Table of Contents
Mucus in the stool is an uncomfortable sight but having to see it chronically is unsettling, especially when there is abdominal pain and alternating constipation that tags along with it. How the disease has two such different symptoms, I do not profess to explain” [1].
Irritable Bowel Syndrome (IBS) is a chronic condition of a functional bowel that can come with abdominal pain, discomfort, bloating, and stool irregularities [4]. According to ROME III criteria, IBS has been classified into four subtypes (a non for profit ROME foundation). Individuals that predominantly have constipation are IBS-C, predominant features of diarrhea are IBS-D, mixed elements of diarrhea, and constipation is IBS-M, while un-subtyped are IBS-U.
Currently, 9%-23% of the world’s population live with IBS, and about 12% of those populations seek a remedy from their Primary Care Physicians [2]. According to American Gastroenterology Association (AGA), IBS is more prevalent in women [2]. Individuals between 30 and 50 tend to reach out to a physician; however, older individuals are less likely to report symptoms. Caucasians and African Americans have a similar prevalence, while lower in Hispanics. Lastly, IBS is present globally, not simply in Western countries. It is also noted that IBS may precede a gastrointestinal infection [4].[1][2]
Mucus in the Stool Causes
It is anyone’s guess, but some workable theories shed some understanding and may help manage IBS symptoms better.
Let’s start with that lingering stress or anxiety that we all have. According to AGA, individuals with IBS under psychosocial stress or anxiety are more susceptible to Gastrointestinal (GI) symptoms. Moreover, there is a strong association between symptoms onset and severity of the symptoms [6]. Numerous studies illustrated the association of gastrointestinal infection preceding IBS symptoms, although it is unclear how infections trigger IBS. Hence, making infectious gastroenteritis a vital risk factor for IBS development.
Although food sensitivity is a working theory, dietary modification remains a primary non-pharmacological intervention for IBS patients [2, 6].[3][4]
Serotonin Dysfunction
A perception of a stimulus within the gut can become modulated at a different level while ascending from the peripheral nervous system to the central system. This symptom has been eluded to somatization disorder [2].
While another working theory is that there might be serotonin dysregulation in the GI tract. Our GI tract is laced with several subtypes of serotonin receptors (5-HT) that help in regulating GI motility, sensation, and secretions [2]. Patients with constipation show a reduced concentration of 5-HT receptors, while patients with diarrhea show an increased concentration of 5-HT. With knowledge of both theories, physicians have been prescribing various types of antidepressants to help individuals with IBS cope with their symptoms.[5][6][7]
Symptoms of Mucus in the Stool
The top symptoms of IBS are abdominal pain, constipation, diarrhea, bloating, belching, and gas.
Abdominal Pain: Abdominal pain or discomfort is the most common symptom associated with alternating bowel movements (constipation and or diarrhea). Characteristic of Abdominal pain is often cramping with fluctuating intensity.
Diarrhea: About 50% of IBS individuals who have diarrhea observe mucous in stool. Most IBS individuals experience diarrheal episodes during the daytime, which usually occur after a meal [6].
Constipation: Generally, it is intermittent but lasts for days. Having such a false sensation can make individuals sit and strain on the commode for too long [6].
