Chronic pain, autoimmune conditions, and/or idiopathic diseases can all be debilitating conditions. Often times the symptoms are invisible. Those who suffer from such a disease may feel like they don’t have the support that others with more visible illnesses get. Society’s expectations on what illnesses should look like can leave those who suffer from the aforementioned diseases feeling despondent. Because some illnesses do not present themselves in a visible manner, others aren’t able to immediately sympathize with them. This leaves many in a scenario where they feel like they have to deal with their health condition silently. The best way to understand, sympathize, and acknowledge a person’s reality when dealing with chronic pain and arthritis is to understand what chronic pain does to an individual.
Table of Contents
- Chronic Pain And Mental Health
- Acute Pain vs. Chronic Pain
- What Is It Like To Suffer From Chronic Pain?
- Understanding Arthritis
- Difference Between Osteoarthritis and Rheumatoid Arthritis
- The Difference To Look Out For When Comparing RA and OA
- Arthritis, Chronic Pain, And Mental Health
- How To Prevent Arthritis
- 3 Things You Can Do Now To Manage Your Arthritis
- CareClinic A Free App To Track And Manage Your Pain
Chronic Pain And Mental Health
Suffering in silence is a huge factor that plays into the comorbidity of chronic pain and mental health conditions. Research has shown that there is a strong relationship between mental illness and chronic pain (R). Often times one can lead to another. A decline in mental health may lead to psychosomatic symptoms or suffering from chronic pain. Pain has the potential for limiting what one can do physically. It may lead to the eventual outcome of chipping away at an individual’s confidence.
The relationship between chronic pain and mental health extends further into the biopsychosocial realm. There are also factors that perpetuate pain and mental health conditions such as poverty, unemployment, and social isolation.
Acute Pain vs. Chronic Pain
Acute pain and chronic pain are different responses that the body manifests.
Acute pain is something that is normal and occurs as a function of the body’s healing mechanism. We experience acute pain because, without it, we may reinjure or further provoke an existing injury. What that means is that when we hurt ourselves the body needs a response mechanism. This mechanism tells our brain that we cannot push ourselves to continue a certain activity. It would be detrimental to the stage of healing. The last thing we want and the body does not need is to heal poorly.
Chronic pain on the other hand is a malfunction of our nervous system. Not that our nervous system has done something wrong. All the nervous system has done is the preservation of a pain pathway. The process of moving from acute pain to chronic pain is within the realm the human body’s greatest functionality: adaptation.
Chronic Pain And Its Neural Pathway
So what exactly is happening with our nervous system when it comes to chronic pain? Without getting too deep into the science of it all, we must understand two things about our nervous system.
In order to make sense of chronic pain here is what happens:
- Our nervous system functions by creating a pathway-like network that connects from the brain to the area of pain
- The more a pathway is used, the more likely the brain will remember the pathway
From these two facts, we can conclude this: if you are experiencing an injury physically or even mentally, and this injury is recurring or the injury was so great that recovery took a long time, the pathway that signals the pain associated with the injury will be utilized often. Like a hiking trail, the more the trail is hiked, the more visible the trail path becomes.
So chronic pain works like this: our body remembered the pain associated with an injury from a long time ago – but the injury has been healed. However, during the injury the pain pathway was signaled often, leading to the nervous system to think it was a good idea to keep the pathway around. It served an important function at the time, so it might continue to serve an important function.
What Is It Like To Suffer From Chronic Pain?
Anxiety, depression, low energy, lethargy, and lack of motivation – are some of the psychological manifestations that plague those with chronic pain. Remember, even though you may not be able to see the state of pain that people are in, does not mean that they are not suffering. Be nice to everyone, because you never know what they are living with, where they are coming from, or what they have been dealing with!
That said, we should also be cognizant not to be overly cautious or interact in a coddling way, it can be perceived as demeaning – people with chronic pain are humans too. Everybody desires to be treated as equals. It’s very possible that a person you know who is dealing with anxiety, depression, or low energy because of chronic pain is taking a measured approach to handling their mental health!
For those that do not have to deal with chronic pain, here is one thing that can help us empathize with those that do: pain becomes a factor that is the limiter to their lives. Symptoms of pain can become the governor of how one navigates their life – which ultimately affects the quality of life. When recording your pain consider using the wong baker faces scale.
