Postural Orthostatic Tachycardia Syndrome (POTS) is a condition that affects many individuals around the world. It is characterized by a variety of patient’s symptoms. Including an increased heart rate upon standing, dizziness or lightheaded feeling, migraine headaches, and fatigue.
The exact cause of POTS is still not fully understood. Researchers have begun to explore the potential impact of adrenaline surges on this condition. In this article, we will delve into the connection between adrenaline and POTS. Providing you with a deeper understanding of how these two factors intertwine.[1][2]
Understanding Adrenaline and Its Function
Before we dive into the impact of adrenaline on Postural Orthostatic Tachycardia Syndrome (POTS), let’s first discuss what adrenaline is and its primary function in the body. Adrenaline, also known as epinephrine, is a hormone secreted by the adrenal glands.
It plays a crucial role in the body’s response to stress and danger. When released into the bloodstream, adrenaline triggers a series of physiological changes. Such as increased heart rate, narrowed blood vessels, and heightened alertness.
Specifically, adrenaline prepares the body and immune system for a fight-or-flight response. Allowing us to respond quickly to potential threats. This response can provide an instant boost of energy and mental clarity to avoid brain fog. And it allows us to mobilize our resources and deal with stressful situations effectively.
The Role of Adrenaline in the Body
Adrenaline’s role in the body extends beyond stress response. It also plays a part in regulating various physiological processes. Including heart rate, pulse and blood pressure, and metabolism. Adrenaline acts on specific receptors in the body. Triggering a cascade of events that ultimately lead to the desired response.
For example, when adrenaline binds to beta-adrenergic receptors in the heart, it increases the heart rate and force of contraction. Ensuring that oxygenated blood is pumped to the muscles and organs that need it the most. This mechanism allows us to perform at our best during physically demanding activities or in situations where quick thinking and action are required.
Furthermore, adrenaline also affects blood vessels, causing them to constrict. This constriction redirects blood flow to vital organs, such as the heart and brain. Ensuring that they receive an adequate supply of oxygen and nutrients. At the same time, blood vessels in non-essential areas, like the skin and digestive system, may narrow to prioritize blood flow to more critical areas.
In terms of metabolism, adrenaline stimulates the breakdown of glycogen, a stored form of glucose, into glucose molecules that can be readily used by the body for energy. This process provides an additional source of fuel during times of increased physical activity extreme fatigue, or stress.
While adrenaline is important for our survival, excessive or prolonged adrenaline surges can have detrimental effects on our health. This is where the connection between adrenaline and POTS comes into play.
Postural Orthostatic Tachycardia Syndrome (POTS) Symptoms: Causes and Effects
Adrenaline surges can be caused by a variety of factors. Including physical exertion, emotional stress, anxiety, and certain medical conditions. These surges can lead to an increase in heart rate and blood pressure. Which is a normal response in healthy individuals.
However, in individuals with Postural Orthostatic Tachycardia Syndrome, adrenaline surges may have a more significant impact. Postural Orthostatic Tachycardia Syndrome is characterized by an abnormal increase in heart rate upon standing. Then often accompanied by dizziness and lightheadedness. Adrenaline surges in POTS patients can exacerbate these symptoms. Making it even more challenging for individuals with similar symptoms to engage in daily activities.
When someone with POTS experiences an adrenaline surge, their heart rate can skyrocket, causing a rapid and irregular heartbeat. This can lead to feelings of palpitations, chest pain, abdominal pain, discomfort, and shortness of breath.
Additionally, the constriction of blood vessels caused by adrenaline can worsen symptoms by reducing blood pressure in the brain. Leading to lightheadedness and fainting.
Individuals with POTS need to manage their adrenaline levels to minimize the impact on their daily lives. This may involve lifestyle modifications, such as avoiding triggers that can lead to adrenaline surges, practicing stress-reducing techniques, and working closely with healthcare professionals. To develop a personalized POTS treatment plan.
