Living with Crohn’s disease can pose many challenges, but with the right self-care practices, you can manage your symptoms effectively and improve your overall well-being. This comprehensive guide will provide you with valuable insights and practical tips on how to optimize your self-care routine for Crohn’s disease. Whether you’re newly diagnosed or have been living with this chronic condition for years, this guide will empower you to take control of your health and live your life to the fullest.[1][2][3][4]
Understanding Crohn’s Disease
The Basics of Crohn’s Disease
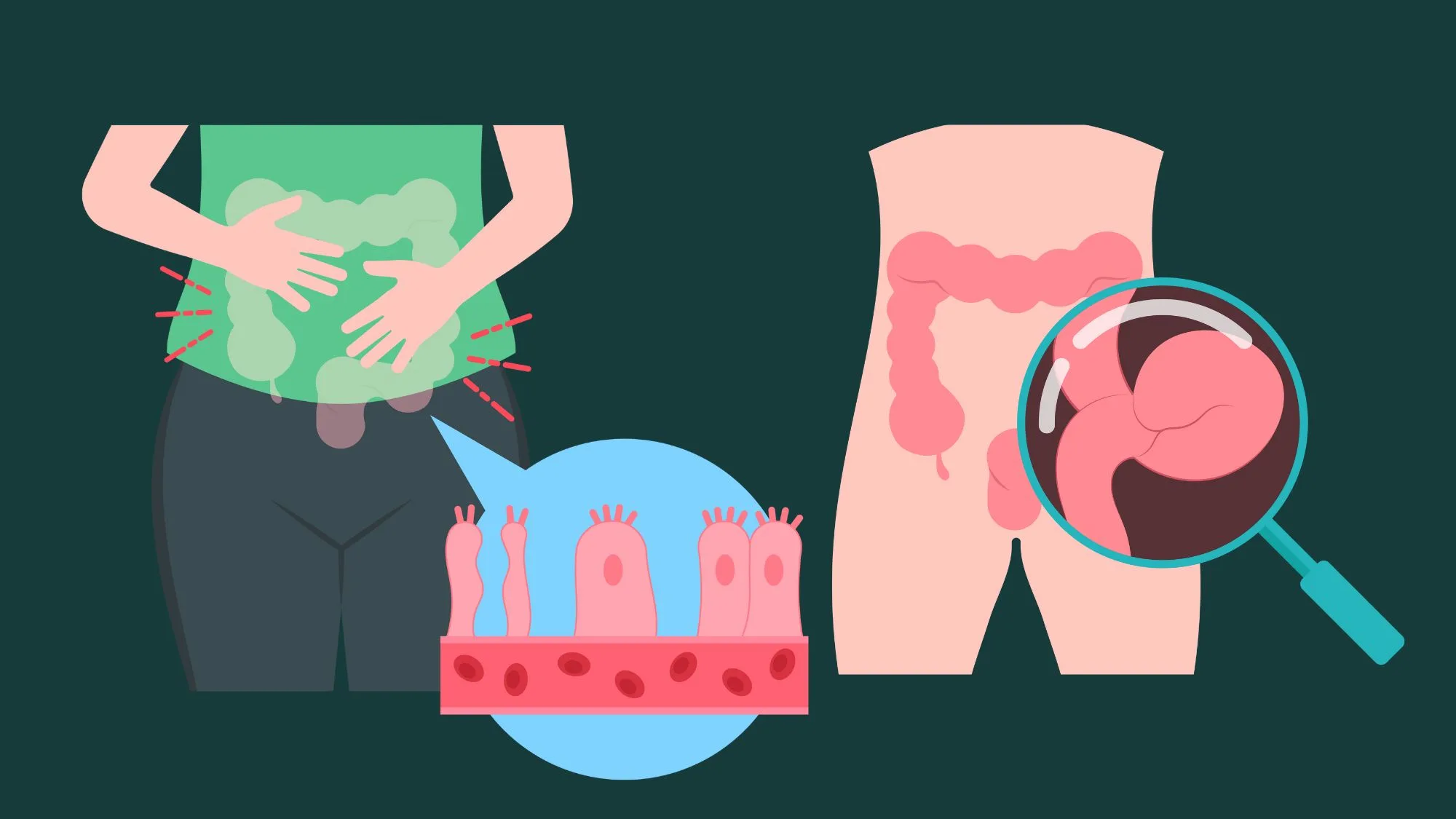
Crohn’s disease is a chronic inflammatory bowel disease that primarily affects the digestive tract. It can cause inflammation anywhere from the mouth to the anus, but the most common site of inflammation is the small intestine. This condition occurs when the immune system mistakenly attacks the healthy cells in the digestive tract, leading to the development of inflammation and various symptoms.
