First of all, let’s get all the giggles out. A poop tracker. Understandably, healthcare professionals will rarely say the word “poop”. It will mostly be referred to as stool or feces. However, for babies/parents/kids/adults all alike, the word “poop” will be used. Let’s face it; it is way more realistic and slightly more humorous. Who does not enjoy a little laugh these days? Let’s lighten up! So…go ahead. Laugh! Poop!!!!!
All jokes aside, the discussion on how to digitalize a poop tracker for IBS will be mentioned, and how the CareClinic platform will help with this achievement. Keeping track of the symptoms, how to keep a poop diary or a poop log, incorporating an elimination diet and so much more.
Keeping a poop tracker for IBS will be critical for prognosis. Whatever you want to call it: A poop tracker, a poop tracking app, a poop app, a poo app, or a pooping app…The journey to relief begins now.
How to Use the Poop app/Poo app/Pooping App
This section will provide a step by step instructions on how to enable or start the poop tracking! Your very own poop tracker!
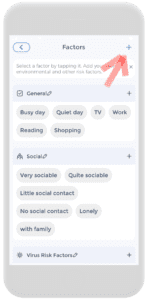
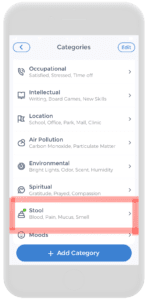
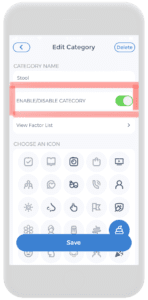
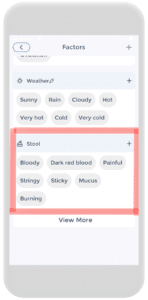
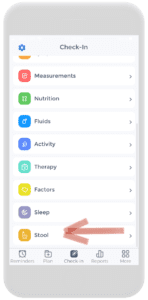
Firstly, on the check-in page, click on Factors. From there, add the stool category by clicking on the plus button. Then scroll down the category list until “stool” is found. Click on it and enable the category. Once that is complete, the stool category will appear on the factors page.
Afterward, from here on out, the “stool category” will appear in the daily check-in. From here, reports, charts, records, and stool insights will appear through the CareClinic platform. This will be discussed in the next section.
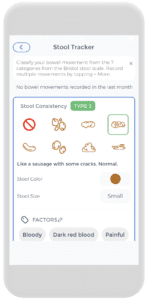
Once the stool tracker is ready to launch from the CareClinic Platform, whenever a poop occurs, it can be tracked there directly. Anywhere and anytime! The official stool tracker page will look like the illustration on the left.
It allows the tracking of all seven types of poop (please refer below to the Bristol Poop Charting) as well as an indication of color, volume, size, and all of its associated factors (such as bloody, pain, bad odour, etc.)
Using the CareClinic Poop tracker, having a poop log, a poop diary or a poop calendar (whichever the term wished to use can be used) has become extremely easier and more convenient. Begin your poop tracking journey today!
Reporting, Chart & Stool Insights
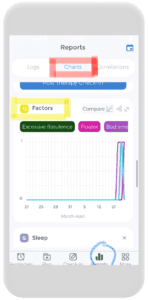
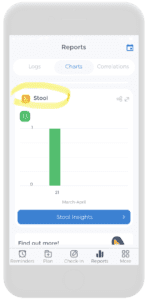
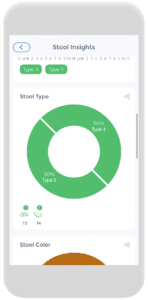
Once the stool tracker is established, the possibilities on the CareClinic Platform are endless. Reports can be checked by clicking on the “reports button” on the bottom (circled in blue in the first picture on the left). From there, charts from the factors and stool section are present.
