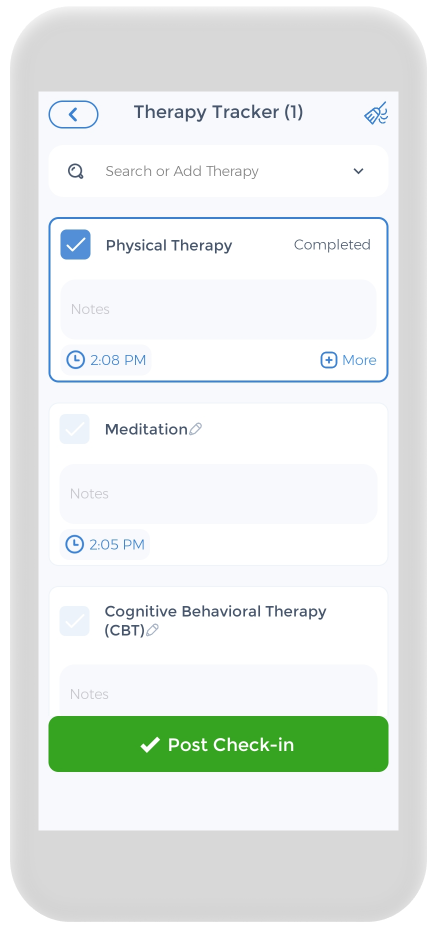 alleviate symptoms and improve the overall function of the affected area. Physical therapists and exercises play a crucial role in the non-surgical treatment of TOS. These exercises focus on improving posture and strengthening the muscles in the neck, shoulder, and upper back. By addressing muscle imbalances and improving posture, physical therapy can help relieve compression on the nerves and blood vessels in the thoracic outlet.
alleviate symptoms and improve the overall function of the affected area. Physical therapists and exercises play a crucial role in the non-surgical treatment of TOS. These exercises focus on improving posture and strengthening the muscles in the neck, shoulder, and upper back. By addressing muscle imbalances and improving posture, physical therapy can help relieve compression on the nerves and blood vessels in the thoracic outlet.
In addition to physical therapy, medications may be prescribed to alleviate pain and reduce inflammation. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to manage pain and inflammation associated with TOS. These medications can help relieve pain, reduce swelling and relieve discomfort.
Ergonomic modifications to the workplace or activities can also be beneficial in managing TOS. Making adjustments to the workstation, such as using an ergonomic chair and positioning the computer monitor at eye level, can help improve posture and reduce strain on the neck and shoulders. Similarly, modifying certain activities that exacerbate symptoms, such as heavy lifting or repetitive overhead movements, can help prevent further compression on the nerves and blood vessels in the thoracic outlet.
Surgical interventions may be considered if conservative treatments fail to provide relief or if there is a clear structural cause of TOS. Surgical procedures aim to relieve compression, remove any anatomical abnormalities or scar tissue, or reposition structures causing irritation. The specific surgical approach will vary depending on the individual case and the underlying cause of TOS.
One surgical option for TOS is called thoracic outlet decompression surgery. This procedure involves removing a portion of the first rib to create more space in the thoracic outlet. By removing the most abnormal first rib, the compression on the nerves and blood vessels can be alleviated, providing relief from symptoms.
In cases where there is an anatomical abnormality, such as a cervical rib or an extra rib, surgical removal of the abnormality may be necessary. This can help eliminate the source of compression and restore normal function to the affected area.
Repositioning structures causing irritation can also be achieved through surgical interventions. For example, if a muscle or tendon is causing compression on the nerves or blood vessels in the thoracic outlet, surgical release or repositioning of the structure may be performed to alleviate symptoms.
Living with Thoracic Outlet Syndrome
Living with Thoracic Outlet Syndrome requires ongoing management and lifestyle adjustments to minimize symptoms and maximize overall well-being. Although TOS can present challenges, there are strategies and resources available to help individuals cope with the condition.
