Crohn’s disease is a chronic, inflammatory disease of the gastrointestinal tract. It is an autoimmune disorder which is when your body’s immune system mistakenly attacks healthy tissue. Crohn’s disease may appear and disappear at various times. Initially, it may affect only a small part of your gastrointestinal tract, but the disease has the potential to progress extensively. Here are Crohn’s disease guidelines and management tips that can help patients cope with and manage their symptoms.[1][2][3]
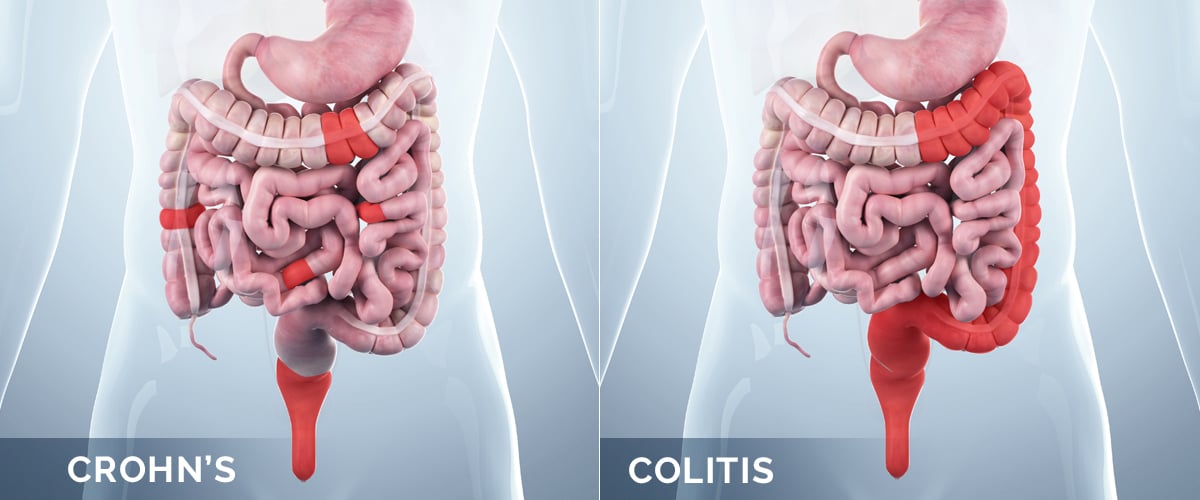
Crohn’s disease and ulcerative colitis
Inflammatory bowel disease (IBD) is a term used to describe two conditions that are characterized by chronic inflammation of the gastrointestinal (GI) tract. These two conditions are Crohn’s disease and ulcerative colitis. Prolonged inflammation results in damage to the GI tract.
Crohn’s disease can affect any part of the GI tract which goes from the mouth to the anus. The disease most often affects the portion of the small intestine before the large intestine or colon. On the other hand, ulcerative colitis usually occurs in the large intestine and rectum.
In Crohn’s disease, damaged tissue areas appear in patches that are next to areas of healthy tissue. Inflammation may also spread through the multiple layers of the walls of the GI tract. In ulcerative colitis, damaged areas are continuous and often start at the rectum and spread further into the colon. Inflammation is also present only in the inner layer of the lining of the colon.
Symptoms of Crohn’s and Colitis can be uncomfortable and damaging, thus it is important to raise Crohn’s disease awareness and ulcerative colitis awareness. Become familiar with their signs and symptoms, and consult your physician if you are experiencing any GI discomfort.
Causes of IBD
The exact cause of IBD is unknown and there are many factors related to the development of IBD. IBD is the result of a defective immune system. An immune system that functions properly normally attacks foreign disease-causing pathogens, such as viruses and bacteria, to protect the body. However, in IBD, the immune system mistakenly responds to environmental triggers, which causes inflammation of the GI tract. If you have a family history of IBD, you are also more likely to develop the disease.
IBD is more common in more developed countries. This suggests that IBD may be related to the modern Western lifestyle and diet. Environmental factors associated with IBD that have been studied include air pollution, certain diets, and taking antibiotics and oral contraceptives.[6][7][8]
Diagnosing Crohn’s disease
Your doctor will likely use a combination of tests to help confirm a diagnosis of Crohn’s disease, including lab tests and various procedures.
- Blood tests. Your doctor may suggest blood tests to check for anemia or signs of infections. Anemia is a condition in which there aren’t enough red blood cells to carry adequate oxygen to your tissues.
