CRPS stands for complex regional pain syndrome. It is a progressive condition where you feel a sudden or constant pain in an area of your body. Since complex regional pain syndrome is progressive, it can also be considered a chronic condition. Sensory, vasomotor, edema or sudomotor, motor or trophic, are characteristic of CRPS symptoms. CRPS is a rare condition. Patients who have had a recent surgery or injury trauma may suffer from this condition. These patients would fall under type 2 CRPS. Type 1 CRPS refers to a not-so-obvious nerve disorder that stems from an unidentified nerve damage. Type 1 CRPS contains three stages. The CRPS stages are: acute, subacute, and chronic. We will discuss these a bit more below.
What causes complex regional pain syndrome? The main cause linked to CRPS is nerve damage and trauma injury. According to a study conducted by Stephen Bruehl, approximately 7% of patients who have suffered a limb injury, or related surgery have experienced acute CRPS (R). CRPS can occur in more than one area of the body. However, minor injuries such as bone fractures occur in the arms and legs. Therefore CRPS affects these areas more commonly.
History of CRPS
Doctor Denmark, a British surgeon in the Royal Navy Hospital recorded the first evidence of CRPS in 1812. Doctor Denmark had treated a gunshot wound, that had healed. However, he had noticed that when he saw the soldier, his forearm was twisted. The solider described a burning pain and was sweating. The doctor concluded that this continuous and burning pain was coming from the radial nerve in the upper arm. The same area where the soldier had a gunshot injury.
Silas Weir Mitchell, a doctor during the American Civil War, took note of the nerve injuries the soldiers suffered as a result of gunshot wounds. In 1864, along with George Morehouse and William Keen, they published the report titled “Gunshot Wounds and Other Injuries”. During the war, physicians would use this to identify and treat nerve damage in soldiers. He linked burning pain and changes in skin temperature and texture to the site of nerve damage.
In the 1900s, quite a few doctors had concluded similar symptoms linked to nerve damage. Either caused by a known injury trauma or by an unknown source or nerve damage. I’m certain you did not come here for a history lesson so I will skip ahead to the naming of CRPS. In 1993, after a criterion was developed in the diagnosis of reflux sympathetic dystrophy, John Bonica proposed the name change to complex regional pain syndrome. His reasoning being that this condition was not limited to the nerve or root, but rather to the diverse distribution of the symptoms (R).
So now that we understand some of the origins of complex regional pain syndrome, let’s dive further into the varying types of CRPS.
CRPS types
The first type of CRPS was formally known as reflux sympathetic dystrophy (RSD). Type 1 CRPS occurs when an individual has suffered a minor but apparent injury, with no evident nerve damage. The individual will experience this around the arms and legs area of the body. Associated with this type are three stages: acute, subacute and chronic.
Type 1 CRPS stages
The acute stage refers to a temporary burning pain or sensation in the area of injury. This does not last more than 3 months after the injury. If the patient experiences swelling and redness, this is an indication that attention needs to be brought to the area and should be treated. By diagnosing the patient in this CRPS stage, symptoms can be reversed and prevented from progressing further. If not, the individual will progress to the subacute CRPS stage.
In the subacute stage, the individual will feel severe and constant burning pain, redness and difficulty in motility in the area of pain. This will last up to 9 months. By diagnosing the patient in this CRPS stage, symptoms can be limited and treated to prevent further harm. If not treated, then the individual will progress to the chronic CRPS stage.
In the chronic stage, the pain will no longer be as manageable. It may continue for many years or become permanent. In this persistent stage it will limit the individual’s ability to perform daily tasks. There will be stiffness in the area, and it will be cold, dry and pale in appearance.
Type 2
Formally known as causalgia, Type 2 CRPS is the widely used term at present. Type 2 CRPS occurs when an individual has suffered a major injury, including bone fracture or has had a surgery. Heart attacks and infection can also lead to the development complex regional pain syndrome. In this type of CRPS the injury or source of nerve damage is clearly apparent.
