acti
Activities of daily living (ADLs) are basic tasks we perform each day without much thought. These include eating, bathing, dressing, toileting, and transferring (moving from one position to another). Instrumental activities of daily living (IADLs) are more complex and involve tasks like cooking, cleaning, doing laundry, and managing money. IADLs typically require the use of tools or equipment to complete. You can download the Activities of Daily Living Worksheet below. But first, we’ll explain which type of tracking you may need and how to record ADL and IADL values accurately.
Table of Contents
- Why log ADLs and IADLs?
- Who Should Use an ADL Worksheet?
- How to Use the ADL Worksheet
- Printable Activities of Daily Living Worksheet PDF
- Track ADLs Using the CareClinic App
- When Should You Use an ADL Log?
- ADL and IADL Rating Scales Explained
- Choosing the Right ADL Scale
- Do Activities of Daily Living Worksheets Actually Help?
- Start Logging Your ADLs Today (PDF or App)
Why log ADLs and IADLs?
There are many reasons why you might want to keep track of your ADLs and IADLs. For example, if you are an older adult, tracking your activities can help you or your doctor spot early signs of functional decline. This information can then be used to make changes in your life that may help prevent further decline.
In addition, tracking your activities can help you to see how your abilities have changed over time. This information can be useful in making decisions about your care or treatment. For example, if you are considering surgery, you may want to know how well you have been able to perform activities since your last operation.
Who Should Use an ADL Worksheet?
Anyone can track their ADLs and IADLs. However, this method may be beneficial for older adults or people with chronic health conditions.
How to Use the ADL Worksheet
You can track ADLs using either a printable worksheet or a smartphone app. Just record which activities you did each day and rate how easy or difficult they were. The key is consistency. Tracking regularly helps you spot changes early.
7 ADL’s
The six daily living activities are:
- Bathing
- Dressing
- Toileting
- Transferring
- Continence
- Feeding
- Grooming
These activities are important for people to be able to do on their own. If a person is unable to do one or more of these activities, they may need help from others.
Printable Activities of Daily Living Worksheet PDF
If you would prefer to use a paper form, you can download and print a PDF version of the ADL tracking worksheet.
Instructions:
- Choose which activities you want to track. You can track as many or as few activities as you like.
- For each activity, rate how well you were able to do it on a scale of 1-5, with 1 being “very difficult” and 5 being “very easy.”
- Optional: If you want, you can also add any comments about the activity.
- Repeat this process for each day that you want to track.
- After a week or two, take a look at your log. Are there any activities that you are having difficulty with? Are there any trends that you see?
- If you are concerned about your ability to perform activities, talk to a doctor or other healthcare professional. They can assess the situation and provide guidance on how to best proceed.
Sample ADL Log
Day 1
Activity, Rating, Comments
Washing face, 5
Brushing teeth, 5
Showering, 5
Dressing, 5
Using the toilet, 5
Eating, 5, low appetite
You can record this and more in the Activities of Daily Living Worksheet Printable PDF below:
Download Your Free ADL Worksheet (PDF)
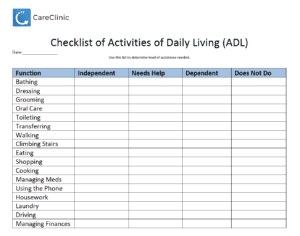
Download Activities of Daily Living Worksheet
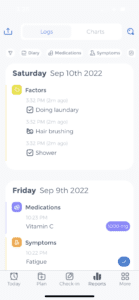
Track ADLs Using the CareClinic App
Logging activities of daily living (ADLs) and instrumental activities of daily living (IADLs) in CareClinic is easy! Just follow these simple steps:
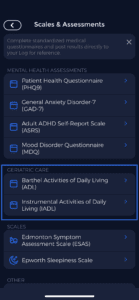
- Open the app and tap on the “…” More text at the bottom of the screen in the navigation
- Tap on “Health Assessments.”
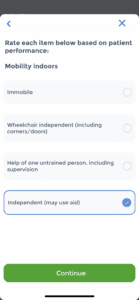
- Tap on “Activities of Daily Living ADL” or & “IADLs”
- On the next screen, you may begin the assessment and get your score.