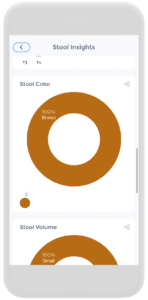
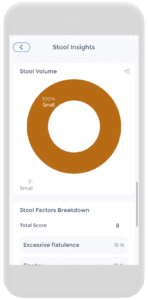
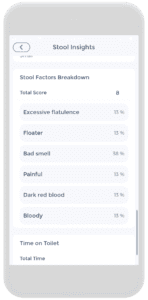
The second picture from the left illustrates a blue button that says “Stool Insights” which will yield pictures from the remaining four illustrations. These stool insights provide…insight! Go figure!!! It shows you the Bristol stool types, color, volume, and stool factor breakdowns throughout a time interval.
All of this is conveniently in one platform- a new, enhanced digital approach for a personalized poop workbook. The poop workbook of what IBS dreams are made of.
Quick Review of IBS
What is IBS?
Irritable bowel syndrome (IBS) is a chronic and debilitating gastrointestinal disorder that affects about 9%-23% of the population across the world (7). This statistic makes IBS one of the most commonly diagnosed gastrointestinal diseases. IBS is defined as the “presence of abdominal pain or discomfort with altered bowel habits”. This abdominal pain must have the absence of any other detectable structural and biochemical abnormalities. Which strictly means that there is no other diagnosis that will explain this discomfort or pain (6).
IBS Symptoms
For example, IBS symptoms typically consist of abdominal pain or discomfort, altered pooping habits such as constipation, diarrhea, or both. Other symptoms can include: bloating, distention, symptoms brought on by food intake, a change in pain location, and stool pattern over time.
IBS Diagnosis
A licensed physician is the only person who will diagnose IBS. In addition, a “Rome Criteria” has been developed that is used to diagnose IBS. The first edition was published in 1990- however, modifications have been made. Currently, Rome Criteria III (from 2006) is being used.
Rome III criteria state that IBS requires “at least three days a month in the last three months are associated with two or more of the following: improvement in abdominal pain or discomfort with defecation, onset associated with a change in frequency of stool, and/or an onset accompanied by a change in form or appearance of the stool” (6,7).
Bristol Poop Chart
This Bristol Poop Chart was developed as a way to talk about shapes and different types of poop. It is also called the Meyers Scale. However, the Bristol Poop Chart has a nice ring to it…
Imagine going to the doctor’s office and instead of having a method to describe it, you bring a sample with you in a little baggie. That is pretty gross. For this particular reason, the Bristol Poop Chart has made this conversation a lot easier. For example it is important to have this poop discussion with the healthcare team especially regarding monitoring IBS symptoms. Please refer to the chart for further reference (8).
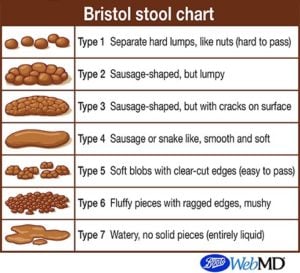
Type 1 Stool
For instance, this stool is similar to the shape of nuts, as they are hard lumps that come out separately. If it is hard to pass, this type of stool usually indicates constipation(8). This type of stool can be used for babies/parents/kids/adults or anyone. Knowing this type of information and recording it on a poop log/poop diary/poop calendar on the poo app/pooping app will be informative to the healthcare team looking after your IBS. Some people suffering from IBS can have predominantly constipated-IBS symptoms.
Type 2 Stool
This stool is lumpy but still collectively together. Also, it appears to have a sausage shape. This type of stool is still considered closer to the constipation side (8).
Type 3 Stool
For example, this stool is also sausage-shaped. On the other hand, this poop has some cracks on its surface (8).
Type 4 Stool
For example, this stool is also sausage-shaped. However, it does not have cracks. It is very smooth and soft. Types 3 and 4 are considered the ‘ideal stools” as they are easily passed (8).
Type 5 Stool
For example, this poop is described as “soft blobs with clear-cut edges” (8).
Type 6 stool
For instance, on the other hand, this stool is mushier and softer than type 5. There will be fluffier pieces with ragged edges (8).
Type 7 Stool
Very watery poop. Types 5-7 lean towards the diarrhea scale. Some IBS patients suffer from diarrhea-prominent IBS (8).
Treatment and Management of IBS
For example, IBS is a “symptom-based disorder, and therefore the treatment goals will be aimed at resolving symptoms such as pain, bloating, cramping, and diarrhea or constipation”. Before discussing treatment options with patients suspected of IBS, the physician will carefully perform a detailed history and physical to exclude other diagnoses with symptoms similar to those of IBS (6,7).