So what does chronic pain do to a person? Often there is a battle with the mind to stave off feelings of frustration and negative thoughts. The propensity for those struggling with chronic pain has a steeper uphill climb when it comes to overcoming self-esteem issues, creating a positive sense of self-worth, and maintaining healthy emotions.
Understanding Arthritis
Arthritis is a disease that affects the health of your joints. At its most basic form, it is the inflammation of joints. A joint is where two different bones meet. Depending on which joint you are examining in the body, there are fluids called synovial fluid cartilage, meniscus, or vertebral discs that protect the bone surfaces sharing a joint from rubbing up against one another.
When inflammation happens in a joint space, pain develops, the range of motion within said joint diminishes, and visible swelling and redness can occur on the surface. In totality, a person will have limited movement, and daily tasks may become harder to accomplish.
So what exactly is inflammation? In order to fully appreciate what arthritis is and to acknowledge the full effects of the condition, we need to understand inflammation first.
Simply put, inflammation is the body’s response to healing. Inflammatory markers rush in when an area in your body is damaged in order to promote 5 things to occur: redness, swelling, heat, pain, and loss of function (R). This alerts you to know that an area in your body is not fully functional and it might be a smart idea to remain cognizant in not demanding too much from that area in your body until the healing process can complete. That said, arthritis is tricky because the healing process with this condition does not end. It’s a perpetual battle for those who suffer from the condition.
Arthritis can vary, in fact, there are more than 100 different types of it. The two most common forms of arthritis that is heard of is osteoarthritis and rheumatoid arthritis.
Difference Between Osteoarthritis and Rheumatoid Arthritis
Although the symptoms presented are quite similar between osteoarthritis and rheumatoid arthritis, the way the conditions are developed within the body is very different.
Osteoarthritis (OA)
With osteoarthritis, the condition occurs when the cartilage between two bones that share a joint wear out. When this happens, the two bones start to rub up against each other. Since the surfaces are hard, irritation begins to happen, leading to some pain. When this goes on for a longer period of time, inflammation happens.
Rheumatoid Arthritis (RA)
When considering RA, the biggest differential is that it is an autoimmune disease. There is a systemic factor to it, which means this differential leads to a whole list of other complications that those who suffer from OA do not need to deal with. These complications may include but are not limited to a net negative impact on organ function, skin problems, eye problems, and cardiovascular problems.
In a nutshell, RA being an autoimmune disease means that the individual’s own immune system is attacking the body. In the case of joint pain, the structures around the joints are attacked. These structures serve to protect the bones sharing the joint from rubbing up against one another. When these structures start to break down, the healing process releases chemicals that affect the structures around it (in this case the bone of the joint as well as the cartilage), which breaks those surfaces down as well.
The Difference To Look Out For When Comparing RA and OA
The biggest factor that healthcare professionals look out for in order to rule out rheumatoid arthritis when somebody is experiencing joint pain or inflammation within the joint is age factor.
If you are experiencing new pain within a joint that has been an ongoing issue and you are over 50, chances are you have osteoarthritis and not rheumatoid. This is important to note because osteoarthritis is actually quite common in those who are older! It is just a common manifestation of wear and tears over a long period of time coupled with the human body’s diminishing ability to repair fast enough.
A General Rule Of Thumb
Osteoarthritis occurs in a single joint first, before the integrity of your skeletal system diminishes due to overcompensation. From there other joints that need to take the brunt of the work in order to make up for the weaker joint will eventually also experience faster wear and tear leading to osteoarthritis in a new joint.
That said if your symptoms of joint pain occur in a symmetrical manner like you are experiencing joint pain on both sides of the same part of your body (such as left and right hand, both knees), you may have rheumatoid arthritis and you should seek medical attention as soon as possible.
Arthritis, Chronic Pain, And Mental Health
As mentioned earlier, chronic pain conditions are often invisible at first glance. Common chronic pain conditions include arthritis, fibromyalgia, multiple sclerosis, back/neck pain, and migraines (R). Unless you spend some time observing the movements of an individual for a longer period of time, it may go unnoticed. Even for professionals, it may be difficult. Those who are trained to work with people suffering from the aforementioned conditions can hide their symptoms well. Depending on the individual, if they have been dealing with their condition for long enough, they may have adapted coping mechanisms that allow them to lead predominantly functional lives.