Tests & Diagnosis
Ruling out is the best way to go. For example, doing tests for alternate conditions such as Celiac, Inflammatory Bowel Disease, microscopic colitis, and malabsorption will help physicians understand what the patient does not have. It is a lengthy and frustrating process for both patient and the physician. However, a thorough history and clinical observation can help generate a working diagnosis. According to ROME III criteria for IBS, individuals must have an onset of symptoms six months before the diagnosis. Recurrent abdominal pain and discomfort for ≥ 3 days per month in the last three months must be observed with two or more of the following features: onset associated with either stool frequency or change in stool consistency, and/or improvement with defecation [2, 5, 6].[8][9]
Treatment and Therapy for Mucus in Stool
Monitoring Symptoms
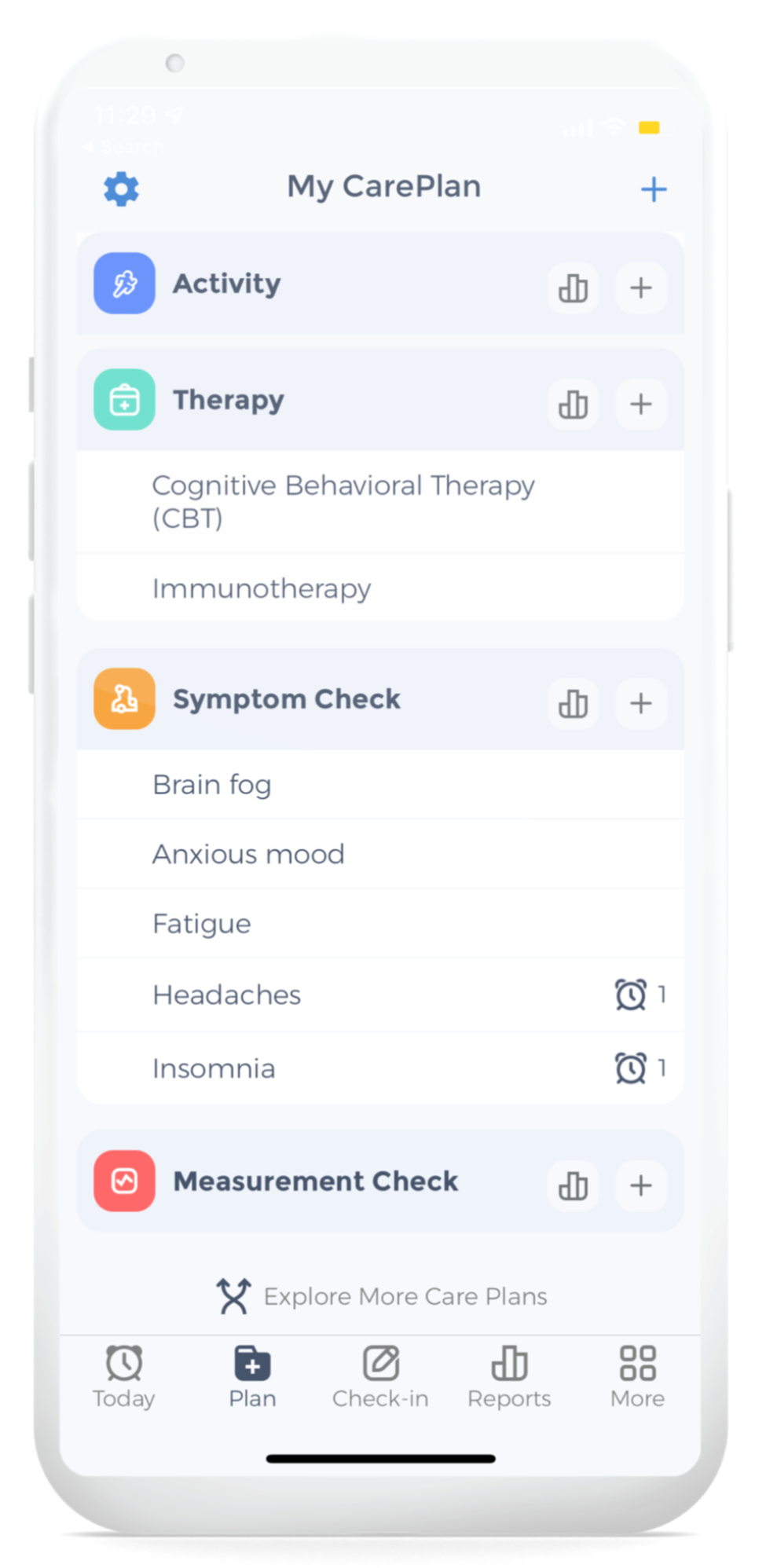
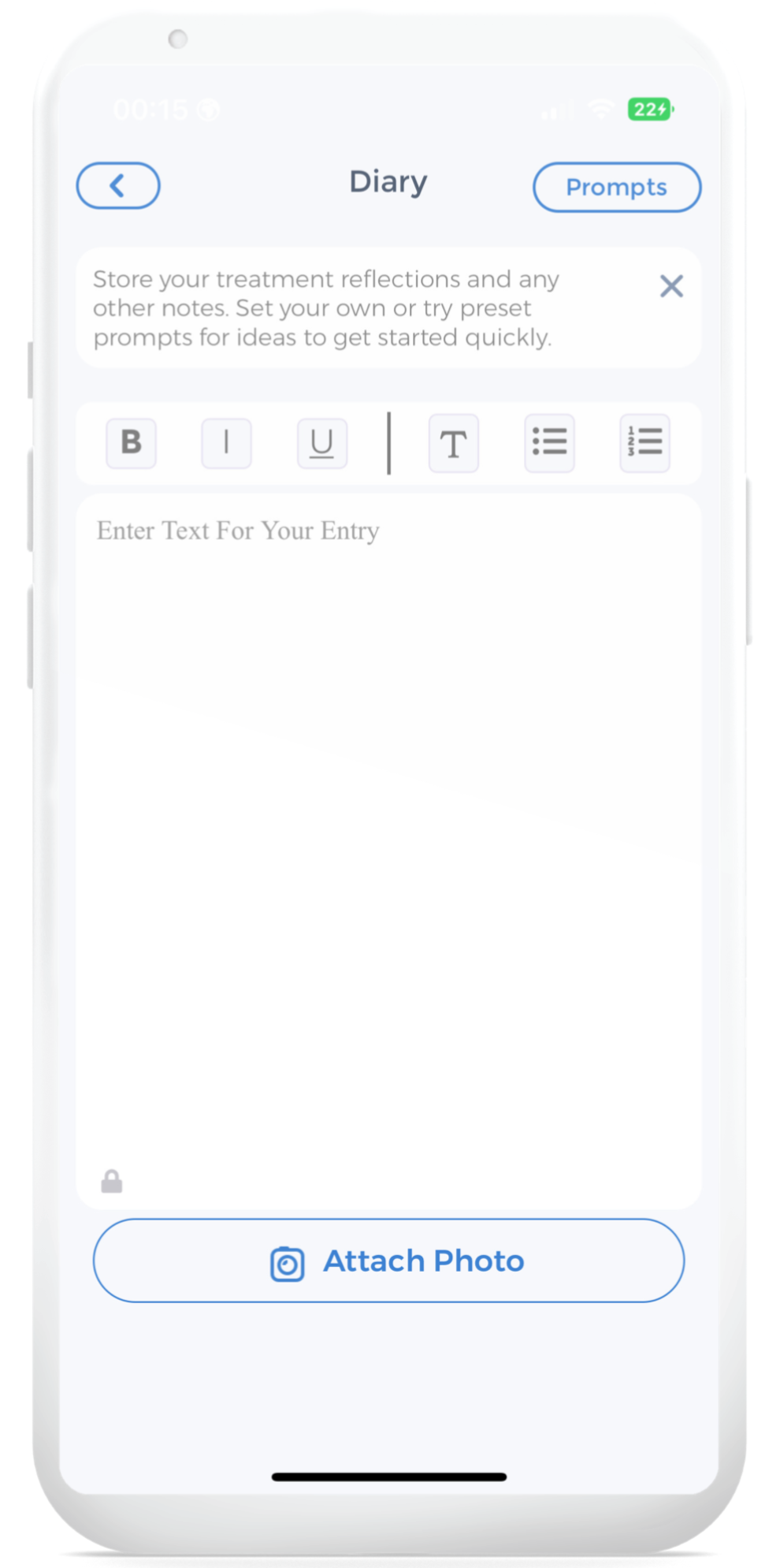
CareClinic also provides you with reports to update you on the progress of your journey. This gives you detailed information on your symptom tracking and an overview of the improvement of your health. You can be descriptive when explaining how your day was, what unfolded, what you experienced, and your emotions, and even grade your experience for all of them from 0 to 10, with “10” being horrible while “0” is no problem. Jotting down your thoughts, emotions, and task for the day will give an insight into your lifestyle and create transparency and better understanding so that the physician can create a unique treatment plan that will benefit you. Get started on your mindfulness journey by downloading the CareClinic app to use features such as its diary and symptom tracker.
