Lungs are made up of tube-like structures in different sizes connected in a series, with tiny sacs. The tubular structures start with the trachea, divides into the right and left bronchi. Bronchi subdivide and form bronchioles, and bronchioles end up in a small balloon-like sac called alveoli. The air you breathe goes through these tubular structures to the alveoli, where it exchanges the gases with the blood through the walls of alveoli and blood vessels closely located around the alveoli.
Fibrosis affects the alveoli or air sacs and the space around the alveoli. They do not affect the blood vessels directly, but with time due to the ineffectiveness of the gas exchange, the blood vessels become incapable of carrying oxygen. Ultimately, they will lead to respiratory failure.[1][2]
Causes of Idiopathic Pulmonary Fibrosis
The cause behind idiopathic pulmonary fibrosis is not identified, hence the name, idiopathic. Meanwhile, the following risk factors may be linked with the disease.
- Male sex: Males are predominant, accounting for up to 75% of patients with IPF.
- Age: Almost all patients with IPF are above 50 years of age.
- Cigarette smoking: Smoking is linked to nearly 75% of people with IPF. It includes both current and past cigarette smokers.
- Genetics (family history): It has a considerable (20%) association with idiopathic pulmonary fibrosis. If you have more than one member in your family with IPF, it is called familial pulmonary fibrosis.
- Gastroesophageal reflux disease (GERD): Approximately 75% of people with IPF have symptoms of acid reflux or heartburn.
Signs & Symptoms of Idiopathic Pulmonary Fibrosis
Since the course of pulmonary fibrosis differs from person to person, the severity of symptoms varies too. You might fall ill suddenly with severe disease or may experience a rapid worsening of your symptoms. This is known as acute exacerbation. This state will mandate immediate treatment with the medications, including but not limited to antibiotics and steroids. At a more complicated stage, people with acute exacerbations may need a mechanical ventilator as well.
On the other hand, you might have less severe symptoms that progress over a long period. Some others might develop milder disease and experience rapidly worsening symptoms that may last for several days to weeks.
The pulmonary fibrosis precipitated the following signs and symptoms.
- Breathlessness or shortness of breath
- Chronic cough
- Chest pain or tightness
- Loss of appetite
- Tiredness/fatigue
- Clubbing (club-like rounding of the tips of the fingers or toes)
- Unexplained weight loss
- Aching muscles and joints
Amongst the above, two main symptoms of IPF are,
Chronic Cough: A chronic cough that lasted longer than eight weeks were the symptom complained by about 85% of people with IPF. Even though it is often a dry cough, some people may cough up sputum.
Breathlessness or Shortness of Breath: Breathlessness can affect any activity you might involve in. Let it be an activity for daily living or an exercise. Initially, breathlessness may become noticeable during exercising, cycling or workout. But with time, climbing stairs, walking for a small distance might cause breathlessness. With the progression of the disease, because of increased scarring of the lung tissue, the severity of the breathlessness would worsen.[7][8]
Diagnosis for Idiopathic Pulmonary Fibrosis
Since different kinds of interstitial lung diseases cause inflammation and fibrosis and treatments differ according to the cause, making a precise diagnosis is essential to differentiate idiopathic pulmonary fibrosis from them.[9][10]
Understanding IPF Status
The most important thing to remember is, not all humans are identical, so do the disease progressions. Your physician knows your medical history so they can choose the most appropriate treatment plan for you. If you have been referred to a respirologist or respiratory physician, try to make sure that you clarify your questions from them.
- Track your symptoms over an adequate period to get a clear picture.
- Prepare your questions well ahead of meeting your physician.
- Share and discuss the list of symptoms you experienced.
- Make notes of your discussion with the physician.
- Bring all your medications/supplements/drugs you take to the physician.
- If you feel comfortable, try to have a family member/friend accompany you.
- Discuss the course of treatment, non-medical remedies, follow-up visits and goals to achieve, etc.
- Get information about programs and support groups in your community that help people with IPF and other lung diseases.