Because of the invisibility of these conditions, it is helpful to know the science behind the comorbidity of chronic conditions and mental health. Taking arthritis as an example, those who suffer from it, have a notable risk in developing mood and anxiety disorders.
Joints function as a way to allow for movement to happen. When an individual newly develops arthritis, there will be a learning curve to adjust for their condition. The pain may stop them from doing activities they are used to doing – which can effect their mental health on the short term.
How To Prevent Arthritis
Prevention and intervention are two great measures to control for condition and symptomatic outcomes when dealing with arthritis. For the most part, because arthritis is an inflammation-based disease, a helpful way to avoid exacerbating the symptoms is by controlling for what you can: namely lifestyle habits, exercise, food intake, and weight fluctuation.
In order to take preventative measures to avoid developing arthritis, it is important to do these things:
- Maintain an active and healthy lifestyle
- Control your weight to avoid high demand and overuse, wear and tear of your joints – use this weight loss tracker template
- Eat foods that are high in collagen
- Be aware of your joint health, if you feel like something is off, let your body rest
- Stretch and strengthen your muscles
- Hire a fitness coach to learn how to do exercises optimally
- Postural assessment done by a professional
Already have arthritis? Here are some great ways to manage your symptoms so the condition does progress faster than it needs to.
- Wear a brace to support your joint
- Avoid strenuous activities that create an environment for high impact on your joints
- Strengthen the muscles around the joint experiencing pain
- See a Registered Dietician or Nutritionist for advice on foods that are anti-inflammatory
- A Physiotherapist can help with preventative rehabilitation
- See a Massage Therapist that is licensed (RMT or LMT) to help manage your muscle pain around the joint
University of Washington Orthopedics and Sports Medicine put together an extensive list of things to do in order to cope with arthritic symptoms (R).
3 Things You Can Do Now To Manage Your Arthritis
It is important that you take the initiative to manage your arthritic condition. Pain management can be very successful if you have a good team of health care providers. Not only will they provide mental support, they will also update you on the newest trends and methods to help manage your condition. On top of that, there are lots of tools out there that can help you manage your chronic pain!
Here are 3 things that you can do to manage your arthritis:
1) Change Your Diet
As stated earlier, arthritis is an inflammation-based disease – this means that if levels of inflammatory markers are high in your blood, chances are that the symptoms of arthritis will be more pronounced.
Food is a great place to start in order to control for how prone your body is to develop an inflammatory state. Although Voltaren is a great drug to use for immediate pain relief, it will only mask the pain temporarily. On the long run, the dividends you get from being selective with your food intake will go a long way.
Foods that are inflammatory include:
- Fried foods
- Refined carbohydrates
- Refined sugars
- Processed meats
- Foods with sulfites
In addition to avoiding the aforementioned foods, it’s also a great idea to eat a lot of foods that have anti-inflammatory affects! These include:
- Turmeric (best taken with fats either cooked or had coconut oil in tea)
- Vegetables and dark leafy greens
- Berries
- Green teas
- Fish high in omega-3 fatty acids such as salmon or sardines
- Good quality olive oils
Overall, the best rule of thumb is to eat wholesome, nutrient dense foods. Avoid having a heavy intake of overly refined and processed foods.
2) Get A Massage
If you are in a lot of pain, chances are you have been compensating in your movements, which leads to further pain, which leads to further pressure on your joints when you have to move. This positive feedback loop happens, and the healing process can take longer.
Seeing a Registered or Licensed Massage Therapist can go a long way. They have been trained in helping to manage with pain. Although you cannot massage your arthritis away, you can mitigate your symptoms of pain.
It’s very plausible that the swelling and inflammation caused by the irritation in your arthritic joint has lead to muscle soreness in the surroundings. Getting a massage can help to reduce muscle soreness and pain.