Adrenaline plays a vital role in our body and nervous system response to stress and danger. While it is essential for our survival, excessive adrenaline surges can have negative effects, particularly for individuals with POTS. Understanding the relationship between adrenaline and POTS can help individuals with this condition better manage their symptoms and improve their quality of life.[3][4][5]
An Overview of Postural Orthostatic Tachycardia Syndrome (POTS)
Before we delve further into the impact of adrenaline on Postural Orthostatic Tachycardia Syndrome (POTS), let’s take a moment to understand the basics of this rare condition first. POTS is a form of dysautonomia, an autonomic disorders that affects the autonomic nervous system. The autonomic nervous system is responsible for controlling various involuntary bodily functions. Such as heart rate, the pulse and blood pressure, and digestion.
POTS, short for Postural Orthostatic Tachycardia Syndrome, is a complex and often debilitating condition that affects millions of people worldwide. It is characterized by an abnormal increase in heart rate upon standing. Leading to symptoms such as dizziness, fatigue, and brain fog. Many individuals with POTS also experience exercise intolerance chronic fatigue syndrome and may have difficulty performing everyday tasks.
Diagnosing Postural Tachycardia Syndrome can be challenging, as the symptoms can overlap with other medical conditions. Healthcare professionals often use a tilt table test to make a definitive diagnosis. This tilt table test is a physical examination that involves lying flat on a table that is then tilted upright while monitoring heart rate and blood pressure. By observing the changes in heart rate and blood pressure during this tilt table test, doctors can determine if POTS is present.
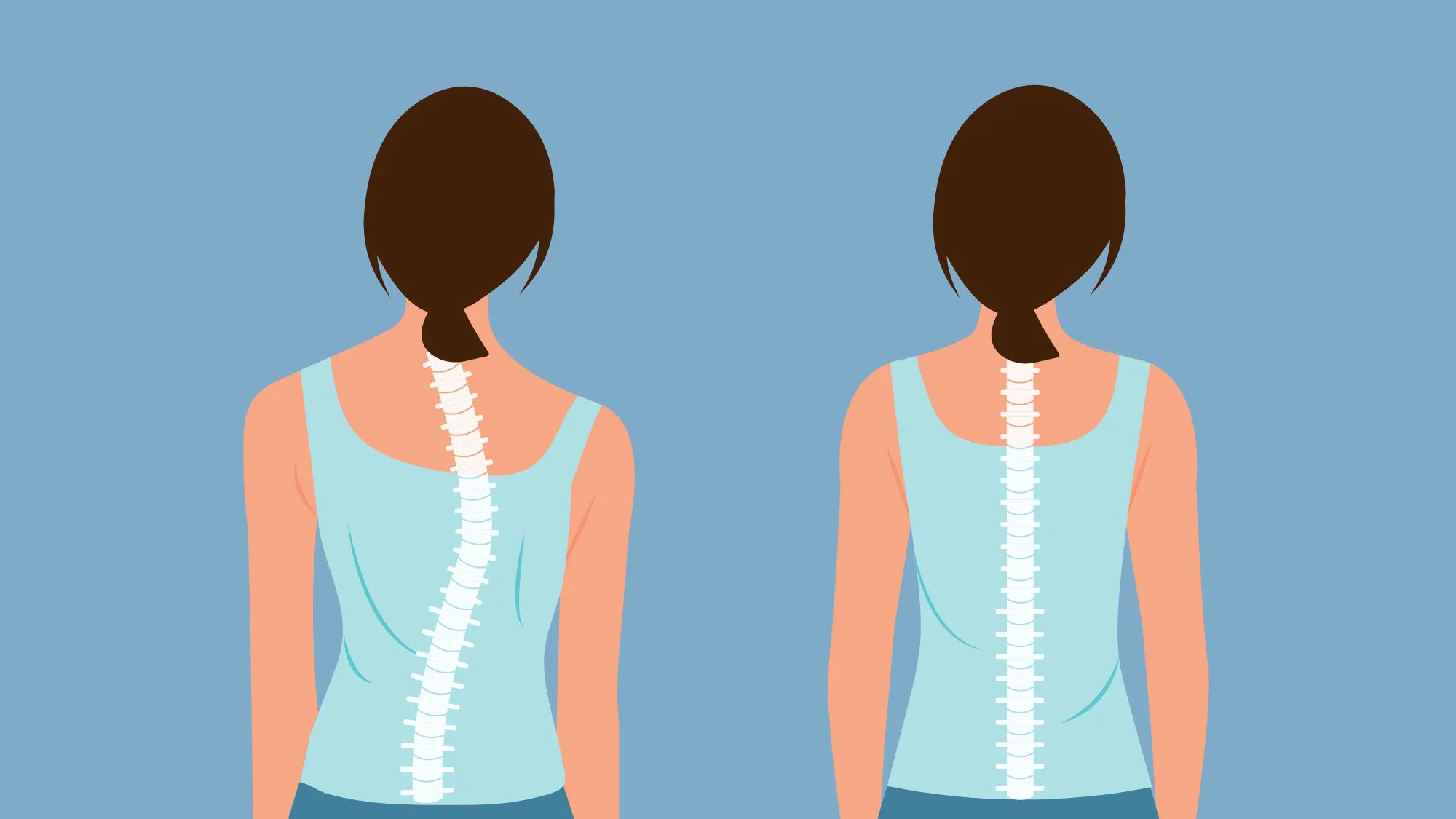
The underlying mechanisms of POTS are still not fully understood. However, researchers believe that it may involve connective tissue abnormalities in the autonomic nervous system and blood flow regulation. Dysfunction in the regulation of blood vessels, along with abnormal adrenaline responses, could contribute to the development of severe POTS.
Theory of Postural Orthostatic Tachycardia Syndrome (POTS)
One theory suggests that Postural Orthostatic Tachycardia Syndrome (POTS) tend to be caused by an imbalance in the autonomic and sympathetic nervous system together. Specifically involving the sympathetic and parasympathetic branches of sympathetic nervous system.