When it comes to understanding Crohn’s disease, it is important to consider the multifactorial nature of this condition. While the exact cause of Crohn’s disease is unknown, research suggests that it may be the result of a combination of genetic, environmental, and immune system factors. Studies have shown that individuals with a family history of Crohn’s disease are more likely to develop the condition themselves. Additionally, certain lifestyle factors such as smoking and diet may increase the risk of developing Crohn’s disease.
Genetics play a significant role in the development of Crohn’s disease. Researchers have identified several genes that are associated with an increased susceptibility to this condition. However, it is important to note that having these genes does not guarantee the development of Crohn’s disease. Environmental factors, such as exposure to certain bacteria or viruses, may trigger the immune system response in individuals who are genetically predisposed to the condition.
Symptoms and Diagnosis
The symptoms of Crohn’s disease can vary from person to person and may range from mild to severe. Some common symptoms include abdominal pain, diarrhea, rectal bleeding, weight loss, fatigue, and reduced appetite. It’s important to keep track of your symptoms and report them to your healthcare provider to aid in the diagnosis and management of your condition.
Diagnosing Crohn’s disease can be a complex process that requires a thorough evaluation of symptoms and various diagnostic tests. Your healthcare provider may order blood tests to check for inflammation markers and to rule out other conditions. Stool tests can help identify any infections or signs of inflammation in the digestive tract. Endoscopy and colonoscopy may be performed to directly visualize the digestive tract and obtain tissue samples for biopsy. Imaging tests, such as CT scans or MRIs, can provide detailed images of the digestive tract to assess the extent of inflammation.
It is important to note that Crohn’s disease can sometimes be challenging to diagnose, as its symptoms can overlap with other gastrointestinal conditions. Therefore, a comprehensive evaluation by a healthcare professional is crucial to ensure an accurate diagnosis.
Long-Term Effects of Crohn’s Disease
Crohn’s disease is a chronic condition, meaning it requires ongoing management. If left uncontrolled, it can lead to complications such as bowel obstruction, malnutrition, fistulas, abscesses, and even an increased risk of colorectal cancer.
Managing Crohn’s disease involves a multidisciplinary approach that includes medication, lifestyle modifications, and regular monitoring. Medications such as anti-inflammatory drugs, immunosuppressants, and biologics are commonly used to reduce inflammation and control symptoms. In some cases, surgery may be necessary to remove damaged portions of the digestive tract or to address complications such as fistulas or strictures.
Adopting a healthy lifestyle can also play a significant role in managing Crohn’s disease. This may include following a balanced diet that is low in trigger foods, such as spicy or fatty foods, and high in nutrients. Regular exercise, stress management techniques, and adequate sleep are also important for overall well-being and can help reduce inflammation and improve symptoms.
Regular follow-up appointments with your healthcare provider are essential to monitor your condition and adjust your treatment plan as needed. They can help identify any potential complications or changes in your symptoms and provide guidance on managing flare-ups.
Living with Crohn’s disease can be challenging, but with proper self-care and medical treatment, the risk of experiencing long-term complications can be reduced. It’s essential to work closely with your healthcare provider to develop a personalized treatment plan that addresses your specific needs and to seek support from patient advocacy groups or support networks to connect with others who understand the challenges of living with this condition.[5]
Importance of Self-Care in Managing Crohn’s Disease
Role of Self-Care in Disease Management
Self-care plays a crucial role in managing Crohn’s disease and minimizing the impact of symptoms on your daily life. By adopting healthy lifestyle habits and making informed choices, you can improve your overall well-being and potentially reduce the frequency and severity of flare-ups.
 One tool that can greatly assist you in tracking your symptoms, monitoring your medication adherence, and even managing your overall well-being is the CareClinic app. This user-friendly and comprehensive app allows you to easily record your symptoms, set medication reminders, track your diet, and connect with a supportive community of individuals living with similar conditions.
One tool that can greatly assist you in tracking your symptoms, monitoring your medication adherence, and even managing your overall well-being is the CareClinic app. This user-friendly and comprehensive app allows you to easily record your symptoms, set medication reminders, track your diet, and connect with a supportive community of individuals living with similar conditions.