The nerve damage site may be obvious or not, CRPS has the potential to spread through the body. It is commonly found to affect the arms and legs. That being said, there are cases where CRPS has affected other areas of the body. For example, CRPS has been found to affect some individual’s teeth and gums.
Potential Symptoms
This condition is most commonly diagnosed in individuals aged between 40-60. Although it is usually found in women and can affect children. However, it can still affect younger adults and men. Therefore, it is important to be aware of the symptoms to help diagnose it earlier rather than later on.
Like most conditions, if recognized early on and treated appropriately, CRPS can be reduced and restricted from causing further strain to the body. If you experience these symptoms, following an injury or surgery, it may be in your best interest to consult a trusted physician. While pain is often the most common symptom, there are other symptoms that need to be present. By identifying the symptoms you will be able to identify CRPS. The symptoms include:
- Burning or stinging sensation that is persistent
- You experience changes in skin temperature; especially if the area is becoming colder or you experience sweating
- There is fluid retention around the area or swelling (edema)
- Skin discoloration, including blotching skin, pale, blueish or red coloring, shiny and tender texture
- Stiff muscle joints, hard to move or painful to move
- Tremors or muscle spasms
- Fainting, frozen shoulder
- Area is touch sensitive (hyperalgesia), or allodynia (experiencing pain from a stimulus that is not commonly painful)
- Changes in hair and nail growth pattern
If you have a systematic disease such as arthritis, psoriasis or diabetes, be vigilant in monitoring these symptoms after you have had a surgery or experience an injury.
Phantom Pain
Phantom pain refers to pain sensation felt in a limb that is no longer there. It can often be mild pain. The pain sensation gets weaker over time and is not as frequent. This is common in individuals who have had surgery to remove a limb. Doctors believed that phantom pain was a psychological condition. However, we have made the link to nerve sensations connected to the spinal cord and brain. Medical testing cis not used to diagnose phantom pain and CRPS. The main difference between CRPS and phantom pain is related to the source of damage. The pain felt from CRPS is from localized nerve damage. The pain felt from phantom pain is through a connection between the spinal cord and brain.
Phantom pain and complex regional pain syndrome can often be confused with one another. Being attentive to your body signals can help you become self-aware of your condition. We will discuss more on how to manage your symptoms and pain later on. To learn more in-depth tips, feel free to read up on this article. Every individual experiences pain differently. Try to focus on your symptoms and educate yourself about the condition. Always consult a trusted and licensed physician or specialist. Although there is much left to learn, there are ways that have successfully identified and limited the pain.
The “Budapest Criteria”
Due to the rarity of this disease, how would your physician know to diagnose you? Well, that is where the Budapest Criteria comes into play. There must be persistent pain following the event of trauma, injury or surgery recovery time. There must be at least three symptoms and one physical sign present at the time of diagnosis that fall under the four categories: sensory, vasomotor, edema or sudomotor, motor or trophic. Sensory referring to physical sensitivity (hyperaesthesia) or allodynia. Vasomotor means skin discoloration or sudden increase or decrease in skin temperature. Edema meaning sweating or swelling in the area. Motor or trophic meaning motility troubles, changes in hair and/or nail growth (R).
The final criteria of the Budapest Criteria states that the cause of these listed symptoms cannot be linked to an alternative diagnosis. Medical testing such as MRI or bone scans may be conducted to ensure that these symptoms are not caused by an alternative condition. As a result, to support CRPS, there is no testing that can be conducted. There is currently no other diagnosis that exists to better explain these symptoms.
Aside from medication there are other ways to treat CRPS, depending on the CRPS stage or type you categorize under. It is best to consult a trusted physician to locate a pain specialist to help you out.
“Prevention is better than cure” – Desiderius Erasmus
We have all heard this famous quote by the Dutch philosopher, “Prevention is better than cure”. Why is prevention better? We are learning and discovering many conditions that affect our health. There are diseases that do not have a cure. The diseases with a cure still need time. During this time the body focuses on healing repairing the damage. Either way, by tracking symptoms, especially related to CRPS stages can help your physician diagnosis and prevent further complications.