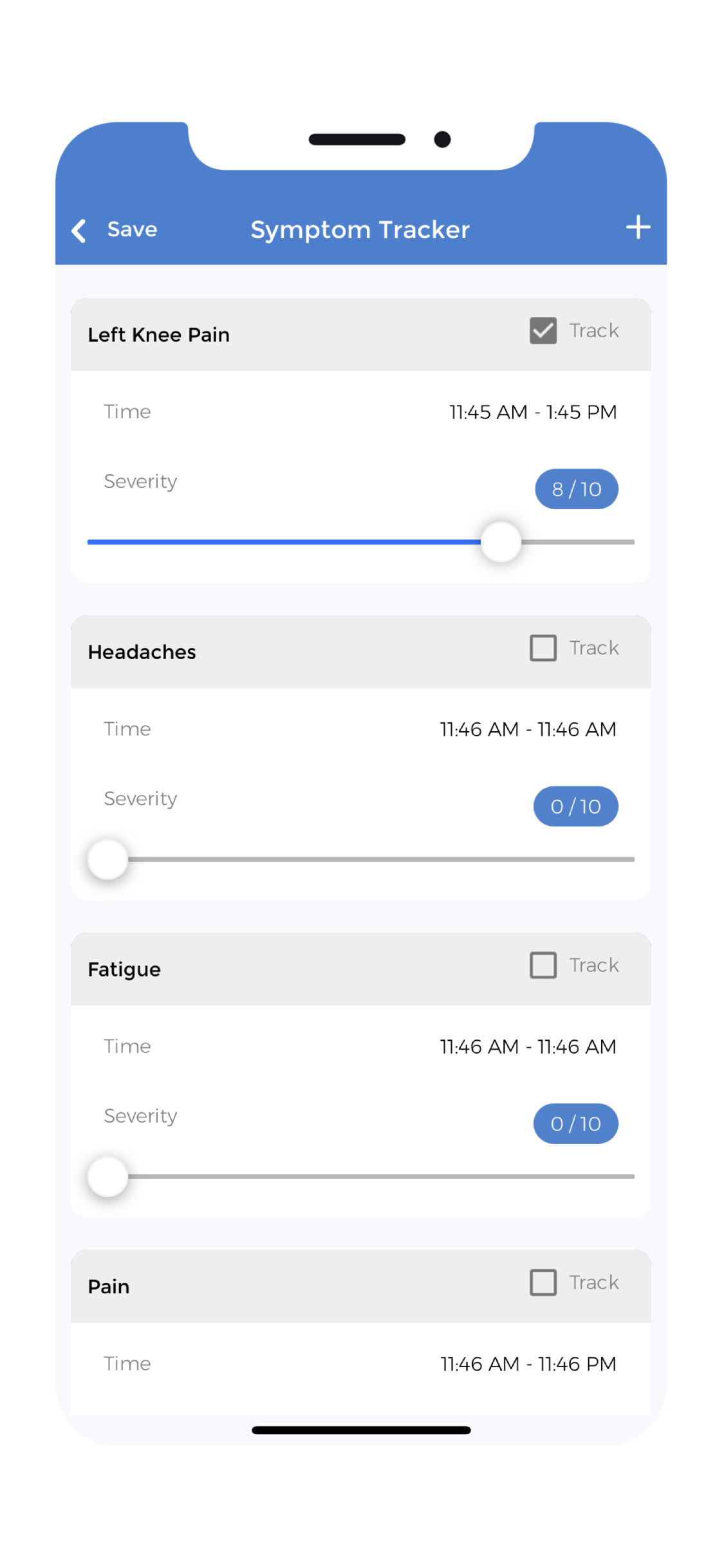 3) Track Your Pain
3) Track Your Pain
Tracking your pain whether its written down or done through an app will give you an edge. As you start the habit of taking notes on the frequency and pattern of your pain, you may find some overlooked details about your condition. This will allow you to take preventative measures before the pain happens.
CareClinic A Free App To Track And Manage Your Pain
The advent of technologies such as CareClinic’s health management platform can assist patients in bettering their chances of successfully managing their pain in a more efficient manner.
The CareClinic app delivers the pinnacle of convenience, as an all-in-one health management application that delivers health solutions right through one’s phone. The simple-to-use app has easily navigated functionalities designed to suit everybody’s needs.
CareClinic’s all-in-one health management app can help track, manage and improve health outcomes for people dealing with either acute or chronic pain. The easy-to-use functionality allows for you to track pain daily.
The simple-to-use measurement input methods allow for patients to easily check-in with the app daily. Their care team is also able to communicate with you through the app. This way doctors can be notified and kept up to date on their patients 24/7.
You are also able to keep track of how are feeling day to day, trace the source of your pain better through using the app.
Here’s a quick video about pain and pain management techniques when living with chronic pain: