Gastroparesis is a complex condition that can greatly impact a person’s quality of life. Understanding gastroparesis life expectancy, managing its symptoms, risk factors, and coping with its impact are all essential for those living with this condition.
In this article, we will explore the definition and causes of gastroparesis, common gastroparesis symptoms to look out for, factors influencing delayed gastric emptying, and various options to treat gastroparesis. We will also delve into the emotional impact of living with gastrointestinal tract. Highlight support systems and resources that can help patients navigate their journey. Additionally, we will touch on recent advances in gastroparesis treatment and the role of ongoing research in improving life expectancy.
Understanding Gastroparesis
Before we delve into the intricacies of gastroparesis, let’s first gain a comprehensive understanding of this condition. Gastroparesis refers to a disorder that affects the normal movement of food from the stomach into the small intestine. This impaired stomach muscles motility can result in a range of uncomfortable symptoms and complications. Such as nausea, vomiting, and malnutrition.
Gastroparesis is a complex and often misunderstood condition that can have a significant impact on an individual’s quality of life. The delayed emptying of the stomach can lead to a variety of challenges. Including difficulty in managing blood sugar levels for those with diabetes. As well as nutritional deficiencies due to poor absorption of essential nutrients.
Definition and Causes of Diabetic Gastroparesis
Gastroparesis is typically defined as delayed gastric emptying without any structural obstruction. It can be caused by a variety of factors, including diabetes, neurological disorders, certain medications, and viral infections. Understanding the specific cause of gastroparesis is crucial in determining the most appropriate treatment approach.
Diabetes is one of the most common causes of gastroparesis. As high blood sugar levels over time can damage the vagus nerve, which plays a key role in the movement of undigested food through the digestive system. Additionally, certain medications such as opioids and antidepressants can also contribute to the development of gastroparesis by affecting the muscles in the stomach.
Common Symptoms of Gastroparesis
Identifying the common symptoms associated with gastroparesis can help individuals seek timely medical attention and management. Some of the most prevalent signs of gastroparesis include recurrent nausea, vomiting, abdominal pain, bloating, and poor appetite. These symptoms can significantly impact a person’s ability to maintain a healthy lifestyle and nutritional balance.
In addition to the physical symptoms, gastroparesis can also have a profound psychological impact on individuals. Leading to feelings of frustration, anxiety, and social isolation. The unpredictable nature of symptom flare-ups and the dietary restrictions that often accompany gastroparesis can make it challenging for individuals to engage in social activities and enjoy a normal routine.[1]
Life Expectancy with Gastroparesis
Life expectancy for individuals with gastroparesis can vary based on several factors. It is essential to understand these influences to gain a realistic perspective and make informed decisions regarding treatment and lifestyle adjustments.
Gastroparesis is a chronic condition characterized by delayed emptying of the stomach. Leading to symptoms such as nausea, vomiting, and bloating. While the condition itself is not typically life-threatening, complications arising from severe cases of gastroparesis can impact life expectancy. These complications may include malnutrition, dehydration, and unpredictable blood sugar levels, especially in individuals with diabetes.
Factors that Affect Life Expectancy
Several factors can influence the life expectancy of those with gastroparesis. Proper management of blood sugar levels in diabetic individuals. For example, can help minimize complications and improve overall health outcomes. Additionally, addressing comorbid conditions, such as gastrointestinal disorders and cardiovascular disease, is crucial in ensuring the best possible prognosis.
Furthermore, the psychological impact of living with a chronic digestive disorder like gastroparesis should not be underestimated. Mental health challenges, including anxiety and depression, can arise from the physical symptoms and lifestyle adjustments required to manage the condition. Seeking support from mental health professionals and engaging in coping strategies is vital for maintaining overall well-being.
Gastroparesis and Comorbid Conditions
Individuals with gastroparesis often have other underlying health conditions that can further complicate their prognosis. Proper management of these comorbid conditions is essential to improve overall health and quality of life. It’s important to work closely with a healthcare provider to develop a comprehensive treatment plan that addresses all aspects of a person’s health.