- Stool tests can test for hidden (occult) blood or organisms, such as parasites, in your stool.
- Colonoscopy. This test allows your doctor to view your entire colon using a thin, flexible, lighted tube with a camera at the end. During the procedure, your doctor can also take small samples of tissue (biopsy) for laboratory analysis, which may help to make a diagnosis.
- Computerized tomography (CT). This is a special X-ray technique that provides more detail than a standard X-ray does. This test looks at the entire bowel as well as at tissues outside the bowel.
- Magnetic resonance imaging (MRI) uses a magnetic field and radio waves to create detailed images of organs and tissues, including the colon.
- Capsule endoscopy. For this test, you swallow a capsule that has a camera in it. The camera takes pictures of your small intestine and images are checked for signs of Crohn’s disease. The camera exits your body painlessly in your stool. Capsule endoscopy should not be performed if there is a bowel obstruction.
- Balloon-assisted enteroscopy. For this test, a scope is used in conjunction with a device called an overtube. This enables the doctor to look further into the small bowel where standard endoscopes don’t reach.
Crohn’s disease guidelines and treatment options
There is currently no cure for Crohn’s disease, and there is no single treatment that works for everyone. One goal of medical treatment is to reduce the inflammation and relieve symptoms. Another goal of medical treatment is to improve long-term prognosis by limiting complications.
Several medications may be used to treat IBD including aminosalicylates, corticosteroids (such as prednisone), immunomodulators, and biologics. Several vaccinations for patients with IBD are recommended to prevent infections.
The medications used to treat Crohn’s disease are often anti-inflammatory drugs. They include:
- Aminosalicylates. These drugs include sulfasalazine (Azulfidine), which contains sulfa, and mesalamine (Asacol HD, Delzicol, and others). Aminosalicylates have been widely used in the past but now are generally considered of very limited benefit.
- Corticosteroids such as prednisone and budesonide (Entocort EC) can help reduce inflammation in your body, but they don’t work for all patients with Crohn’s disease. Doctors generally use them only if you don’t respond to other treatments. Corticosteroids may be used for a short period of time (three to four months) in order to improve symptoms and induce disease remission. They may also be used in combination with an immune system suppressor.
- Immune response suppressors also reduce inflammation, but they target your immune system, which produces the substances that cause inflammation. For some people, a combination of these drugs works better than one drug alone.
- Biologics are a class of therapies that target proteins made by the immune system.
Severe IBD may require surgery to remove damaged portions of the gastrointestinal tract. Since Crohn’s disease and ulcerative colitis affect different parts of the GI tract, the surgical procedures are different for the two conditions.
Crohn’s disease nutrition therapy and diet
Your doctor may recommend a special diet given by mouth or a feeding tube (enteral nutrition) or nutrients infused into a vein (parenteral nutrition). This can improve your overall nutrition and allow the bowel to rest in order to reduce inflammation. Enteral and parenteral nutrition are often used to get people healthier prior to surgery or when other medications fail to control symptoms.
Your doctor may also recommend a low residue or low-fiber diet to reduce the risk of intestinal blockage. A low residue diet helps to reduce the size and number of your stools.
Here are some general dietary suggestions that may help to manage your condition:
- Limit dairy products. Many people with Crohn’s disease find that related issues such as diarrhea, abdominal pain and gas improve by limiting or eliminating dairy products.
- Drink plenty of fluids daily. Drinking water is best. Alcohol and beverages that contain caffeine stimulate your intestines and can make diarrhea worse, while carbonated drinks frequently produce gas.
- Eat small meals. You may find that you feel better eating five or six small meals a day rather than two or three larger ones. This helps to ease the amount of food that is entering your bowel at a given time.
- Take multivitamins. Because Crohn’s disease can interfere with your ability to absorb nutrients and because your diet may be limited, multivitamins and mineral supplements are often helpful. Check with your doctor before taking any vitamins or supplements.
- Talk to a dietitian. If you begin to lose weight or your diet has become very limited, talk to a registered dietitian.