The sympathetic branch is responsible for the “fight or flight” response. While the parasympathetic branch controls the “rest and digest” response. In individuals with POTS, there may be an overactive sympathetic response and an underactive parasympathetic response. Leading to the characteristic symptoms.
Another proposed mechanism is related to low blood volume and blood pressure regulation. It is believed that individuals with POTS may have decreased blood volume. Which can lead to inadequate blood flow to the brain and other vital organs. This reduced blood pressure and flow can trigger the body’s compensatory mechanisms. Such as an increase in heart rate, in an attempt to low blood volume and maintain adequate perfusion.
Furthermore, abnormal adrenaline responses have been observed in individuals with POTS. Adrenaline, also known as epinephrine, is a hormone that plays a crucial role in the body’s response to stress and helps regulate heart rate and blood pressure. In Postural Tachycardia Syndrome, there may be an exaggerated release of adrenaline upon standing. Leading to the rapid increase in heart rate and other symptoms.
While the exact cause of POTS remains elusive, researchers continue to explore various factors that may contribute to develop POTS. Genetic predisposition or family history, viral infection, and hormonal imbalances are among the potential factors being investigated. Understanding the underlying mechanisms are crucial for developing effective POTS treatment and improving the quality of life for individuals living with this condition.[6][7]
The Intersection of Adrenaline and Postural Tachycardia Syndrome
Having explored the nuances of adrenaline and Postural Orthostatic Tachycardia Syndrome (POTS), it is imperative to delve deeper into the intricate interplay between these two factors and how their convergence may heighten the impact on an individual’s daily life.
Individuals with POTS contend with symptoms such as lightheadedness, chronic fatigue syndrome, and a rapid heart rate upon standing, significantly affecting their overall well-being. This syndrome arises from dysregulation in the autonomic nervous system, disrupting the body’s ability to appropriately adjust to changes in posture.
Now, when we overlay same symptoms with the role of adrenaline, a hormone intimately linked to the body’s stress response, the complexity of the scenario becomes apparent.
What is Adrenaline?
Adrenaline, also known as epinephrine, plays a pivotal role in the autonomic dysfunction and “fight or flight” response, triggering physiological changes such as increased heart rate and widened airways. In the context of POTS, a complex illness where the autonomic nervous system is already dysregulated, the presence of adrenaline can potentially exacerbate symptoms.