- Ask about enrolling in a pulmonary rehabilitation program (if available)
Your healthcare would not be relying solely on your physician. It will involve a care team that can be updated in your CareClinic app. It will include physician doctor(s), including your family doctor and a respirologist (lung specialist), nurse, certified respiratory educator/therapist, respiratory nurse, cardiopulmonary physiotherapist, occupational therapist, etc.[11]
Treatment for Idiopathic Pulmonary Fibrosis
Medications
No cure is available for idiopathic pulmonary fibrosis. Treatment for idiopathic pulmonary fibrosis is focused on slowing the scarring than curing the damage that already occurred.
There are no procedures or medications capable of removing scarring. In addition to those medications that slow down the progression of scarring, other medications will help with the symptoms. These drugs will include therapy for breathlessness, therapy for gastroesophageal reflux, etc. As a medication, some people might experience some side effects from these medications too. Considering the focus of the article, in-depth information on drugs is avoided here.
Apart from medications, other therapies such as supplemental oxygen therapy, exercise training, pulmonary rehabilitation are also valuable for treating idiopathic pulmonary fibrosis. Lung transplant is considered a last resort and the only solution for IPF.
Non-Medical Therapies
Lifestyle Changes
Since the nature of the disease is progressive and irreversible, learning to cope-up with the disease would be helpful.
- Smoking cessation – the foremost recommended thing to help with any lung disease.
- Keep yourself away from people with chest infections and colds.
- Wash your hands well and frequently.
- Get your flu shot annually.
- Stay as fit as you can.
Supplementary Oxygen
As we read before, scarring diminishes the oxygen transfer from the inhaled air to the blood capillaries surrounding the alveoli in the lungs. As a result, you might feel tired and breathless. And the intensity of these symptoms may differ between people and activities. It is not mandatory to provide supplementary oxygen therapy for all IPF patients but with low blood oxygen levels.
If you have been diagnosed with low blood oxygen levels, your physician may prescribe supplemental oxygen. It can help you relieve your symptoms. Depending on your requirement, you might need it all the time or during specific activities only.
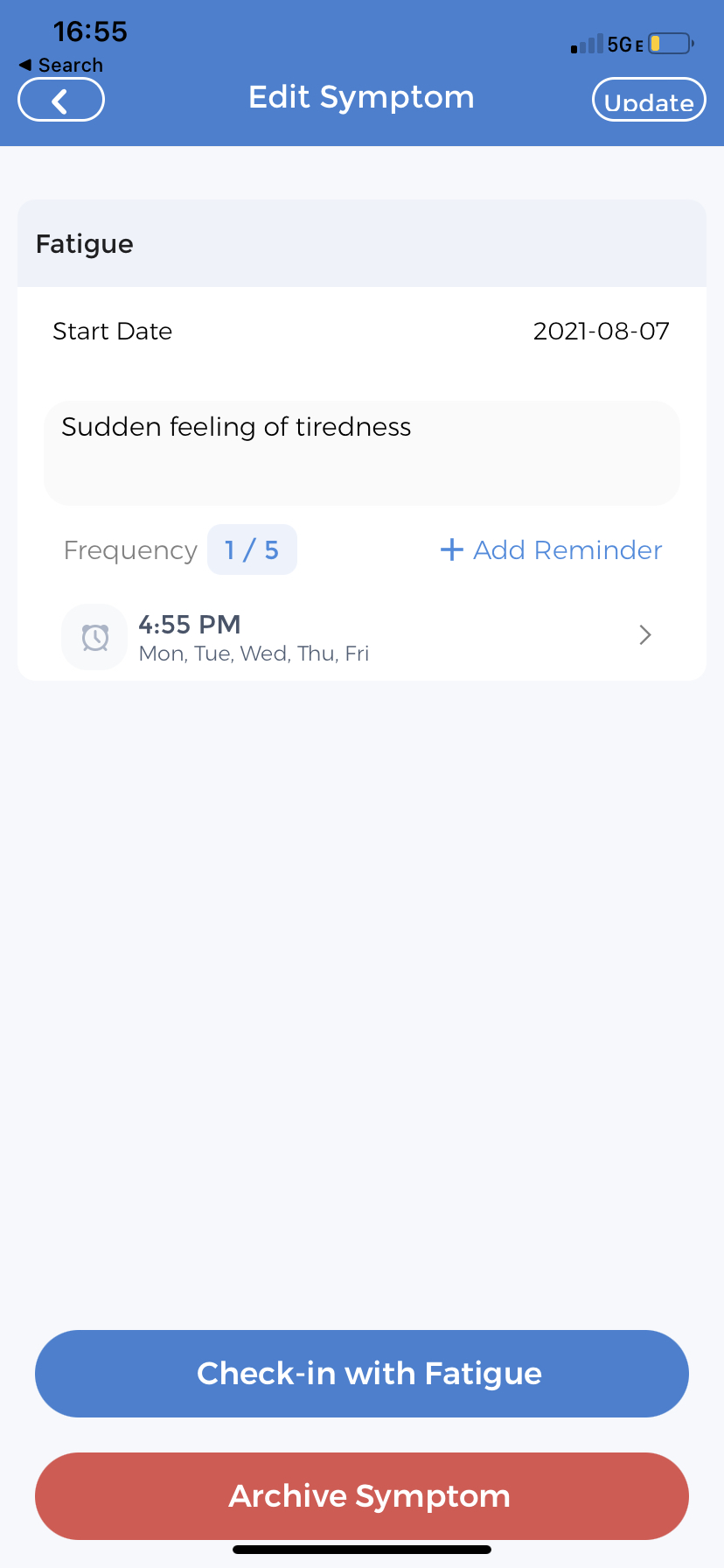
Critical practice with oxygen is to stick with the prescription. Since you need adequate oxygen for your body’s normal functions, you should keep using it as prescribed. If you identify any symptoms occurring during the use of oxygen, make sure you record it using the symptom tracker feature of the CareClinic app.
Pulmonary Rehabilitation
Pulmonary rehabilitation is an educational program for patients with lung diseases. This program educates patients on various aspects of coping with their illness and breathing more efficiently to perform daily life activities.