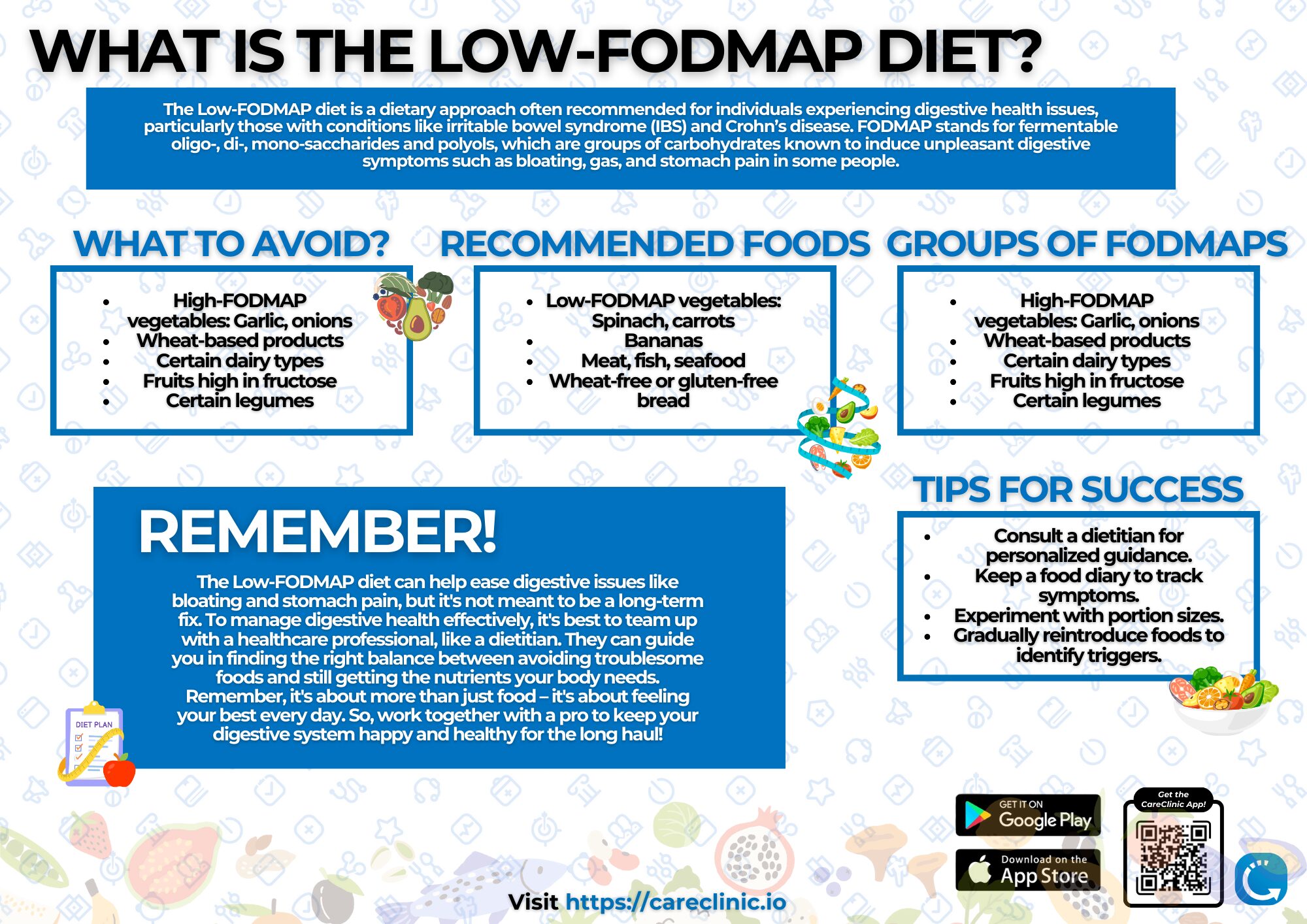
Low-FODMAP diet
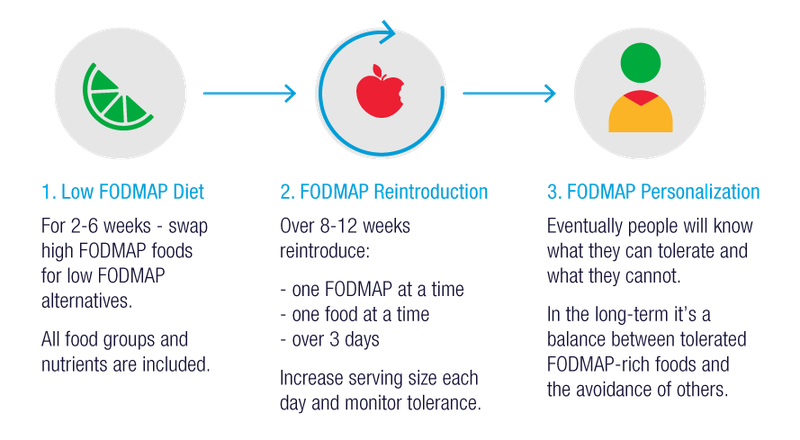
The Low-FODMAP diet is recommended for those who suffer from digestive health issues. These issues include irritable bowel syndrome and Crohn’s disease. Some foods to avoid include garlic, onion, fruits that contain high quantities of fructose, wheat-based products, and certain dairy types. Recommended foods include vegetables, legumes, bananas, meat, fish, seafood, and wheat-free or gluten-free bread.
FODMAP stands for fermentable oligo-, di-, mono-saccharides and polyols. These are groups of carbs that are known to induce unpleasant digestive issues. These symptoms may include bloating, gas and stomach pain.
There are four groups of FODMAPs. The first group is oligosaccharides. This includes wheat, legumes, fruits and vegetables like garlic and onions. The second group is disaccharides and includes dairy products such as milk and cheese. The third group is monosaccharides which include fruits high in fructose such as mangoes, and sweeteners such as honey. The last group is polyols and includes fruits and vegetables like blackberries, as well as low-calorie sweeteners.
Surgical treatment for Crohn’s disease
If lifestyle changes and other treatments don’t relieve your signs and symptoms, your doctor may recommend surgery. Nearly half of those with Crohn’s disease will require at least one surgery. However, surgery does not cure Crohn’s disease.
During surgery, your surgeon removes a damaged portion of your digestive tract and then reconnects the healthy sections. The benefits of surgery for Crohn’s disease are usually temporary as the disease often recurs, frequently near the reconnected tissue. Medications after surgery can minimize the risk of recurrence.[10][11]
Crohn’s disease stress
While stress does not directly cause Crohn’s disease, it can make your signs and symptoms worse and may trigger flare-ups. Stress can affect how quickly food moves through your digestive tract. If food moves too quickly, diarrhea may occur. However, if gastric emptying occurs too slowly, this may result in constipation. Furthermore, stress can induce muscle spasms in the bowel which can be very painful. High stress can also affect which nutrients the intestines absorb. Anxiety and stress can lead to digestive issues, which in turn creates more stress.
When you are anxious, some of the hormones released by your body enter your digestive tract. These chemical messengers can interfere with your digestion and may hurt your gut flora. Your gut flora includes the microorganisms, such as bacteria, that reside in your digestive tract. These bacteria assist with digestion and decrease the body’s production of antibodies. Therefore, it is important to monitor your levels of stress and anxiety, as they can have adverse effects on your digestive health.
Ensure that stress does not negatively affect your gut health. It is important to manage your stress using effective and sustainable methods. This can include going to therapy, utilizing deep breathing, participating in mindfulness activities, or working out. Engage in mindfulness activities and ensure that you contact your healthcare professional if you are having trouble with managing chronic stress.[12][13]
Track your Crohn’s Disease Symptoms
 The CareClinic health app is an effective poop tracker and symptom tracker. It allows you to monitor your daily bowel movements and any pain or inflammation you may be experiencing. You can print the information provided by the application, share it with your physician, seek treatment solutions, and make adjustments to existing medications.
The CareClinic health app is an effective poop tracker and symptom tracker. It allows you to monitor your daily bowel movements and any pain or inflammation you may be experiencing. You can print the information provided by the application, share it with your physician, seek treatment solutions, and make adjustments to existing medications.
CareClinic is an innovative tool for tracking IBS, colitis, or Crohn’s disease. It takes a few minutes to log your bowel movements. Patients can then have easy access to this helpful information about their health.
It is important to record the number of stools in a day. You can add information about each stool regarding its size, color, texture and consistency. It is important to mention whether you felt the urgent need to go to the bathroom. Make sure to take note of any pain or discomfort you experience, including abdominal pain or bloating.
Indicate whether the stool was hard, or soft, or if you experienced any difficulties passing it. You can also add information about your stress levels, water intake and food consumption. All of these factors influence the quality of your stool. Tracking these factors will make it easier to determine what positive lifestyle changes you can pursue.
Why should you track your Crohn’s disease symptoms?
It is possible to suffer from a digestive issue and not be aware of it. Tracking your bowel movements is the most effective way to take charge of your health and discover these issues early on. CareClinic is the best stool tracker app. It can be used to record bowel movements in detail. This is essential for learning about whether you suffer from various medical conditions.
Tracking your bowel movements every day makes determining stool irregularities and finding patterns in your bowel movements very easy. You can identify habits that affect your bowel movements, such as having a low-fiber diet or not drinking enough water. After identifying these habits, one is then able to effectively eliminate such lifestyle choices.