This is particularly notable when adrenaline is released excessively, as can occur in response to chronic stress or anxiety. The heightened heart rate induced by adrenaline may compound the already rapid heart rate associated with POTS, leading to palpitations, dizziness, and profound fatigue.
The dynamic interaction between adrenaline and POTS creates a feedback loop wherein the symptoms of one condition amplify those of the other, posing significant challenges in the daily lives of affected individuals.
Mundane activities, like standing or engaging in mild physical exertion, become formidable tasks as the compounded effects of adrenaline and POTS make routine actions more strenuous.
This complex interplay underscores the necessity of targeted management strategies that address both the autonomic dysregulation intrinsic to POTS and the potential role of stress-induced adrenaline in exacerbating symptoms.
A nuanced understanding of these intricacies is crucial for healthcare professionals to formulate effective interventions, offering improved support and enhanced quality of life for those navigating the intricate landscape of POTS and adrenaline dysregulation.
How Adrenaline Surges Affect POTS Patients
For individuals with POTS, adrenaline surges can trigger a rapid increase in heart rate, leading to symptoms such as palpitations, dizziness, and shortness of breath. These surges can occur during moments of physical or emotional stress, even in situations that would not typically elicit such a response in healthy individuals.
Imagine a POTS patient preparing for a job interview. The anticipation and nervousness can cause an adrenaline surge, which in turn exacerbates their POTS symptoms. Their heart rate skyrockets, making it difficult to concentrate and present themselves confidently.
This vicious cycle of adrenaline surges, sympathetic nervous system, and POTS symptoms can create a challenging and frustrating experience for individuals.
Furthermore, certain activities that naturally result in an adrenaline surge, such as exercise or even standing up, can be particularly challenging for individuals with POTS. The combination of an already elevated heart rate upon standing and an additional surge of adrenaline can lead to significant discomfort and limited physical functioning.
Take, for example, a POTS patient who loves to participate in high-intensity workouts. While exercise is generally beneficial for overall health, it can be a double-edged sword for someone with POTS. As they engage in vigorous physical activity, their body releases adrenaline to meet the demands of the exercise.
However, this surge of adrenaline can push their heart rate to dangerous levels, causing them to feel lightheaded and fatigued. It becomes a delicate balance between staying active and avoiding triggers that worsen their POTS symptoms.
The Physiological Connection Between Adrenaline and POTS
Researchers are still investigating the precise physiological connection between adrenaline and POTS. One theory suggests that the dysregulation of adrenaline receptors in individuals with POTS may contribute to the heightened response to adrenaline surges.
Additionally, abnormalities in blood pressure, body temperature regulation and the autonomic nervous system could further exacerbate the effects of adrenaline.
Understanding the intricate relationship between adrenaline and POTS is crucial for developing strategies to treat POTS chronic illness and celiac disease. By targeting the underlying mechanisms that drive the exaggerated response to adrenaline, researchers hope to alleviate the burden faced by individuals with POTS.
It is important to note that while adrenaline plays a significant role in the symptoms experienced by POTS patients, it is not the sole factor. POTS is a complex condition significant symptoms are influenced by various physiological and environmental factors. Further research is needed to fully unravel the complexities of this condition and provide individuals with better management options.[8][9]
Potential POTS Treatment and Management Strategies
Although a definitive cure for POTS (Postural Orthostatic Tachycardia Syndrome) remains elusive, individuals diagnosed with this condition can pursue an array of treatment strategies to alleviate symptoms and enhance their overall quality of life.
A multifaceted approach, combining medical interventions with lifestyle adjustments, can be instrumental in managing the challenges significant symptoms posed by POTS.
Medications to Control Adrenaline and Manage POTS
In some cases, medications may be prescribed to help control adrenaline levels and manage symptoms associated with POTS. Beta-blockers, for example, can reduce heart rate and blood pressure, helping to keep blood pressure and alleviate symptoms triggered by adrenaline surges.