Managing Crohn’s disease requires a multifaceted approach, and self-care is a fundamental aspect of this strategy. It involves taking an active role in your own health and well-being, empowering yourself with knowledge, and implementing lifestyle changes that can positively impact your disease management.
One of the key components of self-care for Crohn’s disease is maintaining a healthy diet. A balanced and nutritious diet can help reduce inflammation, support gut health, and alleviate symptoms. It is important to work with a registered dietitian or nutritionist to develop a personalized eating plan that takes into consideration your specific dietary needs and restrictions.
Regular exercise is another crucial aspect of self-care for Crohn’s disease. Engaging in physical activity can help improve digestion, reduce stress, and boost overall well-being. However, it is important to consult with your healthcare provider before starting any exercise regimen, as certain activities may exacerbate your symptoms.
Benefits of Self-Care for Crohn’s Patients
Engaging in self-care practices tailored to your specific needs can have numerous benefits for managing Crohn’s disease. Some of the benefits include:
- Better symptom control: By actively participating in self-care, you can gain a better understanding of your triggers and learn how to effectively manage your symptoms. This can lead to fewer flare-ups and a more predictable disease course.
- Improved quality of life: Self-care practices can enhance your overall well-being and help you lead a fulfilling life, despite the challenges posed by Crohn’s disease. By prioritizing self-care, you can focus on activities and relationships that bring you joy and fulfillment.
- Reduced need for medication: While medication is often essential in managing Crohn’s disease, adopting healthy lifestyle habits through self-care may reduce the reliance on medication and its potential side effects. By taking proactive steps to manage your disease, you may be able to achieve better symptom control and minimize the need for higher doses or additional medications.
- Enhanced emotional well-being: Self-care practices can have a positive impact on your mental and emotional health. By engaging in activities that promote relaxation, self-reflection, and self-care, you can reduce stress, anxiety, and depression commonly associated with chronic illnesses like Crohn’s disease.
- Increased self-empowerment: Taking an active role in your own health and well-being through self-care can empower you to make informed decisions, advocate for yourself, and effectively communicate with your healthcare team. This sense of empowerment can lead to better disease management and improved outcomes.
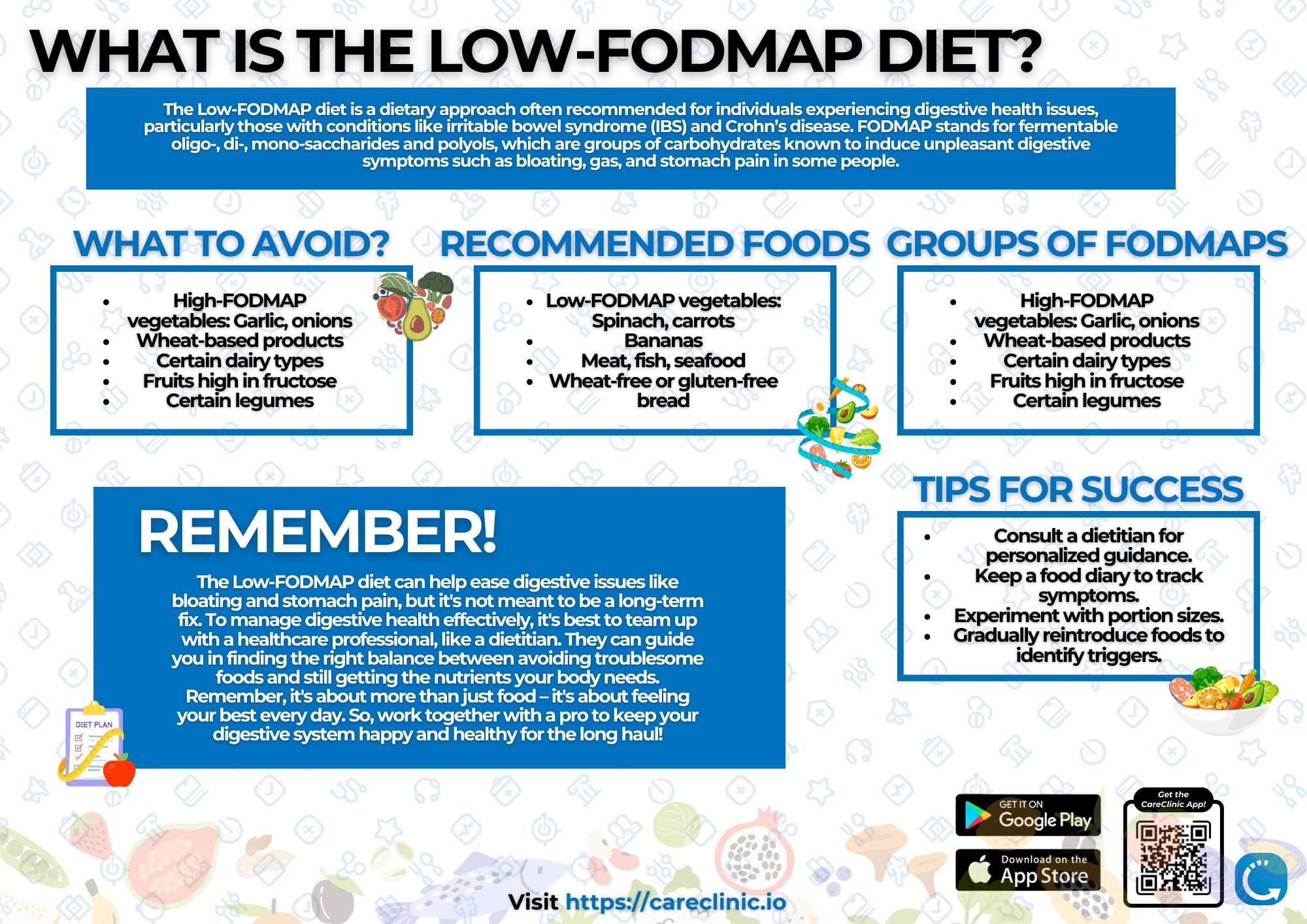
Nutritional Strategies for Crohn’s Disease
Foods to Include in Your Diet