Lung Transplant
A lung transplant is an organ transplant surgery to replace your diseased lung with a healthy lung from a person who has died. Our body is capable of working with just one healthy lung. The majority of the patients get one lung, but they may get both lungs new in some cases.
Lung transplant is the ultimate resort to getting rid of IPF, but it is still not suitable for everyone. It should be decided by your physician, considering various factors. If you are eligible for a transplant, you will have to wait for some (or long) time till you find an appropriate donor. The surgery might mandate lifelong drugs, which are necessary to prevent rejection.
Since the article focuses on transplant and post-transplant care using the CareClinic app, let us dive into some detail about the post-surgical state.
Post-Lung Transplant Care at Home
Wound Care
You can follow your wound care using the daily check-in feature. You can add your notes about the status of your wound daily so that it will be easy to compare and find the abnormality.
Follow-up care is the key to success for a post-transplant patient. Make sure you attend all appointments without fail. Get the emergency contact numbers to reach out to your care team members so that you can contact them quickly. CareClinic has a dedicated feature for this purpose to include information about your care team.
Immediate post-surgical care is mainly related to wound care and related physiotherapy. The surgical wound sites would cause some pain and numbness for a couple of weeks following surgery. Regular surgical clinic follow-up will be mandatory, and your physician will advise you to work with a respiratory therapist to make your new lungs function effectively.
The diary feature and symptom checker features of the CareClinic app will help you monitor your symptoms like pain, bleeding, or oozing from surgical sites or difficulty in breathing, etc. Also, the therapy feature will be handy to follow up with your therapies, especially with the respiratory and occupational therapist.
Medications
Since the new lung is from another individual, there is a chance of your body treating the new lung as a foreign body. Therefore, anti-rejection drugs are essential to prevent your body reject the new lung tissue. You should use these drugs lifelong. Similar to any other medication, it has its side effects. The most important side effect is less immunity to infections. Hence it is advisable to avoid crowded places, frequent handwashing, use of face masks. Most importantly, avoid people who might have an illness such as a cold or influenza. The medication reminder feature of the CareClinic app will help you remember your anti-rejection drugs, along with other medications.
The medication tracker feature in the CareClinic app fulfills your requirement of following your medications all in one place. Also, this feature reminds you when it is time to take your pill.
