Migraines are way more than just a bad headache. A bad migraine can leave you feeling useless and in bed for days. In fact, studies have shown that migraines are the 6th most disabling disease in the world1. So, the next time someone tells you “It’s just a migraine”, find comfort in the fact that there are literal scientific studies proving them wrong. And remember that you’re not alone! More than 10% of the global population suffers from migraines – that’s at least 800 million people1!
Fortunately, there are plenty of migraine treatments available both over the counter and by prescription. While these usually do the trick, some who suffer from more severe and excruciating migraines may find the results from these drugs to be… lackluster. In these cases, physicians actually turn towards a class of immunosuppressant medications called corticosteroids. One of the most popular corticosteroids is indeed prednisone. However, despite the rapid benefits this medication can reap, prednisone does come with a long list of possible side effects and complications that must be considered. Find out how using CareClinic is a great way to determine – along with your physician – if prednisone for migraines is a good treatment plan for you.[1][2][3]
What is a Migraine and Migraine Aura?
The way I’ve always described migraines to my friends is as a headache but make it 10x more intense. Clinically speaking, migraines are defined as typically throbbing, unilateral, severe headaches with associated symptoms such as sensitivity to light, sounds, and nausea1. Migraines often appear in recurrent patterns. There are many triggers and symptoms pre-attack that can help you predict and prepare yourself beforehand.
For example, as migraines begin in the brain, many patients state that they have difficulties with speech, reading and hearing, increased emotionality and sensory hypersensitivity preceding their attacks1. About 15 to 20% of individuals who suffer from migraines experience this group of warning signals commonly referred to as an aura2. Moreover, while an aura does typically show its face before a migraine, it may instead set in during or even after the attack and can last anywhere from 10 minutes to an hour2.
How early these symptoms appear before the attack is hard to say. For some, it may be an hour before the migraine sets in, for others, maybe 121. Similarly, once the throbbing sets in, it may not let up for days, while other attacks might only last an hour1.
Types of Migraines
Maybe you’ve never actually experienced an aura with your migraines. Does that mean what you seemed to think was a migraine isn’t actually one? Nope! In fact, there are many different types of migraines, each with its own characteristics. Some of these migraine types include:
- Migraine with aura (also known as a complicated migraine)2
- Migraine without aura (common migraine: Think the symptoms without the warning aura
- “Silent migraine” or “acephalgic migraine”: The opposite! The aura, without the following headache2
- Hemiplegic migraine: This type of migraine is accompanied by temporary paralysis, neurological or sensory changes on one side of your body, with or without head pain2
- Retinal migraine (ocular migraine): These migraines generally begin as a dull ache behind your eye that is followed by temporary loss of vision in one of your eyes2
- Chronic migraine: These migraines occur for at least 15 days per month. Each migraine attack may vary in severity and symptoms2
- Migraine with brainstem aura: Vertigo, slurred speech, double vision, and loss of balance all commonly occur before the headache sets in with this migraine. These symptoms usually occur suddenly and can be associated with speech difficulties, vomiting and ringing in the ears2
- Status migrainosus: This is a rare, severe migraine that can last longer than 72 hours. Head pain and nausea especially in this headache are often incredibly painful2
Migraine Triggers and Risk Factors
Like most diseases and disorders, it’s difficult to pinpoint exactly who is going to develop migraines and who isn’t. Regardless, there are some triggers and risk factors that can make you more vulnerable2.
Some of these triggers include:
- Emotional Distress: In a stressful event, your body responds by releasing chemicals that push your body into its flight or fight response. These chemicals often have implications for the brain and can bring about a migraine. Additionally, strong emotions such as anxiety and excitement can cause an increase in muscle tension and dilation of your blood vessels. This response can make your migraine much more severe2.
- Your Eating Patterns and Caffeine Consumption: Missing a meal deprives your body of the nutrients it needs. Many people find that skipping a meal, though it may feel harmless at first, can be a migraine headache trigger. Additionally, the abrupt drop in caffeine levels during withdrawal or a large coffee can also cause severe headaches and even migraines2.
- Light: For many who experience repetitive migraine attacks light can be a major trigger. Try avoiding flashing lights, fluorescent lighting, TV, and computer light, as well as significantly bright sunlight if you suffer from migraines2.
- Hormonal Changes in Women: The abrupt drop of estrogen during a menstrual cycle can trigger migraines. This could be the reason why your migraines seem to appear more frequently during and around the time of your period2.