Mucus in Stool Monitoring
- Symptoms including the severity and frequency
- Aggravating/alleviating factors
- Environmental, emotional, physical, and cognitive challenges/stressors
Keeping A Stool Log
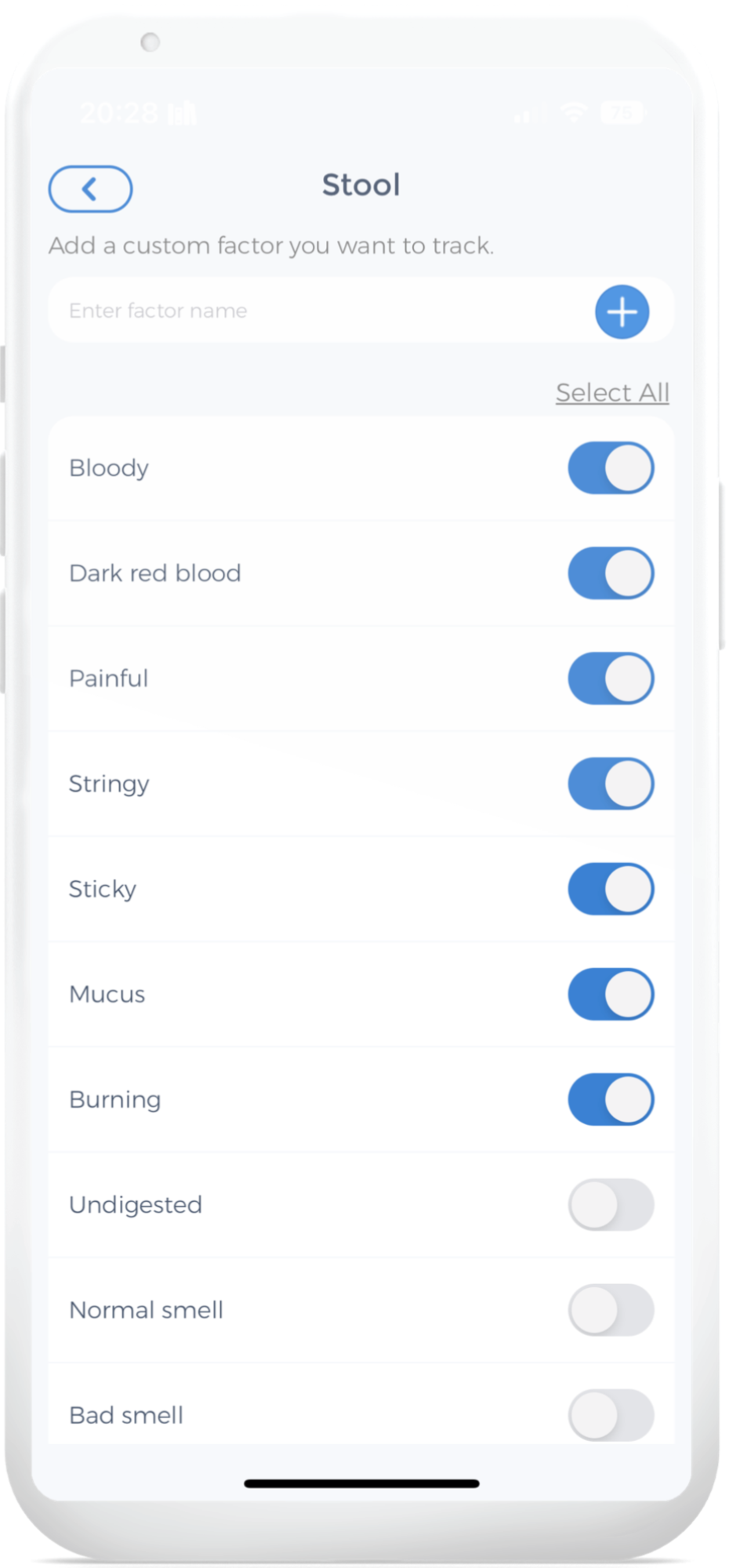
It is possible to experience gut problems without being aware of them. The most effective method to take control of your health and detect these problems early on is to keep track of your bowel movements. The ideal stool-tracking app is CareClinic. It can be for documenting bowel movements diligently.