A well-balanced and nutritious diet is vital for managing Crohn’s disease and promoting gut health. While individual dietary needs may vary, incorporating the following types of foods can be beneficial:
- Fiber-rich fruits and vegetables: Choose low-fiber options, such as cooked or pureed fruits and vegetables, to minimize irritation to the digestive tract. Examples include bananas, applesauce, cooked carrots, and peeled cucumbers.
- Lean proteins: Opt for lean sources of protein, such as chicken, fish, tofu, and eggs, to ensure an adequate intake without adding unnecessary stress to your digestive system.
- Healthy fats: Include sources of healthy fats, such as avocados, olive oil, nuts, and seeds, in moderation, as they provide essential nutrients and promote overall well-being.
- Probiotic-rich foods: Probiotics can help maintain a healthy balance of gut bacteria. Consider incorporating yogurt, kefir, sauerkraut, and kimchi into your diet.
In addition to the above recommendations, it can be beneficial to include other specific foods in your diet to support your overall health while managing Crohn’s disease. For example, incorporating omega-3 fatty acids, found in fatty fish like salmon and mackerel, can help reduce inflammation in the body. Consuming foods rich in antioxidants, such as berries, spinach, and kale, can also provide additional support for your immune system.
Incorporating herbs and spices known for their anti-inflammatory properties, such as turmeric, ginger, and garlic, can be a flavorful way to enhance the nutritional value of your meals. These ingredients not only add depth of flavor but also offer potential health benefits, including reducing inflammation and supporting gut health.
Foods to Avoid
While making conscious choices about what to include in your diet is important, it’s equally essential to be aware of foods that may trigger symptoms and exacerbate inflammation. Some common trigger foods for individuals with Crohn’s disease include:
- High-fiber foods: These can be difficult to digest and may worsen symptoms. Examples include whole grains, raw vegetables, and seeds.
- Spicy and high-fat foods: These can lead to increased inflammation and discomfort. Limit your intake of spicy foods, fried foods, and high-fat meals.
- Dairy products: Some individuals with Crohn’s disease may experience lactose intolerance or have sensitivity to dairy products. If this applies to you, consider opting for lactose-free alternatives instead.
- Processed foods and sugary snacks: These foods typically lack nutritional value and may contribute to inflammation and exacerbate symptoms. Choose whole, unprocessed foods whenever possible.
It’s important to note that while these foods may be triggers for some individuals, everyone’s experience with Crohn’s disease is unique. It’s essential to pay attention to your body’s response to different foods and make adjustments accordingly.