You can see how this process looks in the app (in dark mode) and in regular mode below:
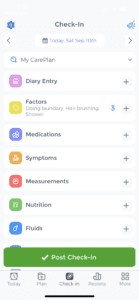
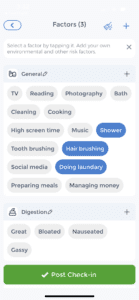
You may also begin to log your data using the “Factors” Tracker, along with other Trackers, to save more details for you to review later. Here is an example of how entries would look if Trackers were used.
When Should You Use an ADL Log?
ADL and IADL tracking is most useful for people with dementia, Parkinson’s, stroke, or any condition that affects daily independence. These logs help spot decline early and guide care decisions.
ADL and IADL Rating Scales Explained
Katz ADL scale
Clinicians use the Katz ADL scale to measure functional decline in individuals. The scale includes six core activities: bathing, dressing, toileting, transferring, continence, and feeding. Evaluators assign a score from 0 to 4 for each activity, where 0 means the person cannot perform the task at all, and 4 means the person completes it independently without difficulty.
If a person scores between 0 and 2 on any individual item, it shows they rely on others to perform that activity. A consistent score of 3 or 4 across all six activities indicates the person maintains full independence in daily living.
Healthcare providers track changes using the Katz ADL scale to monitor functional decline over time. They also apply the scale to compare functional ability across individuals or populations. For example, researchers may use it to examine differences between older adults with dementia and those without cognitive impairment.
Barthel ADL index
Clinicians use the Barthel ADL index to assess functional decline in individuals. The index includes 10 daily activities: feeding, grooming, bathing, dressing, transferring, toileting, ambulation, stair climbing, bladder control, and bowel control. Each activity receives a score ranging from 0 to 20, where 0 means the person cannot perform the task at all, and 20 means the person performs it independently without difficulty.
If a person scores between 0 and 59, it indicates dependence on others for daily activities. A total score between 60 and 100 reflects full independence across all assessed functions.
Healthcare professionals track changes in ability over time using the Barthel ADL index. They also use the tool to compare functional capacity across individuals or population groups. For example, they may compare the daily functioning of older adults with a history of stroke to those without neurological impairments.
The Lawton IADL scale
Clinicians use the Lawton IADL scale to evaluate functional decline related to independent living. The scale covers eight instrumental activities: using the phone, shopping, preparing meals, doing housework, taking medications, handling money, using transportation, and getting out of bed. Each item receives a score from 0 to 4, where 0 means the person cannot perform the task, and 4 means they complete it independently without difficulty.
If a person scores between 0 and 2 on any item, it indicates reliance on others for that activity. A consistent score of 3 or 4 across all eight areas reflects full independence in instrumental daily living.
Healthcare providers track functional changes over time using the Lawton IADL scale. They also use the tool to compare functional abilities across individuals or groups. For example, researchers may use it to examine differences in independent living skills between older adults with dementia and those without cognitive decline.
Functional Independence Measure
The functional independence measure (FIM) is a tool that can be used to measure functional decline. It consists of 18 items: self-care, sphincter control, transferring, locomotion, communication, and social cognition. Each item is rated on a scale from 1 to 7, with 1 being unable to perform the activity and 7 being able to perform it without any difficulty.
A score of 1–2 on any item indicates that the person is dependent on others for that activity. A score of 3–7 on all items indicates that the person is independent in all activities.
The FIM can be used to track functional decline over time. It can also be used to compare different people or groups of people. For example, the scale can be used to compare the functional abilities of older adults with and without stroke.
Rehabilitation outcome measure
The rehabilitation outcome measure (ROM) is a tool that can be used to measure functional decline. It consists of nine items: daily living activities, mobility, self-care, employment, recreation and leisure, education, social function, family function, and community function. Each item is rated on a scale from 0 to 6, with 0 being unable to perform the activity and 6 being able to perform it without any difficulty.