This is valuable knowledge for identifying whether you have any health problems. Regularly tracking bowel motions may also be advantageous for patients with dyspepsia, persistent bloating, or acid reflux.
For instance, with the help of the log, physicians can make specific diet suggestions.
Lactose Intolerance Mucus in Stool
Dietary restrictions employed in individuals with IBS are commented to have provided some symptomatic relief [2]. For instance, removing dairy products that contain lactose from the diet for 2 weeks and reflecting to see if IBS symptoms have reduced in severity/frequency.
Certain carbohydrates like fermented, oligo-, di-, and monosaccharides and polyols (FODMAPs) have been cited for aggravating IBS symptoms [2].
Increase soluble fibre intake, particularly for IBS-C types, such as psyllium, oat products, pectin, and wheat dextrin. However, adding fiber to the diet can also cause abdominal bloating or gas. Therefore, start with a small amount and incorporate adequate fluid intake while slowly increasing the fiber intake until the stool becomes softer and more frequent [2].
Blood in Stool Meaning
There are many reasons why there may be blood in your stool. If you have bloody diarrhea, it could be a sign of a serious infection. If you see blood when you wipe after a bowel movement, it could be a sign of hemorrhoids. Sometimes, blood in the stool can be a sign of cancer. If you have any concerns, it is best to see a doctor to get a proper diagnosis.
Medications to Help with IBS
Anti-Cholinergic
There is no magic bullet to help abate symptoms of IBS such as bloating, abdominal cramps/pain, diarrhea, and constipation. Antispasmodic (anticholinergic) agents like dicyclomine and hyoscyamine are prophylactically indicated for individuals with IBS who experience pain and bloating, especially after meals [3].
Anti-Diarrheal
For individuals with IBS-Diarrheal, taking loperamide and diphenoxylate-atropine can reduce the propulsive peristaltic movement within the digestive tract. Like other medications, use the Anti-diarrheal as needed and not go beyond the recommended dose as it can cause or aggravate serious heart issues [2].
Antidepressant
As mentioned earlier, specific 5-HT receptors are over-expressed in patients with IBS that had more diarrheal symptoms and under-expression of 5-HT receptors in individuals with constipation. Two main types of medication have been shown to be effective in individuals with IBS, which are tricyclic antidepressant (TCA) and selective serotonin reuptake inhibitor (SSRI) [2]. Significant abdominal pain relief and reducing diarrheal and constipation symptoms have been brought up before TCA and SSRI are implemented. It has been mentioned that TCA has been slightly more responsive in individuals with IBS-D subtypes while SSRIs have been responsive in individuals with IBS-D subtypes. Dosing for both of the treatments may vary; however, there is no indication that the dosage has to be in the antidepressant range and that a low dose is sufficient enough [2].
Anti-Anxiety
Anti-Anxiety medications can be effective for specific individuals; however, these drugs should not be taken by any individuals (unless advised by a health practitioner) for a long duration due to their addictive properties above many other harmful side effects. Diazepam (Valium), clonazepam, and valium (Ativan) are the drugs prescribed to individuals with worsening IBS symptoms for a short period [6].