Tips to Follow
- If you are on medications for other diseases and have been withheld for the surgery, your physician will let you know when to restart your medicines. If necessary, they might change your medications in terms of dose and frequency as well.
- Never forget to take your anti-rejection medicines. Follow the physician’s order precisely as prescribed. If you encounter any problems or are in doubt, call your doctor or nurse.
- Take pain medicines as directed, and do not consume painkillers like aspirin, ibuprofen, or other non-steroidal anti-inflammatory drugs without consulting your physician.
- If you encounter any side effects from your pain medicine talk to your doctor.
- Take prescribed antibiotics as directed to complete the entire course of antibiotics.
Mental Health Support
Mental support is critical during the recovery of the post-transplant period. The pain, drug dependency, thoughts about the future, everything would affect your mental health. That is the reason adequate family support is an essential factor in deciding transplant surgeries. Reach out to family, friends, counsellors, and your physician if you need help. You can record your mood and thoughts using the diary feature of the app.
Activity Tracking
Track your daily activities using the diary check-in or activity tracking feature of the CareClinic app.
- If you ever feel tired, take adequate rest. Adequate sleep and hydration will help you a lot.
- Try to walk regularly. But increase the distance or time little by little. Walking helps your lung to work efficiently while preventing pneumonia.
- Avoid strenuous activities, such as weightlifting, jogging, or aerobic exercise, for 4 to 6 weeks. Lifting any kind of weight might stress your body.
- Always hold a pillow over the surgical site when you cough. It will reduce the pain you experience.
- Practice breathing and follow breathing exercises advised by your therapist to make your lung function and prevent pneumonia.
- If at all you have any questions, reach out to your physician for answers. Do not make assumptions or rely on solutions on the internet. Every person is different, and your physician is your best option to get appropriate advice.
Tracking Diet
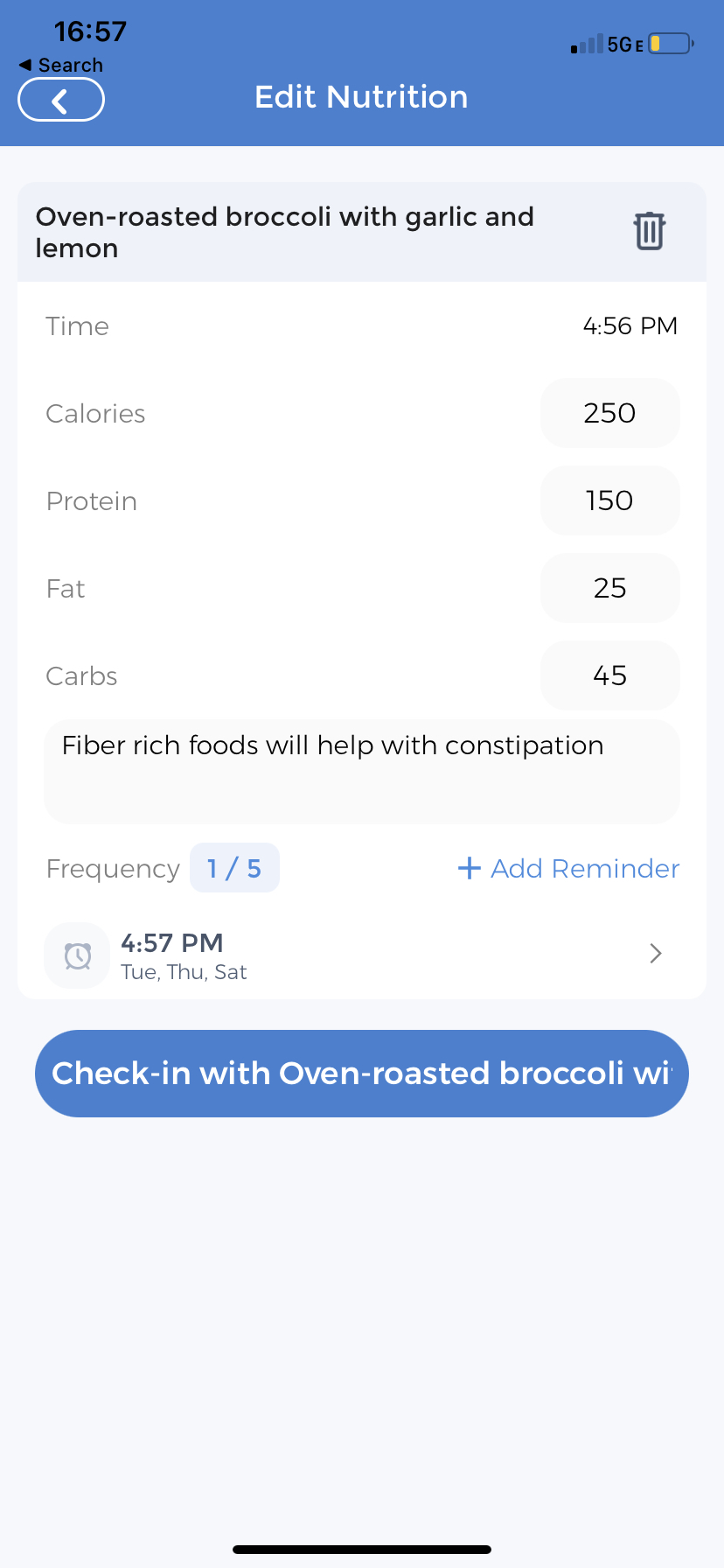
CareClinic nutrient tracker will be handy to track all your diet and nutritional intake.
- Always follow your physician’s instructions about diet after your surgery.
- If told not to do so, drink plenty of fluids.
- Do not take alcohol since it might interact with your anti-rejection medications. Check with your doctor before you drink alcohol.
- Constipation following surgery is common. Follow doctor’s advice to eat fibre-rich food or supplement and adequate water intake.
[12][13][14][15][16][17][18][19][20]
CareClinic for Post Lung Transplant Support