The Elimination Diet
The main reason people try the elimination diet is to identify food triggers. Typical triggers are:
- For example, dairy products (2)
- Gluten-containing foods (wheat, rye, barley) (2)
- Corn (2)
- Soy (2)
- Foods high in FODMAP (2) (will be discussed in the next section)
Keeping a food diary or a food journal will be key in achieving this step. The CareClinic platform can provide not only a personalized poop tracker but also can behave as your personal food diary or food journal. Utilize the platform to become one step closer to achieving IBS-symptom-free lives.
Elimination Diet Phases
Phase 1: This phase will last about two weeks. During this time, all trigger foods (especially high FODMAP foods) will be completely eliminated. Similarly to a cleanse. During the diet’s first phase, it is important to chart the symptoms in the food diary/food journal. If there is a significant reduction in symptoms, it means the elimination diet is working (2).
Phase 2: This is the reintroduction phase. Foods will slowly reintroduce back into the diet, one at a time. Pay close attention to any symptoms and document them in the food diary/food journal. Importantly, after eating a trigger food, it can take up to three days for symptoms to appear (2).
Elimination Diet Cons
Elimination diets are very restrictive. Everyone attempting an elimination diet should work with a licensed dietitian to ensure no harm is done. Children are particularly vulnerable to this type of malnourishment seen in elimination diets (2,4).
Also, while elimination diets can be highly effective, they should be avoided in patients with two emerging eating disorders: Orthorexia Nervosa and Avoidant/Restrictive Food Intake Disorder. It is critical to developing strategies that are not harmful to the patient mentally and physically. The healthcare team should incorporate and support the concept of ‘functional foods” instead (4).
Low FODMAP Diet
FODMAP is an acronym for “fermentable oligosaccharides, disaccharides, monosaccharides, and polyols”. FODMAPs are a collection of short-chain carbohydrates found in many common foods (1, 3, 5).
Listed below is a very long list of foods both high and low in FODMAP. However, keeping track of nutrition will be much easier with the help of the CareClinic Nutrition Tracker. By using this, daily inputs of foods consumed can be recorded and utilized in conjunction with all other functions of the platform.
*Monash University in 2005 was the first to coin the term “FODMAP”. Monash University provides all kinds of IBS help!
Foods High in FODMAP
Similarly, the following foods have been identified as being high in FODMAPs:
Fruits
- For instance, apples (3)
- Apricots(3)
- Blackberries(3)
- Cherries(3)
- Grapefruit(3)
- Mango(3)
- Nectarines(3)
- Peaches(3)
- Pears(3)
- Plums and prunes(3)
- Pomegranates(3)
- Watermelon(3)
- High concentration of fructose from canned fruit, dried fruit, or fruit juice(3)
Grains
- For instance, barley(3)
- For example Couscous(3)
- Farro(3)
- Rye(3)
- Semolina(3)
- Wheat(3)
Lactose-Containing Foods
- For instance, buttermilk(3)
- Cream(3)
- Custard(3)
- Ice cream(3)
- Margarine(3)
- Milk (cow, goat, sheep)(3)
- Soft cheese, including cottage cheese and ricotta(3)
- Yogurt (regular and Greek)(3)
Dairy Substitutes
- For example, oat milk (although a 1/8 serving is considered low-FODMAP)(3)
- For example, soy milk (U.S.)(3)
Legumes
- For example, baked beans(3)
- Black-eyed peas(3)
- Butter beans(3)