Hydration and Crohn’s Disease
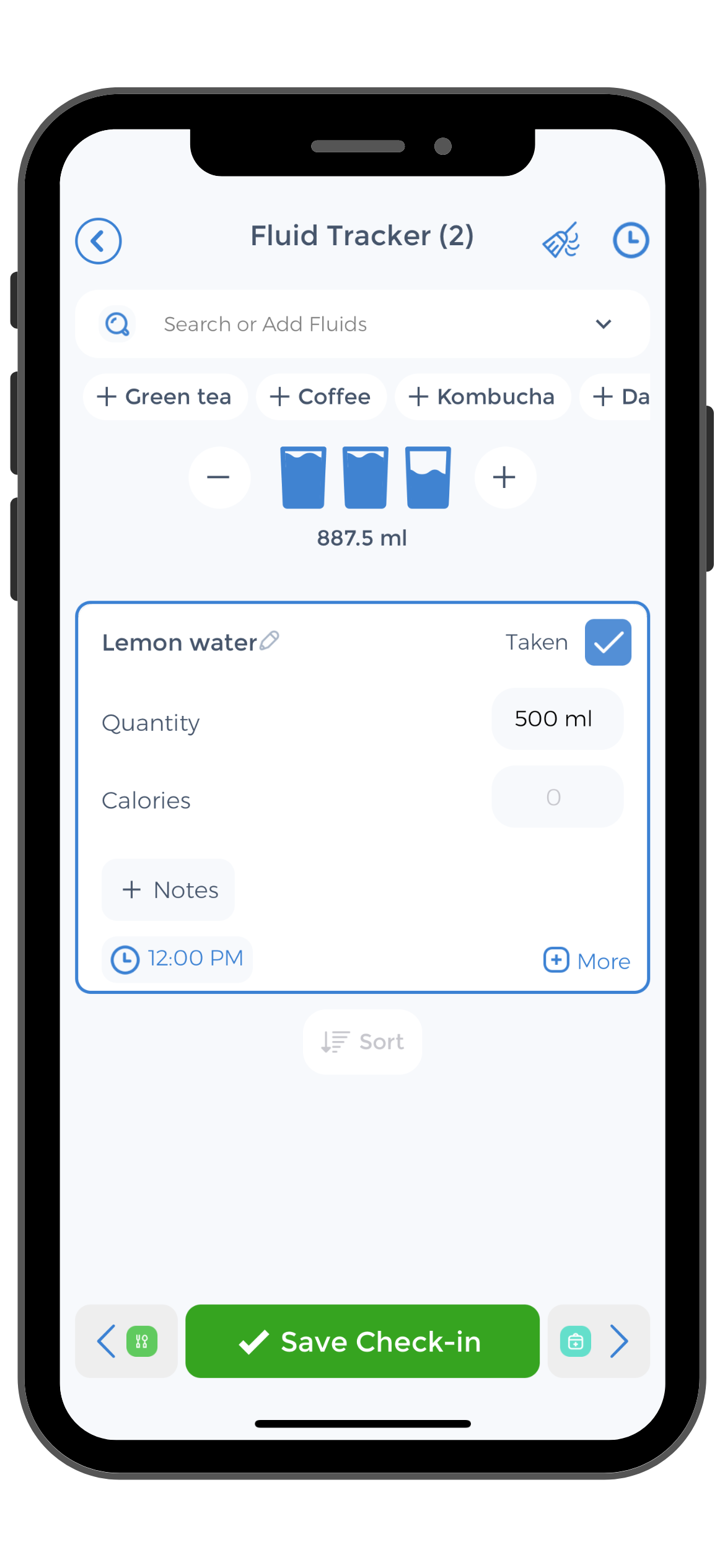 Maintaining proper hydration is essential for individuals with Crohn’s disease, as it helps support digestion, improve gut health, and prevent dehydration. Aim to drink an adequate amount of water throughout the day, and monitor your urine color to ensure you are well-hydrated. It’s important to note that certain medications or active periods of Crohn’s disease may increase the risk of dehydration, so be mindful of your fluid intake during these times.
Maintaining proper hydration is essential for individuals with Crohn’s disease, as it helps support digestion, improve gut health, and prevent dehydration. Aim to drink an adequate amount of water throughout the day, and monitor your urine color to ensure you are well-hydrated. It’s important to note that certain medications or active periods of Crohn’s disease may increase the risk of dehydration, so be mindful of your fluid intake during these times.
In addition to water, incorporating other hydrating beverages can be beneficial. Herbal teas, such as chamomile or peppermint, can provide soothing effects on the digestive system. Coconut water is another hydrating option that also provides electrolytes, which can be beneficial during periods of diarrhea or excessive fluid loss.