Possible Treatments
Invasive treatments can help to improve this condition, but there is still a lack of clinical trials to support this. Treatments include spinal cord stimulator (SCS) and trigger point injections (TPI). What exactly do these treatments entail? Let’s start with what a spinal cord stimulator is. A SCS is a surgically placed device found in the spinal cord. It sends minor electrical currents to the nerves. This will stimulate the nerve and help to ease the pain. A trigger point injection contains a pain relief medication such as lidocaine, bupivacaine or corticosteroid that is injected into the area of pain. This procedure can create relief or ease the pain for approximately six months.
Rehab
Physical rehabilitation can help to desensitize the joints. Gentle and small movements can prevent muscle and joint stiffness. Avoid vigorous exercise and focus on just trying to activate movement in the area. If you experience pain and severe discomfort, then let the physician know and stop.
Psychotherapy
Psychotherapy is another form of treatment that can help mentally prepare you for handling your pain. It can help you to better understand your condition. You can decipher and learn about your condition, which can help you manage your thoughts and actions.
Talk to Your Doctor
Consulting a physician and specialist is always a good resource in managing CRPS. Learn as much about your symptoms as you can. If you are self-aware about the pain triggers, you will be able to determine the best prevention and treatment type.
Treatment results varies among individuals. Some people may be able to reverse the symptoms, while others may experience persistence. Some may be able to tolerate the pain, while others will not. Regardless, do not be discouraged. Be attentive in monitoring symptoms, especially after a surgery. Monitor the area of injury, and keep in mind the triggers. There are many ways to track your personal triggers. Technology and applications are one of the quickest and trending form of symptom tracking.
The Use of Technology
 Some may find it to be difficult to track and monitor potential symptoms. Health apps have always been a trending topic, but it can be hard to find one designated for your needs. Check out this article on the care clinic website for chronic care management and health apps. There are many positive benefits to using an application to help monitor you pain level and health condition.
Some may find it to be difficult to track and monitor potential symptoms. Health apps have always been a trending topic, but it can be hard to find one designated for your needs. Check out this article on the care clinic website for chronic care management and health apps. There are many positive benefits to using an application to help monitor you pain level and health condition.
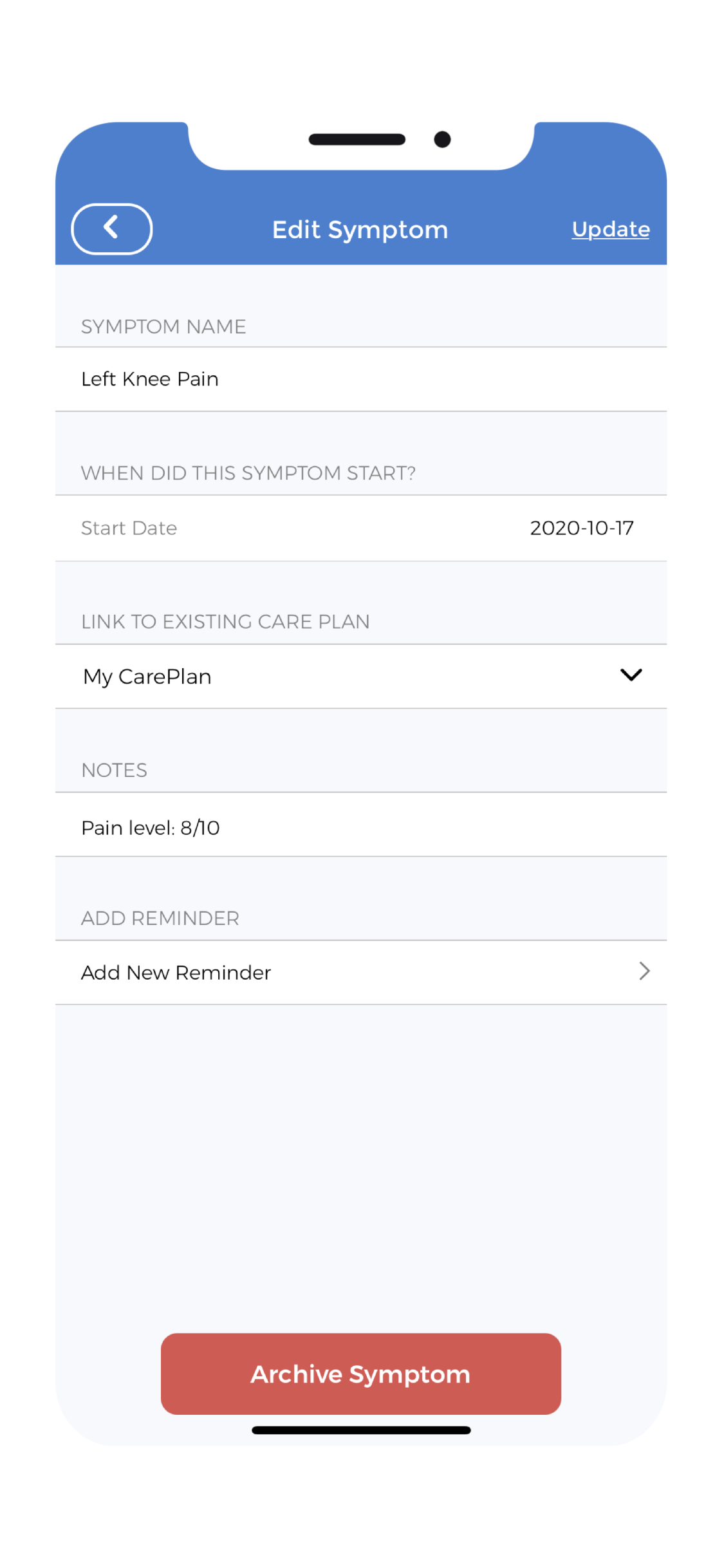