Risk factors for migraines include:
- Genetics: Studies have shown that up to 80% of people who get migraines have a direct relative who also does. This suggests that there is a genetic component2.
- Gender: Due to fluctuating hormones during a women’s reproductive ages (15 to 55), migraine headaches do appear more prevalent in women s compared to men2.
- Stress Level: We’ve already briefly touched on stress as a trigger, and thus it makes perfect sense that constant high amounts of stress put you at an increased risk of developing migraines2
- Smoking: Studies have shown a correlation between smoking and migraine onset, suggesting smoking status as a risk factor2.
Migraine Symptoms
In general, migraines can come with a long list of potential symptoms. These symptoms can go on to further vary greatly between individuals. Nevertheless, the very core of a migraine is a headache2. This pain is characteristic of migraine and generally feels like dull to pulsing pounding or throbbing, in most cases, only on one side of the head. Sometimes this pain can spread, with anecdotal reports of pain around the eye, in the sinus, jaw or neck2.
Other Symptoms include:
- Sensitivity to light, noise, and odors2
- Nausea, vomiting, stomach and abdominal pain2
- Loss of appetite2
- Sweating or chills2
- Pale skin2
- Fatigue2
- Dizziness and blurred vision2
- Tender scalp2
- In rare cases: diarrhea and fever2

Moreover, it is always important to note that you may not experience every one of these symptoms. Or maybe you’ll experience symptoms not even included in this list. Your experience with a migraine won’t always look like the norm and that’s okay. It is always recommended to visit a physician if you suspect you suffer from migraines.
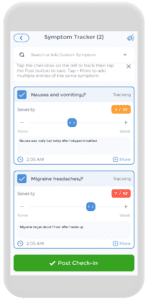
In fact, keeping a symptom tracker on a comprehensive health app, such as CareClinic, can help your physician come to your diagnosis faster and with more confidence! The symptom tracker is an easy-to-use built-in tool on the app that allows you to record the time you experience your symptoms and make note of a specific trigger you may have noticed along with symptom intensity. Over time, you can use the chart feature to recognize patterns in your migraine symptoms to identify triggers to eliminate in order to help you feel your best at all times!
Headaches Treatments
Nonsteroidal Anti-Inflammatory Drugs: Also known as NSAIDS, this is a class of drugs you’re probably already very familiar with. NSAIDs are a therapeutic drug class that is known to reduce pain and decrease inflammation and fever, without being a steroid. Although you may not have heard the term NSAIDs before, chances are you already have some in your medicine cabinet right now! NSAIDs include ibuprofen (better known by the brand name, Advil), and naproxen (or Aleve). These drugs appear consistently effective for migraines in clinical studies and are often the first treatment approach you’ll reach for during a migraine attack3.
Acetaminophen: This is another popular medication often used by patients are the beginning of a migraine – Tylenol! Tylenol does appear to have some implications in pain and headaches treatment3. Due to its widespread and low-cost availability, acetaminophen is a great choice to treat minor migraines. However, there is currently no evidence to suggest that the drug is significantly beneficial in reducing migraine symptoms3.
Triptans: Triptans are essentially small molecules that competitively bind to the serotonin receptors on your neurons4. As a result, the blood vessels we previously said were dilating in a migraine, instead constrict4. Accordingly, this is thought to help relieve the migraine. Overall, this function enforces the role of triptans as an antimigraine agent, however, there are studies showing the therapy is not as effective in prolonged and severe migraine 3,4. Additionally, it is always important to consider the side effects of any medication. Triptans are often associated with dizziness and prickling sensations3.[4][5]
Steroids for Migraines
So far, we’ve talked about typical, first-line treatments for relatively mild and short/acute migraines. You’ve probably noticed that most medications we have discussed often show little to no improvement when it comes to prolonged and more serious cases of migraines. So what headache treatment is available for people who suffer from these debilitating and painful attacks?
What are Corticosteroids?
For some, the answer might be using a generally stronger medication, like a form of steroid. Corticosteroids are one of the most prescribed forms of steroids used to treat inflammation and rheumatologic diseases5. One of its lesser-known uses is as a treatment for intractable and rebounding migraines6. So, what exactly are corticosteroids?
Simply put, corticosteroids are molecules that closely resemble cortisol5,7. Cortisol is your body’s primary stress hormone and is produced by your adrenal glands. Due to the structural similarities, corticosteroids work by binding to cortisol receptors in your body to induce certain physiological effects. One such effect: is the suppression of inflammation7.
Some commonly used corticosteroids include cortisone, methylprednisone and the shining star of our topic today: prednisone7.
Prednisone: Uses, Mechanisms & Side Effects
Prednisone is most commonly used to treat rheumatologic diseases7. A rheumatologic disease is one that is marked by inflammation and pain in the joints, muscles, and ligaments throughout your body. Biologically speaking, prednisone enters of cells and halts the production and function of proinflammatory signals. This, in turn, stops the recruitment of immune cells involved in inflammation and effectively decreases many of the corresponding symptoms7.
Overall, prednisone appears to be a great treatment! Its possible uses are widespread as an immunosuppressor, and it comes with great benefits. But if we’ve learned anything by now, it’s that researching and understanding the adverse side of medication is always important. Moreover, the side effects of prednisone can also vary depending on the method you are consuming it by8. For oral prednisone, some side effects include:
- Fluid retention in the lower legs8
- Increased blood pressure (download a printable blood pressure and pulse chart here) 8
- Abdominal aches and bloating8
- And weight gain8
Inhaled, topical or injected prednisone exhibits slightly different side effects, including:
- Thinning of the skin8
- Pale skin colour8
- Facial flushing8
- Insomnia8
- Increased blood sugar8
In rare cases, long-term use of prednisone can contribute to much more serious effects, such as:
- Increased pressure in the eyes8
- Cataracts8
- Thinning of the bones8
- Suppressed hormone production by the kidneys8
Nevertheless, despite these risks, many people do use prednisone as in most cases, the benefits outweigh the risks! In a choice between the possible side effects or painful current symptoms, prednisone usage does win. As with most medications, these possible side effects are simply a necessary evil for the greater good.
Prednisone Headache Treatment
If a migraine doesn’t let up for 72 hours, corticosteroids are a common therapy to help alleviate symptoms9. That being said, it is important to note that very little is known on the use of these immunosuppressant drugs in migraine treatment. In fact, these agents are never used as a preventative measure – more than likely due to the side effects we just discussed – and instead are only used in severe situations as a short-term treatment9.
Some of these severe situations in which corticosteroids are already used, besides severe and prolonged attacks, include drug-overdose headaches and immunosuppressant-induced headaches following organ transplantation9. As I’m sure you’ve gathered, these situations are harsh, to say the least, and require strong, effective treatment. Hence, prednisone for migraines makes the perfect treatment.
Why does using Prednisone for Migraines Help?
As I’ve said before, very little is actually known about using prednisone and other steroid treatment for migraines9. What I can tell you, is that the general guess involves neurogenic inflammation suppression. After the migraine system in your brain sort of turns on, inflammation in the brain does as well and can continue for many days9. This is dangerous.
Fortunately, steroids seem to do their best work in this stage9. Administering prednisone can suppress this inflammation and thus, reduce and calm some of the aggressive migraine symptoms you may be experiencing. In fact, we’ve been using corticosteroids for migraines since before we even knew how migraines set in9.
General Prednisone Headache Treatment Plan
To achieve prednisone headache relief, the amount of corticosteroid prescribed to you can vary depending on how you respond. You may have previously used prednisone for a tension headache and know it didn’t really help. In this case, the drug likely isn’t the best choice for you. Or maybe the drug completely got rid of the tension headache altogether. The moral I’m trying to get across to you is that many people experience varying degrees of success when it comes to prednisone and headaches6. Unfortunately, there is no one-size fits for prednisone headache relief. Nevertheless, there are starting doses many physicians will prescribe in your prednisone headache treatment.
The general practice seems to recommend doses of 100 mg daily for 10 days with a -10mg decrease per day when prescribing prednisone headache relief10. Thus, when it comes to migraines, this is a great place to start in your treatment plan!

Track the Side Effects of Prednisone for Migraines using the CareClinic App
Once you start taking prednisone, it can be beneficial to track your doses and when you take them. This can help you quickly recognize patterns associated with your treatment and tailor it to best suit your needs. Furthermore, the CareClinic app does come with a built-in medication tracker as a one-stop show for all your tracking needs!