It’s important to consult with a healthcare professional or registered dietitian who specializes in gastrointestinal health to develop an individualized nutrition plan that takes into account your specific needs and preferences. They can provide guidance on portion sizes, meal timing, and any necessary modifications to ensure you are getting the nutrients you need while managing Crohn’s disease.[7][8]
Exercise and Physical Activity
Safe Exercises for Crohn’s Patients
Engaging in regular physical activity can have numerous benefits for individuals with Crohn’s disease. Exercise can help alleviate stress, improve digestion, boost mood, and enhance overall well-being. However, it’s essential to choose exercises that are safe and suitable for your individual condition. Some low-impact exercises that are generally well-tolerated by individuals with Crohn’s disease include:
- Walking: Brisk walking is an excellent form of cardiovascular exercise that is gentle on the joints and can be easily adjusted to your fitness level.
- Yoga: Practicing gentle yoga poses and deep breathing exercises can help reduce stress and promote relaxation.
- Swimming: Swimming is a low-impact exercise that provides a full-body workout without placing excessive stress on the joints.
- Cycling: Cycling is a great option for individuals looking for a low-impact cardiovascular workout. You can choose outdoor cycling or use a stationary bike indoors.
Benefits of Regular Physical Activity
Regular physical activity offers numerous benefits for individuals with Crohn’s disease, including:
- Improved digestive function: Exercise helps stimulate bowel movements and enhances digestion, potentially reducing the frequency and severity of gastrointestinal symptoms.
- Stress relief: Physical activity can act as a natural stress reliever and improve mental well-being, which is particularly important for individuals with chronic conditions like Crohn’s disease.
- Increased energy levels: Engaging in regular exercise can boost your energy levels, reduce fatigue, and improve overall vitality.
Precautions While Exercising
While physical activity can be beneficial, it’s important to take certain precautions to avoid exacerbating your symptoms or causing injury. Here are some key considerations:
- Listen to your body: If you experience pain, discomfort, or other symptoms during exercise, it’s important to listen to your body and modify or stop the activity as needed.
- Stay hydrated: Make sure to drink plenty of water before, during, and after exercise to stay adequately hydrated and minimize the risk of dehydration.
- Warm up and cool down: Prioritize warm-up exercises, such as stretching, to prepare your muscles and joints for physical activity. Also, remember to cool down and stretch after each workout to promote recovery.
- Work with a healthcare professional: If you have concerns or specific limitations, consult with a healthcare professional or a certified exercise specialist who can provide personalized guidance on exercise modifications tailored to your individual needs.
Mental Health and Coping Strategies
Understanding the Emotional Impact of Crohn’s Disease
Crohn’s disease can have a significant emotional impact on individuals, as living with a chronic illness can be challenging and stressful. It’s important to acknowledge and address the emotional aspect of your condition to maintain good mental health. Here are some strategies to consider:
- Seek emotional support: Connect with friends, family, or support groups who understand your experiences and can provide a listening ear or offer advice.
- Practice stress management techniques: Engaging in activities such as deep breathing exercises, meditation, practicing mindfulness, or engaging in hobbies that bring you joy can help reduce stress and promote relaxation.
- Set realistic expectations: Be kind to yourself and understand that managing Crohn’s disease takes time and effort. Set realistic expectations and celebrate small victories along the way.
Seeking Professional Mental Health Support
If you find that your emotional well-being is significantly impacted by your condition, it can be beneficial to seek professional mental health support. Mental health professionals, such as therapists or counselors, can provide valuable guidance and support in navigating the challenges associated with living with Crohn’s disease.
Medication and Treatment Options
Common Medications for Crohn’s Disease
Medication plays a crucial role in managing Crohn’s disease and reducing inflammation in the digestive tract. Depending on the severity and location of your condition, your healthcare provider may prescribe medications such as:
- Aminosalicylates: These medications are often used to control inflammation and treat mild to moderate symptoms.
- Corticosteroids: Corticosteroids help reduce inflammation and can be particularly beneficial during flare-ups. However, they are typically used for short-term relief due to potential side effects.
- Immunomodulators: These medications help regulate the immune system’s response and are often used to maintain remission and reduce the need for corticosteroids.
- Biologics: Biologic medications target specific proteins in the immune system to reduce inflammation. They are typically reserved for individuals with moderate to severe Crohn’s disease who do not respond to other treatments.
Understanding Side Effects and Risks
It’s essential to be aware of the potential side effects and risks associated with the medications prescribed for Crohn’s disease. While each medication carries its own set of risks, your healthcare provider will closely monitor your treatment and make adjustments as necessary to mitigate any potential complications.