Clear Mucus in Stool
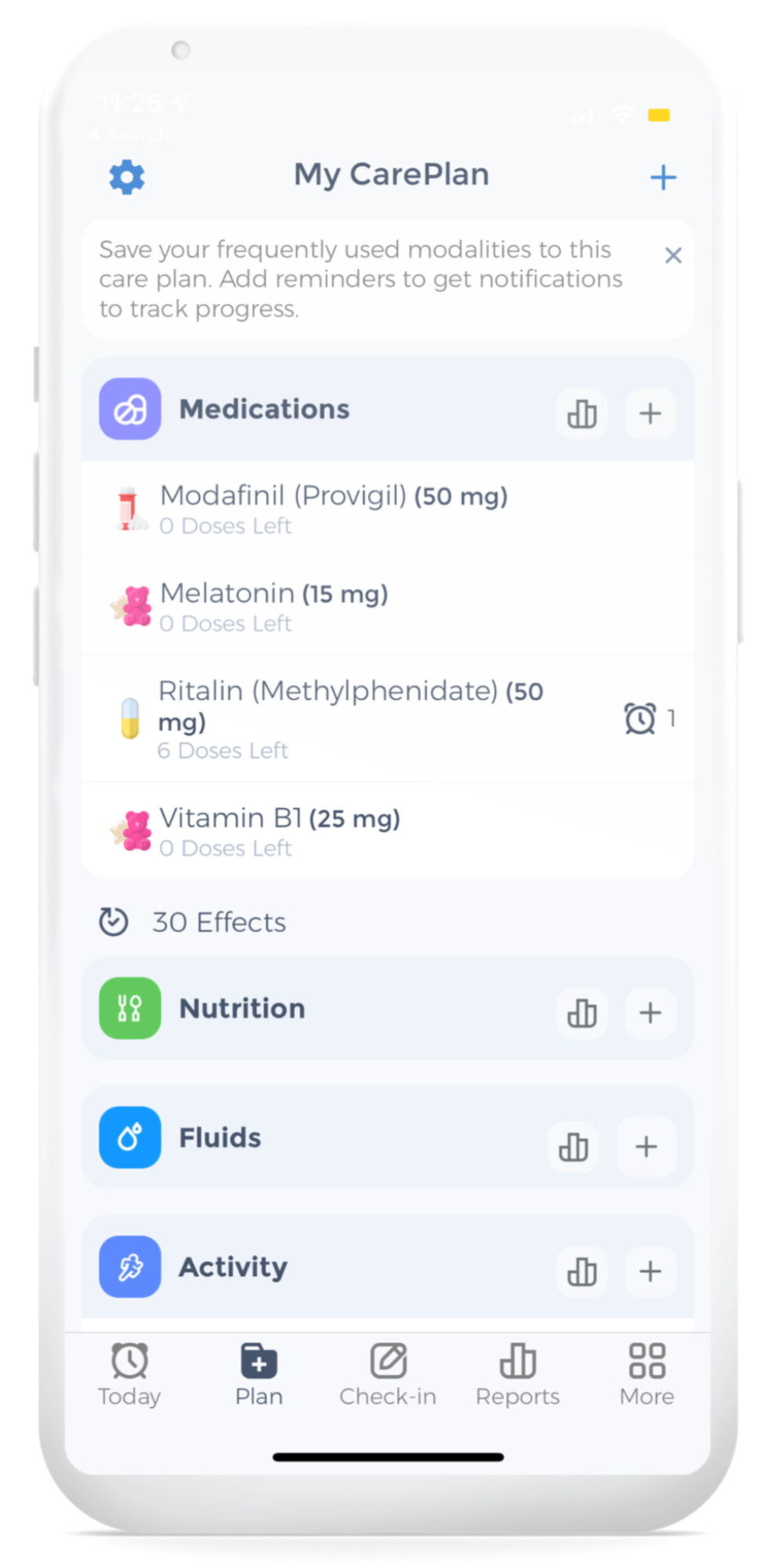
Tracking your medication intake also forces you to stay organized and in control of your treatments. It increases medication adherence, as you will be able to track the efficacy of your treatment and its impact on general health.