- Chickpeas(3)
- Lentils(3)
- Kidney beans(3)
- Lima beans(3)
- Soybeans(3)
- Split peas(3)
Sweeteners
- For example, agave(3)
- Fructose(3)
- High fructose corn syrup(3)
- Honey(3)
- Isomalt(3)
- Maltitol(3)
- Mannitol(3)
- Molasses(3)
- Sorbitol(3)
- Xylitol(3)
Vegetables
- For example, artichokes(3)
- Asparagus(3)
- Beets(3)
- Brussels sprouts(3)
- Cauliflower(3)
- Celery(3)
- Garlic(3)
- Leeks(3)
- Mushrooms(3)
- Okra(3)
- Onions(3)
- Peas(3)
- Scallions (white parts)(3)
- Shallots(3)
- Snow peas(3)
- Sugar snap peas(3)
Foods low in FODMAP
For instance, the following foods have been identified as being lower in FODMAPs:
Fruits
- For instance, avocado (limit 1/8 of the whole)(3)
- for example, bananas(3)
- Blueberry(3)
- Cantaloupe(3)
- Grapes(3)
- Honeydew melon(3)
- Kiwi(3)
- Lemon(3)
- Lime(3)
- Mandarin oranges(3)
- Olives(3)
- Orange(3)
- Papaya(3)
- Plantain(3)
- Pineapple(3)
- Raspberry(3)
- Rhubarb(3)
- Strawberry(3)
- Tangelo(3)
Sweeteners
- For instance, Artificial sweeteners that do not end in -ol (3)
- Brown sugar(3)
- Glucose(3)
- Maple syrup(3)
- Powdered sugar(3)
- Sugar (sucrose)(3)
Dairy and Alternatives
- For example, almond milk(3)
- Coconut milk (limit 1/2 cup)(3)
- Hemp milk(3)
- Rice milk(3)
- Butter(3)
- Certain cheeses, such as brie, camembert, mozzarella, Parmesan(3)
- Lactose-free products, such as lactose-free milk, ice cream, and yogurt(3)
Vegetables
- For example, arugula(3)
- Bamboo shoots(3)
- Bell peppers(3)
- Broccoli(3)
- Bok choy(3)
- Carrots(3)
- Celery root(3)
- Collard greens(3)
- Common cabbage(3)
- Corn (half a cob)(3)
- Eggplant(3)
- Endive(3)
- Fennel(3)
- Green beans(3)
- Kale(3)
- Lettuce(3)
- Parsley(3)
- Parsnip(3)
- Potato(3)
- Radicchio(3)
- Scallions (green parts only)(3)
- Baby Spinach (3)
- Squash(3)
- Sweet potato(3)
- Swiss chard(3)
- Tomato(3)
- Turnip(3)
- Water chestnut(3)
- Zucchini(3)
Grains
- For example, amaranth(3)
- For example, brown rice(3)
- Bulgur wheat (limit to 1/4 cup cooked)(3)
- Oats(3)
- Gluten-free products(3)
- Quinoa(3)
- Spelt products(3)
Nuts
- For example, Almonds (limit 10)(3)
- Brazil nuts(3)
- Hazelnuts (limit 10)(3)
- Macadamia nuts(3)
- Peanuts(3)
- Pecan(3)
- Pine nuts(3)
- Walnuts(3)
Seeds
- For example caraway(3)
- Chia(3)
- Pumpkin(3)
- Sesame(3)
- Sunflower(3)
Protein Sources
- For example, beef(3)
- Chicken(3)
- Eggs(3)
- Fish(3)
- Lamb(3)
- Pork(3)
- Shellfish(3)
- Tofu and tempeh(3)
- Turkey(3)
Physical Activity
Exercise has been shown to help maintain GI function and reduce stress, which in turn can help relieve some IBS symptoms. Studies of IBS have indicated a positive relationship between physical activity and symptom relief (7).
Above all, physical activity, such as pedalling a bicycle, protects against GI symptom aggravation and alleviates gas in several studies. The practice of yoga has also demonstrated a reduction of IBS symptoms in both adult and adolescent populations. In a two-month study, a yoga intervention group practiced twice daily, while the conventional treatment group received 2-6 mg loperamide daily. Results showed that yoga demonstrated improvement of IBS symptoms equivalent to conventional treatment(7).
In addition, using the CareClinic Activity Tracker, tracking physical activity has also become easier. Are you sensing a trend here? Yes. Above all if physical activity, such as yoga, has shown some improvements in IBS symptoms, it is worth a try for some people. Utilize this platform for all of your IBS needs.