Practicing regular tracking of your health is essential and useful for everyone. CareClinic is a one-stop personal health app, providing numerous useful features to help you maintain a personal health record. Create a self-care action plan, add medications, supplements, diet, physical activities, and therapies you receive. You can even set your healthcare team that manages your health. Add your physician, registered nurse, and family members to keep them in the loop. As a summary of the features, the CareClinic app offers your best personal healthcare app companion.
All these features of the CareClinic app will be more helpful after your lung transplant.
Diary Entry Tracking
The diary entry feature lets you make entries about your daily life. Use the app’s diary entry feature to track day-to-day activities or events you encounter. You will realize how important it is to monitor your days tracking your symptoms (e.g., breathless episodes) and associated activities.
Symptom Tracking for Idiopathic Pulmonary Fibrosis
The symptom tracker lets you add symptoms you are experiencing after the lung transplant. You can start tracking them whenever you experience any of the symptoms mentioned above. Including IPF, if you have any medical conditions or are on any medications, you can start tracking your symptoms before seeking medical attention and compare how well the therapy relieves you from symptoms after visiting the doctor’s office. This helps seek medical attention during the worsening of disease-related symptoms, which might lead to complications.
Pill Tracking for Idiopathic Pulmonary Fibrosis
Medications are important, after your lung transplant. Never forget your medications – including your anti-rejection drugs and painkillers with the CareClinic app. Get reminders before you run out of medications. Have a look at our blog article on pill tracking.
Nutrition for Idiopathic Pulmonary Fibrosis
CareClinic offers a nutrition tracker, which helps you maintain your diet log. When you are in the post-transplant period, it is essential to keep track of your food to ensure adequate nutrition is taken for your speedy recovery and avoiding constipation, etc. If you have a specific diet to change your food habit, you can follow your diet and reflect on how you can live a healthy life.
Activities for Idiopathic Pulmonary Fibrosis
Use this feature to track any and all activities you do. CareClinic’s activity tracker lets you identify any actions that worsen or relieves your symptoms. You can figure out which activities help improve your symptoms and which don’t. If you suffer from non-IPF specific symptoms like fatigue, you can identify them easily by reviewing your activities. You can look back to see if there are any correlations between your symptoms and any activity you may have participated in. Similarly, you can identify activities worsening your pain after your lung transplant.