Other medications, such as fludrocortisone, may be prescribed to help increase blood volume, improving blood flow regulation.
It is important to note that medication should always be taken under the guidance of a healthcare professional. They will assess psychiatric symptoms, your specific needs and determine the most appropriate medication and dosage for your condition.
Regular check-ups and monitoring will also be necessary to ensure the medication is effectively managing your symptoms.
Lifestyle Changes for Better Adrenaline and POTS Management
In addition to medications, making certain lifestyle changes can also play a significant role in managing adrenaline surges and symptoms of POTS. Here are some self-care strategies you can implement:
Hydration and Electrolyte Balance:
- Ensuring adequate hydration can help maintain blood volume, blood pressure, and reduce the risk of dehydration, which can worsen POTS symptoms. Ensure proper hydration by drinking an adequate amount of water throughout the day. Maintaining electrolyte balance is crucial, so consider incorporating electrolyte-rich drinks or supplements, especially if you experience excessive sweating or dehydration. Drinking enough water throughout the day is essential for individuals with POTS. It is recommended to aim for at least 8 cups of water or fluid intake per day, but this may vary depending on individual needs and activity levels. Additionally, fluid intake of electrolyte-rich beverages, such as sports drinks or coconut water, can help replenish essential minerals lost through excessive sweating.
Avoid triggers:
- Identify any triggers that may exacerbate adrenaline surges and try to minimize exposure to them. This may include reducing stress levels, avoiding extreme temperature changes, and managing emotional triggers. Stress management techniques, such as deep breathing exercises, progressive muscle relaxation, and engaging in hobbies or activities that bring joy and relaxation, can help reduce stress levels. It is also important to create a calm and supportive environment at home and work, minimizing exposure to stressful situations whenever possible.
Gradual Physical Conditioning and Regular Exercise:

- Engage in light to moderate exercise under the guidance of a healthcare professional. Regular exercise can help improve blood flow regulation and strengthen cardiovascular function.
- Engage in a tailored exercise program that focuses on gradual conditioning. Start with low-impact activities like swimming, walking, or stationary cycling, and slowly increase intensity over time. Consult with a healthcare professional or a physical therapist to create a personalized exercise plan.
- Exercise is an important component of managing POTS. However, it is crucial to work with a healthcare professional who specializes in POTS to develop an exercise plan tailored to your individual needs.
- Low-impact exercises, such as walking, swimming, or cycling, are generally recommended. Gradually increasing exercise intensity and duration over time can help improve cardiovascular fitness and reduce symptoms.
Practice stress management techniques:
- Explore stress management techniques such as deep breathing exercises, mindfulness meditation, and yoga. These practices can help reduce panic attack and promote relaxation, potentially mitigating the impact of adrenaline surges.
- Stress management techniques can be beneficial in managing POTS symptoms. Deep breathing exercises, for example, can activate the body’s relaxation response, reducing chest pains, and stress and promoting a sense of calm. Mindfulness meditation and yoga can also help improve mental well-being and provide a sense of control over symptoms.
Frequently monitor symptoms:
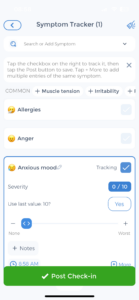
- Keep a journal to track symptoms, triggers, and lifestyle changes. Regularly communicate with your healthcare team to adjust your treatment plan based on your experiences and any changes in symptoms.
- Keeping a symptom diary can provide valuable insights into your condition. By recording your symptoms, their severity, and any potential triggers, you can identify patterns and make informed decisions about your treatment plan.
- This information can also be shared with your healthcare professional, enabling them to make more accurate assessments and adjustments to your management strategies.
Remember, managing POTS is a journey that requires patience and collaboration with healthcare professionals. By implementing a comprehensive self-care plan that includes medications, lifestyle changes, and symptom monitoring, you can take control of your condition and improve your quality of life.
Future Research Directions
Unanswered Questions in the Adrenaline-POTS Connection
While we have made significant progress in understanding the connection between adrenaline and POTS, there are still many unanswered questions. Further research is needed to explore the precise mechanisms by which adrenaline surges impact individuals with POTS and to identify potential targeted treatment strategies.