When to Seek Medical Attention
Regular communication and follow-up with your healthcare provider is crucial in effectively managing Crohn’s disease. It’s important to reach out to your healthcare provider if you experience:
- Severe abdominal pain: Intense and prolonged abdominal pain may indicate a complication or flare-up that requires immediate medical attention.
- Persistent diarrhea or bleeding: If you experience persistent or severe diarrhea or notice blood in your stool, it’s important to consult your healthcare provider.
- Unexplained weight loss: Significant and unintentional weight loss may indicate a worsening of your condition and should be discussed with your healthcare provider.
Building a Support Network
Communicating with Family and Friends
Open and honest communication with your family and friends about your condition can help them better understand your needs and provide the necessary support. Share information about Crohn’s disease with your loved ones, and let them know how they can assist you during flare-ups or times of need.
Joining Support Groups
Support groups can be an invaluable resource for individuals with Crohn’s disease. Connecting with others who share similar experiences can provide emotional support, practical advice, and a sense of community. Consider joining local or online support groups to connect with individuals who truly understand what you’re going through.
Leveraging Online Resources and Communities
The internet offers a wealth of resources and communities dedicated to Crohn’s disease. Websites, blogs, and social media platforms can provide up-to-date information, personal stories, and practical tips for managing life with the condition. The CareClinic app also offers an online community where you can connect with others, share experiences, and learn from each other’s self-care journeys.
Creating a Personalized Self-Care Plan
Assessing Your Needs and Goals
Creating a personalized self-care plan starts with understanding your unique needs and goals. Reflect on your current health, daily routines, and challenges you may face. Consider the aspects of self-care that are most important to you and align with your specific circumstances.
Developing a Daily Routine
Establishing a daily routine can help you stay consistent with your self-care practices. Determine the best time for activities such as taking medication, engaging in physical activity, and meal planning. Use the CareClinic app to set reminders and track your progress, ensuring you stay on top of your self-care routine.
Adjusting Your Plan Over Time
It’s essential to remember that self-care is an ongoing process that may require adjustments along the way. As your needs and goals change, make necessary modifications to your self-care plan. Regularly assess your progress and be open to exploring new strategies that may enhance your well-being.