If you have already been diagnosed with a chronic bowel condition, you might also consider tracking your bowel movements. The poop log will help you monitor the frequency and severity of your symptoms. It can also be used to assess the progress you have made with certain treatments.
Using CareClinic to stick to Crohn’s disease guidelines
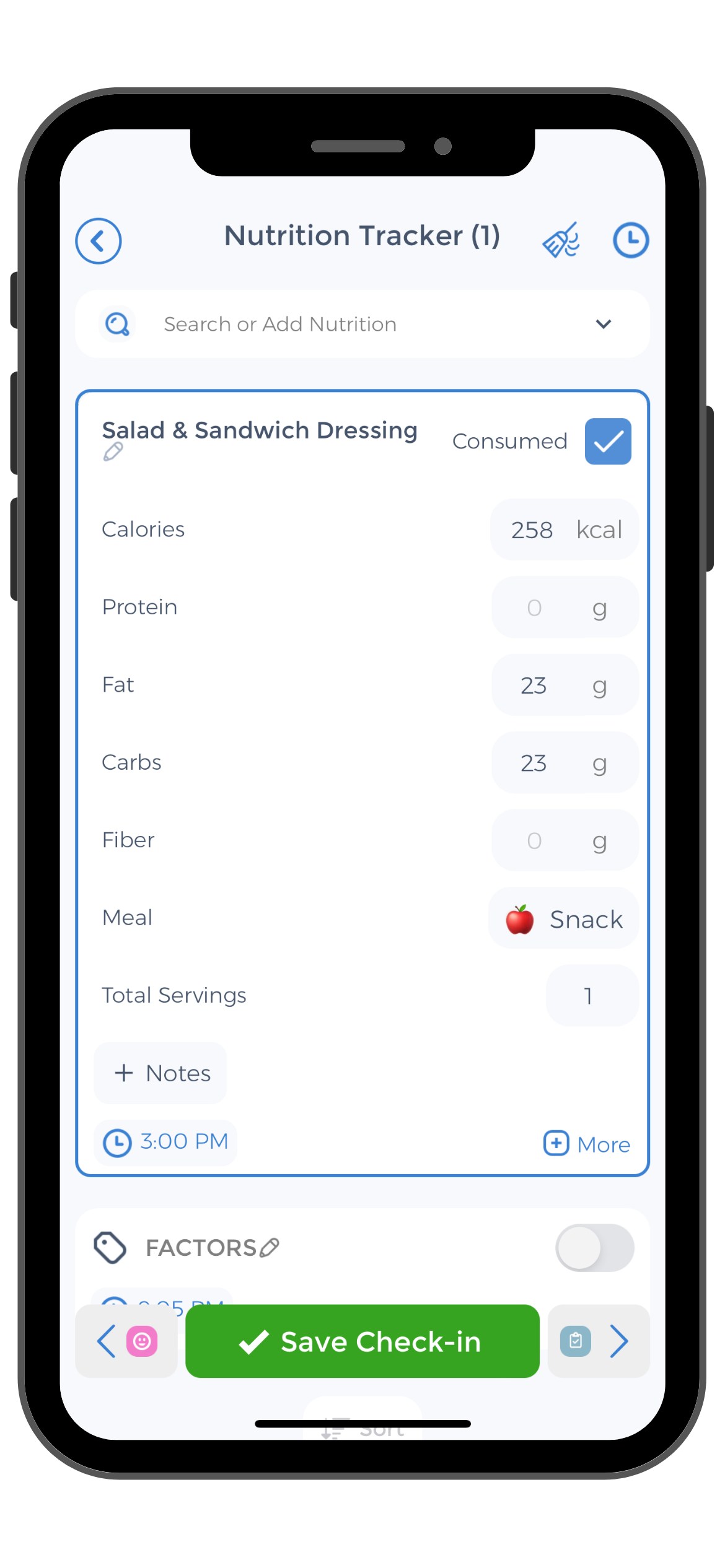 We make choices every day to ensure that our diets are rich in gut-friendly food. Use the CareClinic health app to track your meals and the reactions you had to them. This can help identify foods that you might not be able to digest very well.
We make choices every day to ensure that our diets are rich in gut-friendly food. Use the CareClinic health app to track your meals and the reactions you had to them. This can help identify foods that you might not be able to digest very well.
Once you have eliminated foods you cannot tolerate, the improvements in the quality and frequency of your stools will become evident. Planning your meals on a weekly basis, opting for a personalized diet, and experimenting with different ingredients are great ways to improve gut health.