Using the app makes this process easy, accessible, and fast, all while having additional features to provide the most comprehensive overview possible. A notes section is included in every check-in you post as a place for you to add any notes you may deem important. And of course, the time, and dosage are always included in every check-in. In this way, CareClinic helps you stay one step ahead of any adverse prednisone side effects! Not in the mood to use an App? Fear not, there is also a printable headache log we have created that you can download from here.[6][7][8]
Using CareClinic to Determine if Prednisone for Migraines is Right for YOU
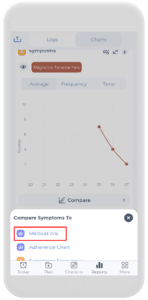
I know considering prednisone can be a little scary. The adverse effects can be severe if not properly monitored. Fortunately, CareClinic offers you all you need to make an informed and personalized decision that best fits your needs! The app allows you to not only track your medications and symptoms but also to compare them using a variety of analysis features available right at your fingertips. The correlation charts are a perfect way to help you notice trends visually with just one glance.
If you and your physician decide not to use medication to treat your migraines – do not worry, CareClinic is still here to help you out! Make use of the app’s nutrition and water trackers to make sure you’re always avoiding your migraine triggers and putting what’s best for you into your body! Additionally, if you find that stress is a major catalyst for migraines in your life, try the CareClinic diary feature as a journal to help log your emotions and day. This can hopefully help you identify stress points in your life and take steps towards reducing them! The App comes built-in with over a dozen journal prompts for mental health that you can start to use right away by tapping “Prompts” from the top right-hand side of the Diary screen.
Overall, the CareClinic app is here to be whatever you need it to be. The health tracker is always available for use and makes gaining a comprehensive picture of your health easier than ever before!
References
- Pietrobon, D., & Moskowitz, M. A. (2012). Pathophysiology of Migraine. Annual Review of Physiology, 75(1). https://doi.org/10.1146/annurev-physiol-030212-183717
- Cleveland Clinic. (2021, March 03). Migraine Headaches. Retrieved from: https://my.clevelandclinic.org/health/diseases/5005-migraine-headaches
- Gupta, S., Oosthuizen, R., & Pulfrey, S. (2014). Treatment of acute migraine in the
emergency department. Canadian Family Physician, 60(1),47-49. https://https://www.cfp.ca/content/60/1/47.short - & Nicolas, D.
- Cleveland Clinic. (2020, January 20). Corticosteroids. Retrieved from: https://my.clevelandclinic.org/health/drugs/4812-corticosteroids
- Roberts-Zibbel, E. (2017, March 21). The Catch-All Treatment: Prednisone. Migraine.com. Retrieved from: https://migraine.com/living-migraine/the-catch-all-treatment-prednisone
- , , &
- Mayo Clinic. (2020, December 16). Prednisone and other corticosteroids. Retrieved from: https://www.mayoclinic.org/steroids/art-20045692
- Rozen, T. D. (2002). Migraine headache: Immunosuppressant therapy. Current Treatment Options in Neurology, 4(5), 395–401. https://doi.org/10.1007/s11940-002-0050-0
- Mauskop, A. (2012, June 11). Steroids for migraines. Headache NewsBlog. Retrieved from: https://www.nyheadache.com/blog/steroids-for-migraines/
References
- “Migraine is the most disabling neurological disease among children and adolescents, and second after stroke among adults: A call to action – PubMed”. https://pubmed.ncbi.nlm.nih.gov/39197864/
- “Steroids for preventing recurrence of acute severe migraine headaches: a meta-analysis – PubMed”. https://pubmed.ncbi.nlm.nih.gov/23577697/
- “Prednisone”. https://en.wikipedia.org/wiki/Prednisone
- “Migraine | National Institute of Neurological Disorders and Stroke”. https://www.ninds.nih.gov/health-information/disorders/migraine
- “Migraine Aura: What Is It, Symptoms, Causes & Treatments”. https://my.clevelandclinic.org/health/diseases/22131-migraine-aura
- “Migraine Headache: Immunosuppressant Therapy – PubMed”. https://pubmed.ncbi.nlm.nih.gov/12162928/
- “The place of corticosteroids in migraine attack management: A 65-year systematic review with pooled analysis and critical appraisal”. https://pubmed.ncbi.nlm.nih.gov/25576463/
- “Prednisone for migraines: Efficacy and dosage”. https://www.singlecare.com/blog/prednisone-for-migraine/