A score of 0–3 on any item indicates that the person is dependent on others for that activity. A score of 4–6 on all items indicates that the person is independent in all activities.
The ROM can be used to track functional decline over time. It can also be used to compare different people or groups of people. For example, the scale can be used to compare the functional abilities of older adults with and without stroke.
Functional assessment measure
The functional assessment measure (FAM) tracks functional decline across 10 areas: daily living activities, mobility, self-care, employment, recreation and leisure, education, social function, family function, community function, and global function. Each item is scored from 0 to 6, where 0 means the person cannot perform the activity and 6 means they can complete it without difficulty.
Scores of 0 – 3 suggest dependence on others, while consistent scores of 4–6 indicate full independence.
Clinicians use the FAM to monitor changes over time and compare functional abilities across individuals or groups, such as older adults with and without a history of stroke.
Performance-oriented mobility assessment
The performance-oriented mobility assessment (POMA) measures functional decline based on six items: standing, walking, stair climbing, transfers, arm movements, and leg movements. Each item receives a score from 0 to 4, where 0 means the person cannot perform the task and 4 means they can do it without difficulty.
People who score 0–2 on any item typically depend on others. A consistent score of 3–4 indicates full independence. Clinicians use the POMA to track changes over time and compare functional ability across individuals or groups, such as older adults with or without a history of stroke.
Bristol Activities of Daily Living Scale
The Bristol Activities of Daily Living Scale measures functional decline across six items: bathing, dressing, toileting, transferring, continence, and feeding. Each item receives a score from 0 to 4, where 0 means the person cannot perform the activity and 4 means they can complete it independently.
Scores of 0 – 2 on any item suggest dependence, while consistent scores of 3–4 indicate full independence.
Clinicians use the Bristol Scale to track changes over time and compare functional abilities between individuals or groups, such as older adults with or without a history of stroke.
Choosing the Right ADL Scale
The best scale for you will depend on your needs and preferences. Some factors to consider include:
- How often do you want to track your activities
- How much time do you have to devote to tracking
- Whether you want to track your activities yourself or have someone else do it for you
Once you have considered these factors, you can choose the scale that best suits your needs. For example, the Bristol Activities of Daily Living Scale, if you want to track your activities over time, or the Lawton scale if you need a more detailed assessment.
How long does it take to record ADLs?
The amount of time it takes to track your ADLs and IADLs will depend on the method you choose. A daily log can take just a few minutes each day. However, a home health assessment may take an hour or more.
Who records it?
You can track your ADLs and IADLs yourself, or you can have someone else do it for you. If you are tracking your own activities, it is important to be consistent in how you record them. This will make it easier to spot trends over time.
If you have someone else track your activities, they will need to be familiar with the method you are using. For example, if you are using a smartphone app, they will need to know how to use the app and how to enter the data.
How Often Should You Log ADLs?
The frequency of tracking will depend on the purpose of the tracking. For example, if you are tracking your activities to spot trends over time, you may want to do it daily or weekly. If you are tracking your activities for a home health assessment, you may only need to do it once.
Do Activities of Daily Living Worksheets Actually Help?
There is limited evidence on the use of ADL and IADL tracking. However, one study found that tracking functional decline can be useful in predicting the need for long-term care. Another study found that tracking functional decline can help identify people at risk for falls. This is important because falls are a leading cause of injury in older adults.
Are Activities of Daily Living Worksheets used in nursing homes and communities?
Care teams track ADLs and IADLs in both nursing homes and community settings. In nursing homes, staff use them to assess long-term care needs. In the community, providers use them to identify people at risk for falls.
What if you can’t do an activity?
If you are unable to do an activity, you can ask for help from another person or use adaptive equipment. For example, if you are unable to dress yourself, you can ask someone else to help you or use adaptive clothing.
Start Logging Your ADLs Today (PDF or App)
Using an activities of daily living worksheet helps you track progress, spot areas where you need support, and plan for long-term care. Print the free Activities of Daily Living worksheet file above whenever you want to record values for yourself or a dependent. Or use the CareClinic app on iOS or Android to log everything digitally without printing. Either way, start today.