It’s fantastic to have a resource where you can keep track of your whole pharmaceutical history. It is a helpful reference tool that speeds up the retrieval of medical data. Furthermore, by utilizing CareClinic to keep track of your previous and present medications, you will limit the chances of misunderstanding. You will make your therapy run more smoothly, and you will attain your health goals.
Additionally, depending on the symptoms, such as bloating or abdominal pain might have their own list of medications. Keeping track of what the poop looks like, the frequency, and food triggers in the food diary are all vital to discuss. Speaking to the healthcare team will determine what the prognosis will look like. Be as clear and transparent as possible.
Alternative Treatments
Lubiprostone and Linactolide
These medications are last-ditch efforts when the above remedies are not effective. Lubiprostone (Amitiza) and Linactolide (Linzess) are best for 18+ females with severe or refractory constipation, with nausea as the side effect of Lubiprostone. Effectiveness and long-term safety are still being studied for both medications. In comparison, Linactolide is more expensive compared to Lubiprostone [6].
Herbal Medications
Herbal alternative medicine such as chamomile tea, peppermint oil, aloe vera, acidophilus, and wormwood have been well-sought natural treatments. However, clinical studies indicate that only a few herbal medications are effective in relieving IBS symptoms.
Another alternative is probiotics like acidophilus which have warranted no benefit. However, probiotic strains such as bifidobacterial, saccharomyces boulardii, and other combinations have been shown to normalize stool behaviour along with decreasing abdominal pain, bloating, and constipation regardless of the IBS subtypes [2]. In contrast, the benefit of chamomile tea and wormwood have been unproven [6].
Psychosocial Therapy
According to National Institute Health and Care Excellence (NICE) guidelines, if an individual with IBS symptoms that do not resolve after interventional medications after 12 months should receive a referral for cognitive-behavioural therapy (CBT), hypnotherapy (gut-directed hypnosis, psychodynamic (interpersonal) therapy, and mindfulness-based therapy, which will be discussed shortly [5, 6].
The idea of CBT is to identify the stressor that is attributing to the IBS symptoms and find a healthier coping mechanism to combat the stressor. By doing so, IBS symptoms may decrease or even diminish [5, 6].
Logging Mucus in Poop
Monitoring Symptoms
Developing a habit can be difficult since you must develop the discipline to sit down and log in. However, once starting this regimen is highly effective and isn’t as demanding. This may also help to unleash your creativity and allow you to wander beyond your usual schedule. Making the time and adopting this discipline will aid in your re-discovery. To truly empower your life, beginning with journaling can be highly beneficial. Furthermore, journaling for mental health purposes will assist you in overcoming any mental barriers you may be encountering.
CareClinic lists a range of journal prompts that you can use on a routine basis, according to your particular needs. This allows you to express a variety of emotions. You also might prefer setting a journaling prompt for each day if you want. This might support you in analyzing all of your emotions on a regular basis in a constructive manner. You may also prefer just to use a poop tracker to log your movements daily as well, you can learn more about tracking poop here.
Take Control of Your IBS Treatment
Living with IBS is hard but living with IBS and managing it is challenging. Thus trying to treat IBS is unique since every individual experiences different symptoms with varying levels of severity and is different to various stressors. About 9 to 23% of the world has been dealing with IBS. There is no specific regimen to help treat mucus in stool completely; however, there are numerous approaches that an individual with IBS can take to alleviate symptoms.
Abdominal discomfort is the top complaint, along with alternating diarrhea and or discomfort regarding gastrointestinal symptoms. There are no specific tests to identify IBS; however, a thorough history and physical will help the physician not only narrow the diagnosis of IBS but rule out other similar conditions.