Additionally, investigating the potential role of lifestyle modifications and self-care practices in managing adrenaline surges in POTS patients could shed new light on effective management strategies.
The Potential of New Therapies and Interventions
As research progresses, new therapies and interventions may emerge that offer novel avenues for managing the impact of adrenaline surges on individuals with POTS.
By staying informed and up-to-date with the latest advancements, individuals with POTS and healthcare professionals can make informed decisions regarding treatment options and develop POTS personalized management plans.
The impact of adrenaline surges on POTS is a complex and multifaceted topic. While adrenaline serves as an important hormone in the body’s response to stress, its dysregulation can significantly impact individuals with POTS.
By understanding this connection and implementing appropriate management strategies, individuals with POTS can take active steps toward improving their quality of life and effectively managing their condition.[10][11]
Use the CareClinic App as a Health Management Tool
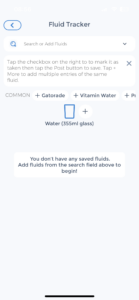
Managing POTS and its associated adrenaline surges can be streamlined with the CareClinic App, a comprehensive health management tool designed to track and analyze your symptoms and treatment efficacy. By utilizing the app’s symptom tracker, you can record the frequency and intensity of adrenaline surges and related symptoms, providing valuable data that can help tailor your treatment plan.
The medication reminder feature ensures you take prescribed medications, like beta blockers, consistently and on time, which is crucial for managing heart rate and blood pressure in POTS patients.
Download the CareClinic App Today
With the CareClinic App, you also gain access to a personalized health diary, allowing you to monitor the effectiveness of lifestyle changes and stress management techniques discussed in this article. By understanding the patterns and triggers of your POTS symptoms, you can work with your primary care physician to adjust your management strategies for better health outcomes.
Take the first step towards improved quality of life by installing the CareClinic App today. Take control of your POTS management journey.[12]
References
- “POTS: Causes, Symptoms, Diagnosis & Treatment”. https://my.clevelandclinic.org/health/diseases/16560-postural-orthostatic-tachycardia-syndrome-pots
- “POTS: Lightheadedness and a racing heart – Harvard Health”. https://www.health.harvard.edu/blog/pots-lightheadedness-and-a-racing-heart-202110012608
- “Adrenaline: Where the hormone is located & what it does”. https://my.clevelandclinic.org/health/body/23038-adrenaline
- “Epinephrine (Adrenaline): What It Is, Function, Deficiency & Side Effects”. https://my.clevelandclinic.org/health/articles/22611-epinephrine-adrenaline
- “Postural orthostatic tachycardia syndrome”. https://en.wikipedia.org/wiki/Postural_orthostatic_tachycardia_syndrome
- “Postural Orthostatic Tachycardia Syndrome (POTS) | Johns Hopkins Medicine”. https://www.hopkinsmedicine.org/health/conditions-and-diseases/postural-orthostatic-tachycardia-syndrome-pots
- “Postural Orthostatic Tachycardia Syndrome – StatPearls – NCBI Bookshelf”. https://www.ncbi.nlm.nih.gov/books/NBK541074/
- “Postural orthostatic tachycardia syndrome: A conundrum for patients and healthcare providers – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC8687482/
- “Postural Tachycardia Syndrome (POTS) | Circulation”. https://www.ahajournals.org/doi/full/10.1161/circulationaha.112.144501
- “Hyperadrenergic Postural Tachycardia Syndrome: Clinical Biomarkers and Response to Guanfacine – PubMed”. https://pubmed.ncbi.nlm.nih.gov/39109428/
- “Exercise and Non-Pharmacological Treatment of POTS – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC6289756/
- “Effectiveness of Mobile Applications on Medication Adherence in Adults with Chronic Diseases: A Systematic Review and Meta-Analysis | Journal of Managed Care & Specialty Pharmacy”. https://www.jmcp.org/doi/10.18553/jmcp.2020.26.4.550


