Pain Tracker
Trying to make sense of your pain? With CareClinic, you can track symptoms, lifestyle factors, and triggers like Anxiety — giving you the clarity you need to manage and improve your health daily.
Trying to make sense of your pain? With CareClinic, you can track symptoms, lifestyle factors, and triggers like Anxiety — giving you the clarity you need to manage and improve your health daily.
You've probably tried everything. Medications. Journals. Doctors. Avoiding your favorite foods. And still, the pain keeps coming back.
Maybe someone told you it's just stress. Maybe you were rushed out of an appointment in under 7 minutes. Maybe you started believing that nothing could fix it.
The problem isn't you. The problem is you've never had a way to connect the dots — until now.
Your doctor's memory isn't perfect. But your data can be.
Record your pain in seconds. Rate severity, note location, and track duration effortlessly.
Uncover connections between your pain, medications, foods, stress, and more.
Generate detailed reports for your healthcare providers with one click. Get taken seriously.
Catch worsening patterns early. Stop minor symptoms from becoming major health issues.
CareClinic helps cut that down. Way down.
Free to start. Advanced features available for power users.
Identify patterns between pain and changes in: Sleep, HRV, Steps, Heart Rate, Resting Heart Rate, Weight, Blood Pressure, and more.
Apple Health

Google Fit
Stop guessing about your health. Get the clarity you need with data-driven insights.
Track what triggers your pain such as stress, anxiety, lack of sleep.
Identifying your specific triggers can help you avoid or minimize them in your daily routine.
Frustrated that over-the-counter pain relievers, rest, and hydration aren't working consistently for your pain? Tracking reveals what's actually helping.
Consistent tracking provides objective data about treatment effectiveness, helping you and your healthcare provider make informed decisions.
Tired of not being taken seriously by doctors? Bring data, not just complaints, about your pain to get the care you deserve.
Without tracking:
Doctor: "It's probably just stress. Let's wait and see."
With CareClinic tracking:
Doctor: "These patterns are concerning. Let's run some tests to investigate further."
Stop suffering in silence. Join the thousands who've taken control of their health journey.
| Problem | What Most People Do | What Smart People Use |
|---|---|---|
| Pain | Ignore, Google symptoms, worry | CareClinic Tracker |
| Doctor Visits | Forget details, feel dismissed | CareClinic Reports |
| Treatment Effectiveness | Guess, waste time & money | CareClinic Analysis |
| Finding Triggers | Trial & error, months of frustration | CareClinic Patterns |
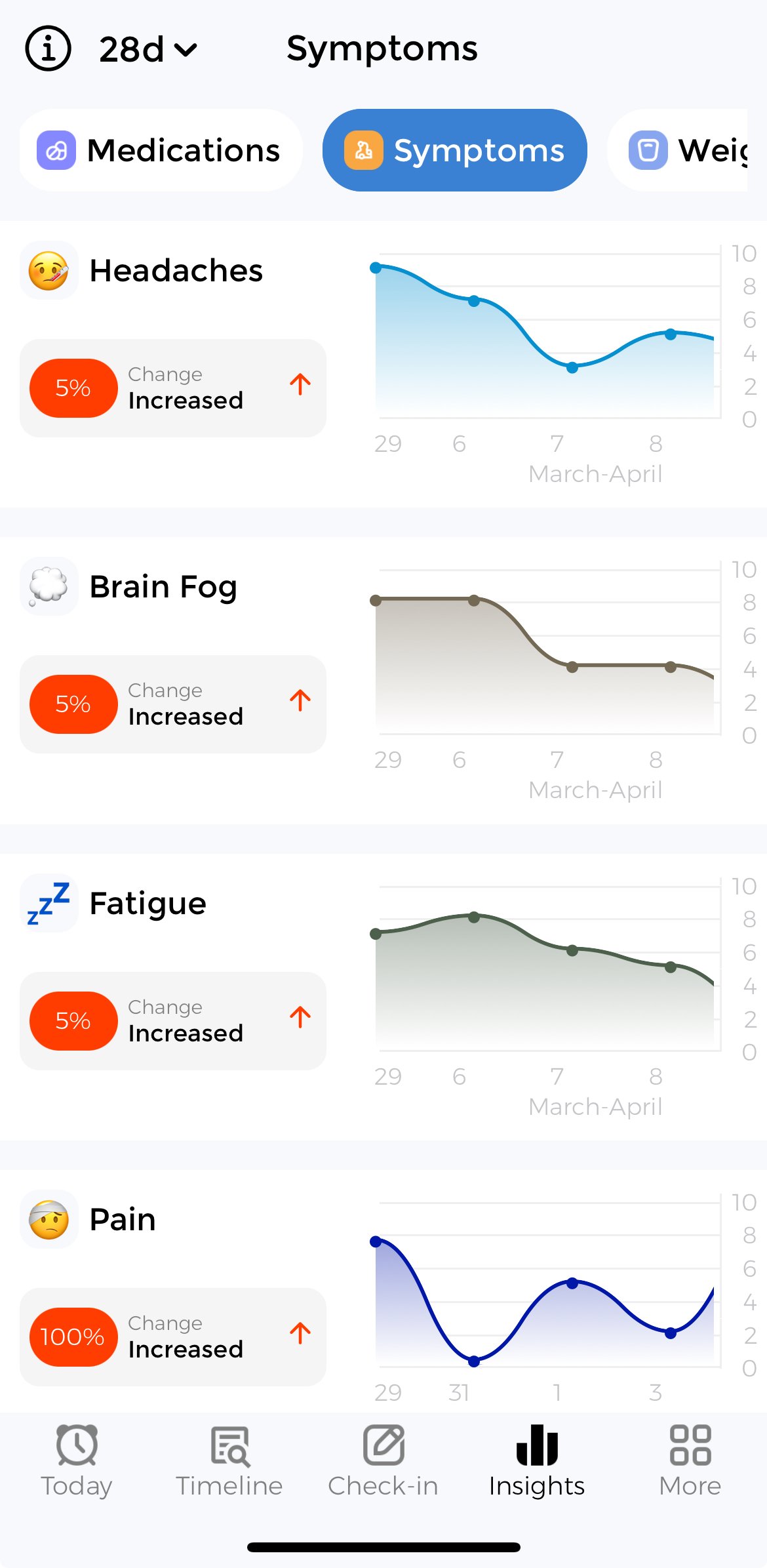
Visualize your progress, identify patterns, and see how lifestyle changes impact your symptoms over time.