Monitoring symptoms through the journal or using an electronic diary on the CareClinic App has been crucial to not only diagnosing but helping treat it. Be as descriptive as possible; mention the severity of the pain, the pattern of the symptoms, psychosocial/environmental factors, and even diet. Incorporating products such as fiber into the diet may provide relief while removing harmful products that can worsen the symptoms. Lastly, do not neglect mental health and seek professional help to eliminate negative factors that exacerbate symptoms and quality of life.
References
[1] Horwitz BJ, Fisher RS. The irritable bowel syndrome. N Engl J Med. 2001;344:1846-1850. [PubMed] [DOI] [Cited in This Article: 1] [Cited by in Crossref: 135] [Cited by in F6Publishing: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)]
[2] Saha L. Irritable bowel syndrome: Pathogenesis, diagnosis, treatment, and evidence-based medicine. World J Gastroenterol 2014; 20(22): 6759-6773 [PMID: 24944467 DOI: 10.3748/wjg.v20.i22.6759]
[3] Drossman, D. A., Camilleri, M., Mayer, E. A., & Whitehead, W. E. (2002). AGA technical review on Irritable bowel syndrome. Gastroenterology, 123(6), 2108–2131. https://doi.org/10.1053/gast.2002.37095
[4]Enck, P., Aziz, Q., Barbara, G., Farmer, A. D., Fukudo, S., Mayer, E. A., Niesler, B., Quigley, E. M., Rajilić-Stojanović, M., Schemann, M., Schwille-Kiuntke, J., Simren, M., Zipfel, S., & Spiller, R. C. (2016). Irritable bowel syndrome. Nature Reviews Disease Primers, 2(1). https://doi.org/10.1038/nrdp.2016.14
[5] Aucoin, M., Lalonde-Parsi, M.-J., & Cooley, K. (2014). Mindfulness-based therapies in the treatment of functional gastrointestinal disorders: A meta-analysis. Evidence-Based Complementary and Alternative Medicine, 2014, 1–11. https://doi.org/10.1155/2014/140724
[6] Wald, A. (2015). Patient education: Irritable bowel syndrome (Beyond the Basics). UpToDate. Retrieved February 20, 2022, from https://www.uptodate.com/contents/irritable-bowel-syndrome-beyond-the-basics?search=irritable+bowel+syndrome&source=search_result&selectedTitle=5~150&usage_type=default&display_rank=5
[7] Saha L. (2014). Irritable bowel syndrome: pathogenesis, diagnosis, treatment, and evidence-based medicine. World journal of gastroenterology, 20(22), 6759–6773. https://doi.org/10.3748/wjg.v20.i22.6759
References
- “Bristol stool scale”. https://en.wikipedia.org/wiki/Bristol_stool_scale
- “Irritable bowel syndrome”. https://en.wikipedia.org/wiki/Irritable_bowel_syndrome
- “Gastrointestinal-specific anxiety: an important factor for severity of GI symptoms and quality of life in IBS”. https://pubmed.ncbi.nlm.nih.gov/20367800/
- “Role of infection in irritable bowel syndrome”. https://pubmed.ncbi.nlm.nih.gov/17238025/
- “[Role of serotonin in the pathophysiology of the irritable bowel syndrome]”. https://pubmed.ncbi.nlm.nih.gov/18175558/
- “Serotonin receptor modulators in the treatment of irritable bowel syndrome – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC2503665/
- “Antidepressants for irritable bowel syndrome – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC7145118/
- “Irritable Bowel Syndrome Causes, Signs, Symptoms, Diagnosis”. https://www.dailymeded.com/ibs-irritable-bowel-syndrome-causes-signs-symptoms-diagnosis/
- “Irritable Bowel Syndrome | Abdominal Key”. https://abdominalkey.com/irritable-bowel-syndrome-8/
- “Mucus in Stool: Causes & When To Be Concerned”. https://my.clevelandclinic.org/health/symptoms/mucus-in-stool