Complementary and Alternative Medicine (CAM)
CAM is often used for chronic medical conditions, health promotion, and/or disease prevention. Currently, the available systematic reviews provide conflicting findings on the effectiveness of CAM therapies for IBS. In addition, the American College of Gastroenterology Task Force on IBS reported that CAM therapies have not demonstrated any strong evidence-based support for positive outcomes. On the other hand, other systematic reviews have some evidence of effectiveness (7).
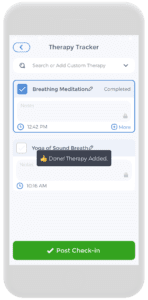
Nevertheless, CAM such as relaxation techniques has been studied for their potential role in alleviating IBS symptoms. Multiple studies have indicated positive correlations among psychological distress, daily stress, and GI symptom aggravation that triggered IBS symptoms. In addition, relaxation training, such as breathing mediation (shown in the picture to the right) may be beneficial for symptom improvement and appears to be at least as effective as standard pharmacological treatment (7).
Keeping track of all the ways you can keep your IBS symptoms at bay is available on the convenient one-stop-shop CareClinic platform. Whichever you decide on trying!
Medications
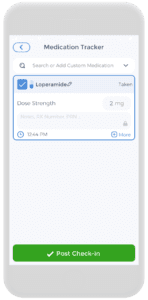
The medication section could be five pages long. There are a lot of choices available and quite frankly, too lengthy to discuss here. Ultimately, the medication that will be chosen will be depending on the IBS symptoms. For example, the picture on the left illustrates Loperamide, a drug that stops diarrhea. If IBS is diarrhea dominant, loperamide will be considered first-line. If IBS is constipation dominant, fiber might be the first line (7).
Additionally, depending on the symptoms, such as bloating or abdominal pain might have their own list of medications. Keeping track of what the poop looks like, the frequency, and food triggers in the food diary/food journal are all vital to the discussion. Speaking to the healthcare team will determine what the prognosis will look like. Be as clear and transparent as possible.
Utilizing the Medication Tracker on the CareClinic Platform will make tracking all medications super easy. Therefore, it will be able to track the dosage of medication and the frequency and comes with refill reminders!
Your Own Digital Poop Tracker
Start your journey today for living an IBS-symptom-Free life! A convenient digital approach to keeping track of poop, as well as other essential factors that can lead you to health freedom! Start your journey today by downloading on your iOS or Android devices by clicking below.
References
- Bellini, M., Tonarelli, S., Nagy, A. G., Pancetti, A., Costa, F., Ricchiuti, A., de Bortoli, N., Mosca, M., Marchi, S., & Rossi, A. (2020). Low FODMAP Diet: Evidence, Doubts, and Hopes. Nutrients, 12(1), 148. https://doi.org/10.3390/nu12010148
- Bolen, B. (2021, June 29). How to Follow an Elimination Diet for IBS. VeryWellHealth. Retrieved from: https://www.verywellhealth.com/how-to-follow-an-elimination-diet-1945007
- Bolen, B. (2021, November 11). High and Low FODMAP Diet Foods to Eat. VeryWellHealth. Retrieved from: https://www.verywellhealth.com/foods-on-the-low-fodmap-diet-1944679
- Chey W. D. (2019). Elimination Diets for Irritable Bowel Syndrome: Approaching the End of the Beginning. The American journal of gastroenterology, 114(2), 201–203. https://doi.org/10.14309/ajg.0000000000000099
- Halmos, E. P., Power, V. A., Shepherd, S. J., Gibson, P. R., & Muir, J. G. (2014). A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology, 146(1), 67–75.e5. https://doi.org/10.1053/j.gastro.2013.09.046
- Patel N, Shackelford K. Irritable Bowel Syndrome. [Updated 2021 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534810/
- Saha L. (2014). Irritable bowel syndrome: pathogenesis, diagnosis, treatment, and evidence-based medicine. World journal of gastroenterology, 20(22), 6759–6773. https://doi.org/10.3748/wjg.v20.i22.6759
- WebMD. (2022, January 16). What Kind of Poop Do I Have? https://www.webmd.com/digestive-disorders/poop-chart-bristol-stool-scale