Therapy for Idiopathic Pulmonary Fibrosis
Keep a record of therapies you may be receiving. Maybe you are seeing a respiratory physician or your family doctor. You can record all your appointments so that you never forget something. Since you will need to follow respiratory or occupational therapy following a lung transplant, this feature will become handy in managing all your therapies in one place.
Report Tracking for Idiopathic Pulmonary Fibrosis
Reports are another great feature in the CareClinic app. They can provide a lot of perception into your lifestyle. CareClinic’s reports consider your logs in the diary, nutrition, activities, symptoms, etc., and subsequently generate reports to show the associations between those entries. This connection would be helpful to learn more about yourself, your IPF-related and post-transplant symptoms.
In summary, using an all-in-one app like CareClinic as an idiopathic pulmonary fibrosis transplant app can help you lead a healthy post-transplant life.
References
- “”. https://www.nhs.uk/conditions/idiopathic-pulmonary-fibrosis/
- “How Lungs Work | American Lung Association”. https://www.lung.org/lung-health-diseases/how-lungs-work
- “Pulmonary Fibrosis – Causes and Risk Factors | NHLBI, NIH”. https://www.nhlbi.nih.gov/health/idiopathic-pulmonary-fibrosis/causes
- “Pulmonary Fibrosis – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC7120641/
- “Familial pulmonary fibrosis is the strongest risk factor for idiopathic pulmonary fibrosis”. https://pubmed.ncbi.nlm.nih.gov/21917441/
- “Idiopathic pulmonary fibrosis beyond the lung: understanding disease mechanisms to improve diagnosis and management | Respiratory Research | Full Text”. https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-021-01711-1
- “Acute exacerbation of idiopathic pulmonary fibrosis: who to treat, how to treat – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC7732144/
- “Pulmonary Fibrosis – Symptoms | NHLBI, NIH”. https://www.nhlbi.nih.gov/health/idiopathic-pulmonary-fibrosis/symptoms
- “An Official ATS/ERS/JRS/ALAT Statement: Idiopathic Pulmonary Fibrosis: Evidence-based Guidelines for Diagnosis and Management – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC5450933/
- “Idiopathic Pulmonary Fibrosis (IPF) Guidelines: Guidelines Summary”. https://emedicine.medscape.com/article/301226-guidelines
- “Pulmonary Rehabilitation | Pulmonary Fibrosis Foundation | Pulmonary Fibrosis Foundation”. https://www.pulmonaryfibrosis.org/understanding-pff/treatment-options/pulmonary-rehabilitation
- “A Review of the Treatment and Management of Idiopathic Pulmonary Fibrosis”. https://www.uspharmacist.com/article/a-review-of-the-treatment-and-management-of-idiopathic-pulmonary-fibrosis
- “Consensus document for the diagnosis and treatment of idiopathic pulmonary fibrosis | Pulmonology”. https://www.journalpulmonology.org/en-consensus-document-for-diagnosis-treatment-articulo-X0873215916514648
- “Idiopathic pulmonary fibrosis”. https://en.wikipedia.org/wiki/Idiopathic_pulmonary_fibrosis
- “Discharge, Planning & Recovery | Lung Transplant”. https://my.clevelandclinic.org/departments/transplant/programs/lung/recovery
- “Critical care considerations in the post-operative period for the lung transplant patient – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC8662514/
- “Lung Transplant Recovery and Follow-Up Care | Spectrum Health”. https://www.spectrumhealth.org/services/heart-lung-and-vascular-care/transplant/lung/recovery-and-follow-up-care
- “Post-Lung Transplant Surgery – Penn Medicine”. https://www.pennmedicine.org/for-patients-and-visitors/find-a-program-or-service/harron-lung-center/lung-transplant/treatments-and-procedures/post-lung-transplant-surgery
- “A Patient and Family Guide to Lung Transplant Success | Columbia Surgery”. https://columbiasurgery.org/thoracic/cf-patient-and-family-guide-lung-transplant-success
- “Post-Lung Transplant Recovery & Aftercare | UPMC”. https://www.upmc.com/services/transplant/lung/process/after