Lifestyle Modifications
Making certain lifestyle modifications can help individuals prevent thoracic outlet syndrome and manage their symptoms more effectively. These may include:
- Adopting good posture and ergonomics
- Performing regular stretching and strengthening exercises
- Managing stress and practicing relaxation techniques
- Avoiding repetitive activities that strain the affected area
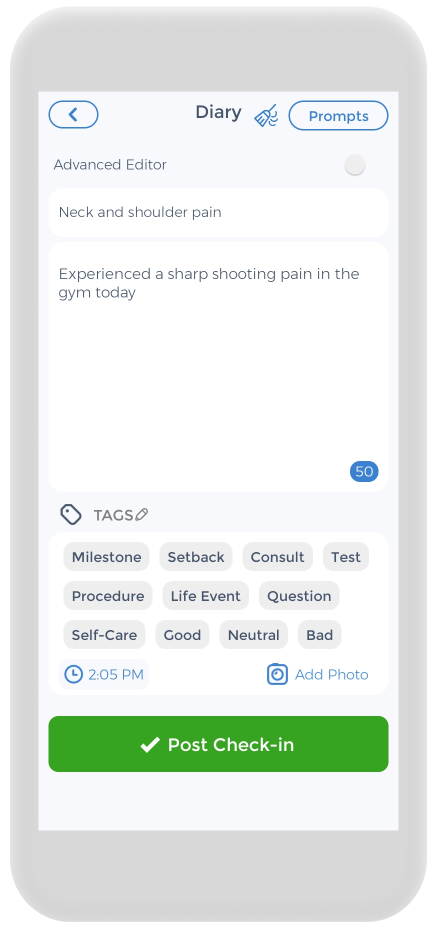
Using the CareClinic App to Manage Pain
Having a pain diary is crucial for your health, and the CareClinic app can help with that. You can use the app as your health and clinical journal. Just go to the pain diary section of the app and enter your daily symptoms, medications, and other triggers, as they occur. There are also specific sections on the app to track each of these. This can help you be aware of early warning signs. Whether you suffer from chronic low back pain, chronic tension headache, impaired physical and mental functioning, chronic headaches, chronic widespread pain, chronic musculoskeletal pain, chronic neck and shoulder pain, or depressive and anxiety disorders, the app is here to help you improve your chronic pain-related health.
The app also has a medication section where you can precisely track the pain therapies you are undergoing, whether it be superficial heat, spinal manipulation, relaxation therapy, or transcutaneous electrical nerve stimulation. Hopefully, having all this information handy will help you with treating chronic pain conditions.
Sources
- https://www.ninds.nih.gov/health-information/disorders/pain
- https://painbc.ca/health-professionals/education/OT-workshop
References
- “Thoracic outlet syndrome”. https://en.wikipedia.org/wiki/Thoracic_outlet_syndrome
- “Thoracic Outlet Syndrome: A Narrative Review – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC7957681/
- “Subclavian artery”. https://en.wikipedia.org/wiki/Subclavian_artery
- “Thoracic Outlet Syndrome | Johns Hopkins Medicine”. https://www.hopkinsmedicine.org/health/conditions-and-diseases/thoracic-outlet-syndrome
- “Evaluation of the socioprofessional consequences of thoracic outlet syndrome – PubMed”. https://pubmed.ncbi.nlm.nih.gov/37697402/
- “Psychosocial Factors in NTOS | SpringerLink”. https://link.springer.com/chapter/10.1007/978-1-4471-4366-6_37
- “Diagnostic and Therapeutic Approach to Thoracic Outlet Syndrome – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC11436167/
- “JAAOS – Journal of the American Academy of Orthopaedic Surgeons”. https://journals.lww.com/jaaos/Fulltext/2015/04000/Thoracic_Outlet_Syndrome.4.aspx
- “Thoracic Outlet Syndrome – TeachMe Orthopedics”. https://teachmeorthopedics.info/thoracic-outlet-syndrome-2/
- “Thoracic outlet syndrome<!– –> – <!– –>Knowledge<!– –> @ AMBOSS”. https://www.amboss.com/us/knowledge/thoracic-outlet-syndrome
- “Diagnosing thoracic outlet syndrome: contribution of provocative tests, ultrasonography, electrophysiology, and helical computed tomography in 48 patients – PubMed”. https://pubmed.ncbi.nlm.nih.gov/11707008/
- “Thoracic Outlet Syndromes | Thoracic Key”. https://thoracickey.com/thoracic-outlet-syndromes/
- “Management — A Guide to Thoracic Outlet Syndrome”. https://www.thoracic-outlet-syndrome.com/treatment
- “Electronic diaries for monitoring chronic pain: 1-year validation study – PubMed”. https://pubmed.ncbi.nlm.nih.gov/11275385/
- “The Use of Symptom Diaries in Outpatient Care | AAFP”. https://www.aafp.org/pubs/fpm/issues/2013/0500/p24.html