The CareClinic app helps you visualize your pain severity over time, allowing you to:
The app automatically identifies patterns in your pain, showing you which days, times, or activities are associated with symptom changes.
Discover which triggers have the strongest impact on your pain with our correlation analysis. Focus on the factors that matter most.
Compare how different treatments affect your pain over time. Find what works best for your unique situation.
Start tracking today to generate your own personalized insights and charts.
Get Your Personalized ResultsTake complete control of your pain management with these powerful tracking features
Many people find that stress can affect their pain. Tracking this trigger may help identify patterns.
Many people find that anxiety can affect their pain. Tracking this trigger may help identify patterns.
Many people find that lack of sleep can affect their pain. Tracking this trigger may help identify patterns.
Many people find that dehydration can affect their pain. Tracking this trigger may help identify patterns.
Many people find that allergens can affect their pain. Tracking this trigger may help identify patterns.
Many people find that certain foods can affect their pain. Tracking this trigger may help identify patterns.
Many people find that caffeine can affect their pain. Tracking this trigger may help identify patterns.
Many people find that alcohol can affect their pain. Tracking this trigger may help identify patterns.
Many people find that weather changes can affect their pain. Tracking this trigger may help identify patterns.
Many people find that physical activity can affect their pain. Tracking this trigger may help identify patterns.
Identifying and tracking your personal triggers is the first step to managing your pain effectively.
Start Tracking Your TriggersUnderstanding conditions associated with your pain can help you have more informed conversations with your healthcare provider.
Endometriosis involves abnormal tissue growth outside uterus. Tracking symptoms helps monitor pain patterns and treatmen...
Infertility is the inability to conceive after one year of regular unprotected intercourse. Tracking ovulation, symptoms...
Fertility issues encompass various conditions that impair the ability to conceive or carry a pregnancy to term. Tracking...
Our comprehensive tracking tools provide everything you need to monitor, understand, and manage your pain.
Track severity, duration, location, and other characteristics of your pain with easy-to-use tools.
Identify potential triggers by connecting your pain to factors like sleep, diet, stress, and activity.
Never miss tracking with customizable reminders that help you maintain consistent records.
Generate detailed reports to share with healthcare providers for more informed discussions about your pain.
🎁 Includes: Guided check-ins, trigger discovery paths, and direct export to PDF for doctors.
Answer a few questions to better understand your symptoms and possible related conditions.
Thousands of people use CareClinic to track their pain and take control of their health.
Since I started tracking my pain with CareClinic, I've identified my triggers and reduced episodes by 60%. My doctor was impressed with the detailed reports.
The correlation features helped me discover that my pain worsens after certain foods. Making small changes based on the data has made a huge difference.
As a nurse, I recommend CareClinic to my patients with chronic pain. The detailed data helps their doctors make more informed treatment decisions.
CareClinic is the premier symptom tracking app available on iOS, Android, and Web, helping thousands of people feel more in control of their chronic mental and physical health conditions each year. CareClinic is recommended by leading health platforms including WebMD, Healthline, the National Science Foundation, Harvard University, and healthcare professionals worldwide.
Over 400,000 CareClinic members have used the app to identify triggers, track changes in symptom severity, and share detailed health data with doctors to aid with diagnosis and treatment. It's not just a free symptom tracker app – it's also the best health companion for anyone hoping to take control of every aspect of their physical and mental wellbeing.
CareClinic is recommended by leading healthcare organizations and professionals for managing pain and other chronic conditions.
"CareClinic's symptom tracking tools provide patients with valuable insights that can lead to more productive healthcare visits and better treatment outcomes."

Take control of your health before problems escalate. Start tracking your symptoms today and spot patterns you might be missing.