 By incorporating the principles and practices outlined in this comprehensive guide, you can confidently embark on your Crohn’s disease self-care journey. Remember, self-care is not a one-size-fits-all approach, and what works for someone else may not work for you. Be patient, listen to your body, and work closely with your healthcare provider to find the optimal self-care plan that best suits your needs. With a proactive approach and a dedication to your well-being, you can successfully manage Crohn’s disease and lead a fulfilling life.
By incorporating the principles and practices outlined in this comprehensive guide, you can confidently embark on your Crohn’s disease self-care journey. Remember, self-care is not a one-size-fits-all approach, and what works for someone else may not work for you. Be patient, listen to your body, and work closely with your healthcare provider to find the optimal self-care plan that best suits your needs. With a proactive approach and a dedication to your well-being, you can successfully manage Crohn’s disease and lead a fulfilling life.
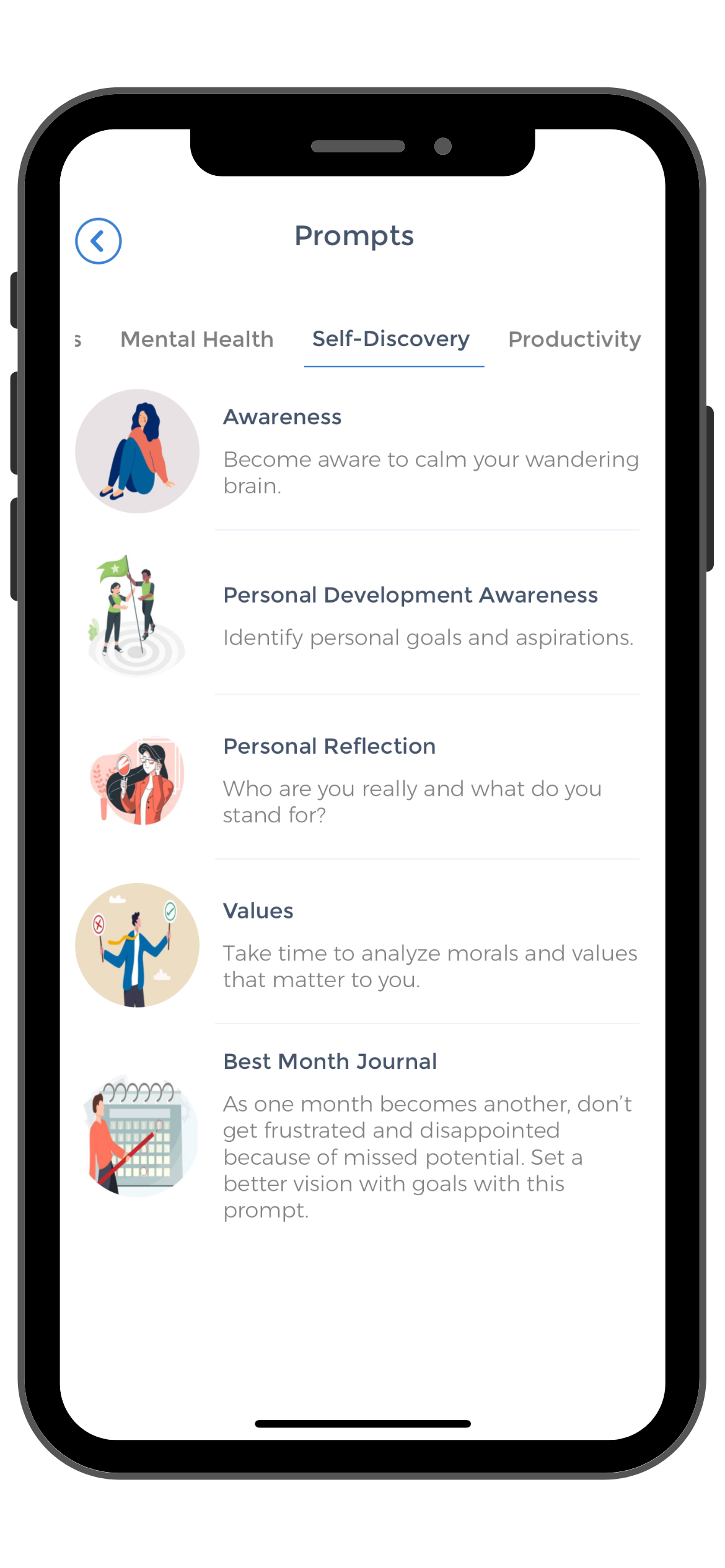
As you continue your journey with Crohn’s disease, the CareClinic app stands as a vital companion for your self-care regimen. With features tailored to track symptoms, monitor medication adherence, and even manage dietary habits, CareClinic empowers you to take control of your health. The app’s symptom tracker allows you to identify patterns and triggers, while the medication reminder ensures you never miss a dose.
With the ability to log your meals, you can pinpoint which foods work best for your body. By consistently using CareClinic, you’re not just managing your condition on a day-to-day basis; you’re building a long-term strategy that adapts to your changing needs, leading to improved health outcomes. Embrace the proactive approach to self-care and discover how CareClinic can transform your management of Crohn’s disease.
Learn more about Self-Care Journaling and how it can support your journey toward a healthier, more fulfilling life.
References
- “Crohn's disease”. https://en.wikipedia.org/wiki/Crohn%27s_disease
- “What to Know About Complementary Treatments for IBD”. https://time.com/6693232/ibd-complementary-treatments/
- “Management of Crohn's disease”. https://en.wikipedia.org/wiki/Management_of_Crohn%27s_disease
- “The Surprising Relationship Between Oral Health and IBD”. https://time.com/7199308/ibd-oral-dental-health-connection/
- “These Environmental Factors Increase the Risk of IBD”. https://time.com/6210633/environmental-risk-factors-ibd/
- “How to Maintain Your Social Life When You Have IBD”. https://time.com/6103888/social-life-ibd/
- “What Should I Eat? | Crohn's & Colitis Foundation”. https://www.crohnscolitisfoundation.org/patientsandcaregivers/diet-and-nutrition/what-should-i-eat
- “Inflammatory bowel disease (IBD): Staying hydrated – AGA GI Patient Center”. https://patient.gastro.org/inflammatory-bowel-disease-ibd-staying-hydrated/
- “Invisible Illness: The Emotional Impact of Crohn's Disease”. https://www.projectcrohns.org/blog/invisible-illness-the-emotional-impact-of-crohns-disease
- “15 Mental Health Tips For People With IBD – National Association For Continence”. https://nafc.org/bhealth-blog/15-mental-health-tips-for-people-with-ibd