Clinicians often recommend a diet low in FODMAP foods to patients with irritable bowel syndrome and Crohn’s disease. If you are experiencing such symptoms, it is important to talk to your healthcare provider in order to identify any necessary dietary changes.
The CareClinic app can help ease the transition into following a low-FODMAP diet. Patients are able to track their daily food consumption. This is essential for ensuring that they are obtaining the necessary nutrients. Caregivers and patients can work together to develop nutrition plans using the app. Patients are then able to access their nutrition plan at any time on their devices. This ensures that they are sticking to their new diet plans and necessary Crohn’s disease guidelines for nutrition.
Monitor and stick to Crohn’s disease guidelines
Take steps for Crohn’s and Colitis by downloading CareClinic, a free health app that can be downloaded on Android and iOS. It can draw information from other applications such as Apple Health and vice versa. The app serves as an easy-to-use stool log. It provides beneficial information for those experiencing bowel issues and seeking potential treatment routes. The app assists individuals with developing personalized nutrition plans and ensures that users stick to their diet plans. It is a useful urination and stool tracker that empowers users to take charge of their own health on a daily basis.
Use CareClinic to monitor your stool habits. This can help with identifying any adverse digestive symptoms which may be indicative of underlying health problems. This stool tracker app also allows you to easily contact your caregivers to receive up-to-date information about what next steps to take after identifying abnormalities in your bowel movements. Also use the CareClinic app to track your Crohn’s disease symptoms, including pain, inflammation and bowel movements. CareClinic is an innovative tool for identifying conditions like colitis or Crohn’s disease. CareClinic can help you stick to your Crohn’s disease guidelines and treatment plan recommended by your healthcare team. Install the app today.[14]
References Crohn’s disease can cause symptoms beyond just bowel issues. Some people also get crohn’s mouth sores that can make eating uncomfortable. Tracking all your symptoms together helps you see the full picture of how Crohn’s affects your daily life.
- “Crohn’s Disease Self-Care: Strategies and Tips”. https://www.health.com/crohns-disease-self-care-7965532
- “Official journal of the American College of Gastroenterology | ACG”. https://journals.lww.com/ajg/fulltext/2017/02000/acg_clinical_guideline__preventive_care_in.15.aspx
- “14 Self-Care Tips for Crohn's Disease”. https://resources.healthgrades.com/right-care/crohns-disease/crohns-disease-self-care
- “Crohn's Disease vs Ulcerative Colitis: What's the Difference? | Blog | Loyola Medicine”. https://www.loyolamedicine.org/newsroom/blog-articles/crohns-disease-vs-ulcerative-colitis-whats-difference
- “Differences Between Crohn's Disease and Ulcerative… | GI Associates”. https://gi.md/resources/articles/differences-between-crohns-disease-and-ulcerative-colitis
- “What Causes IBD | IBD | CDC”. https://www.cdc.gov/inflammatory-bowel-disease/causes/index.html
- “Evaluating the influence of environmental risk factors on inflammatory bowel diseases: a case-control study – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC10520386/
- “Environmental risk factors for inflammatory bowel disease – Singh – 2022 – United European Gastroenterology Journal – Wiley Online Library”. https://onlinelibrary.wiley.com/doi/10.1002/ueg2.12319
- “Diagnosis of Crohn’s Disease – NIDDK”. https://www.niddk.nih.gov/health-information/digestive-diseases/crohns-disease/diagnosis/
- “Inflammatory Bowel Disease Guidelines: Guidelines Summary, British Society of Gastroenterology Guidelines (BSG) (2019), European Crohn's and Colitis Organisation Guidelines on Medical Treatment (ECCO) (2019)”. https://emedicine.medscape.com/article/179037-guidelines
- “Special IBD Diets | Crohn's & Colitis Foundation”. https://www.crohnscolitisfoundation.org/patientandcaregivers/diet-and-nutrition/special-ibd-diets
- “Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options – PubMed”. https://pubmed.ncbi.nlm.nih.gov/22314561/
- “Coping Strategies to Improve Mental Health | Crohn's & Colitis Foundation”. https://www.crohnscolitisfoundation.org/patientsandcaregivers/mental-health/coping-strategies-for-better-mental-health
- “Journal of Medical Internet Research – Mobile Apps for the Management of Gastrointestinal Diseases: Systematic Search and Evaluation Within App Stores”. https://jmir.org/2022/10/e37497