Tracker apps have become a trending topic. Medication, physical activity, symptoms, sleep are a few examples of what a tracker app can do for you. Sometimes we may forget to jot down our symptoms or think that we will be able to remember it. The symptom tracker is an excellent feature to help identify and determine what is affecting our health.
The CareClinic app allows the user to document and monitor medication as well as pain symptoms. This platform allows for the user to be proactive and in charge of their own health. It allows for the patient to gain a better understanding of their own health and determine the treatments that work for them. Finding effective treatments leads to effective results.
If you have ongoing treatment, record the effects and condition of your body before and after your treatment. Review and analyze any improvements in pain you experience. If you find that the treatment is worsening your symptoms then talk to your physician about stopping treatment. Factor in other activities and medication into your report to help determine the causes of your symptoms.
Report Monitoring
The reporting feature allows the user to monitor which medications or activities increase or decrease the pain. Effective management of chronic pain can be difficult. No one wants to be in a state of constant pain. No one wants to be dependent on someone else to help with performing daily tasks. Living with chronic pain can be disheartening. Put into practice ways to minimize your symptoms. In this article, Dr. Furmli highlights the advantages of using technology to help ease pain. Tracking your pain triggers is an advantageous aid in limiting the pain level and making it more tolerable.
“There’s a very close tie between good health and good education.” – Laura Bush
Since CRPS occurs due to some type of injury, be observant to the healing process of your body. Monitoring the injured area and being aware of other pains, can help to identify CRPS. CRPS stages have their respective symptoms, so keep track of the injured area. If you notice a few symptoms related to CRPS, then consult your doctor to verify.
Managing your health and wellness can be difficult. When you don’t see the results, it can also be disheartening. Being attentive to the signals your body sends you can help to improve your health quality. There are a lot of resources and information available to educate you on your healthcare journey. Always be informed about your condition and consult your trusted physician to connect you to the right resources. When you are educated about your condition, you increase your self-awareness. With increased self-awareness, you can find the best-suited prevention and treatments. If you can ease your symptoms effectively, you can get back to doing the things you love. Download the CareClinic app by tapping the banner below to start managing your health.