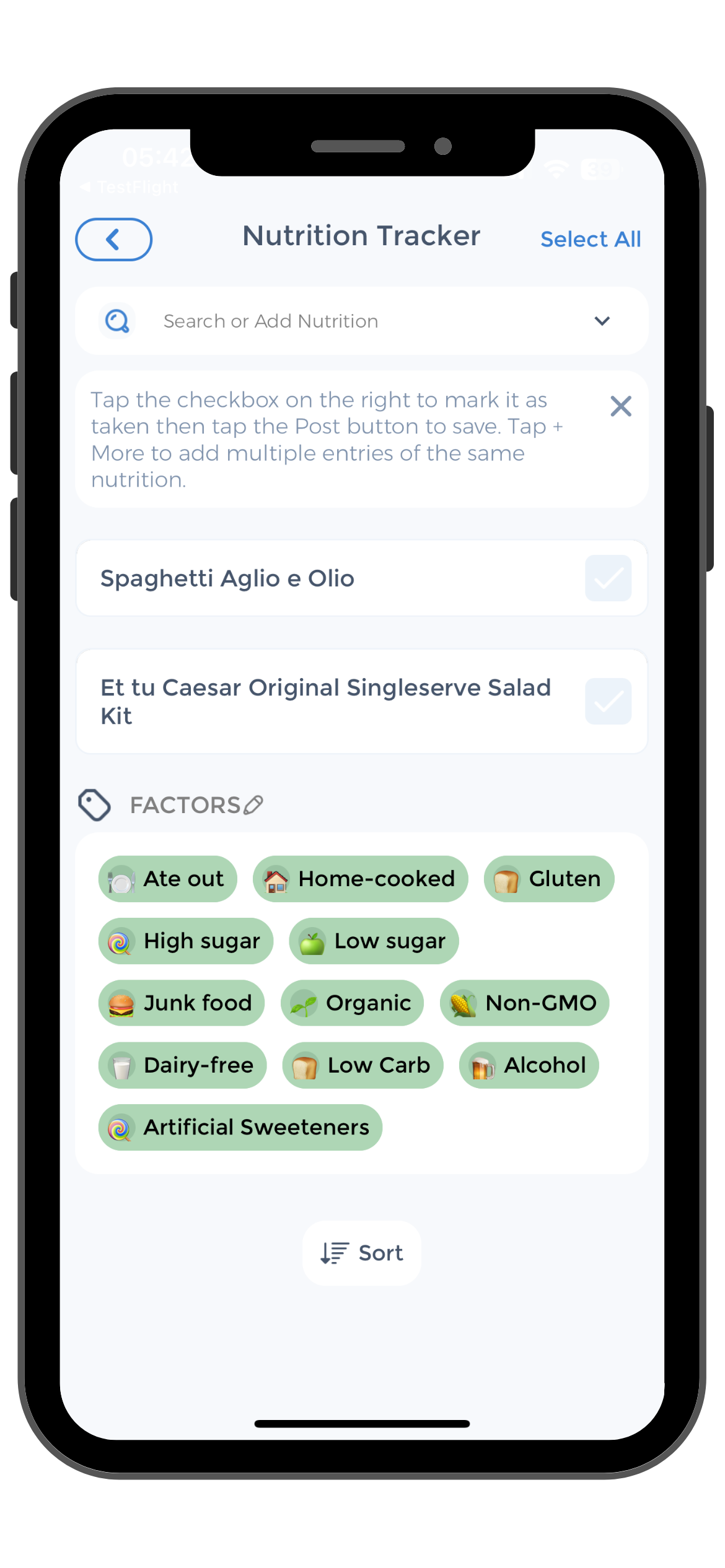
Moreover, dietary modifications play a significant role in managing gastroparesis and its comorbidities. Following a gastroparesis-friendly diet, which typically involves consuming smaller, more frequent meals low in fiber and fat, can help alleviate severe symptoms and improve nutritional intake. Working with a registered dietitian can provide personalized guidance on creating a nutrition plan that meets individual needs and supports overall health.[2][3][4]
Managing Gastroparesis: Gastric Emptying Study
 Living with upper gastrointestinal symptoms can be challenging. But there are numerous strategies that can help effectively manage the condition and alleviate its symptoms. By working closely with healthcare professionals, utilizing medical treatments, and implementing lifestyle changes and home remedies, individuals can significantly improve their overall well-being.
Living with upper gastrointestinal symptoms can be challenging. But there are numerous strategies that can help effectively manage the condition and alleviate its symptoms. By working closely with healthcare professionals, utilizing medical treatments, and implementing lifestyle changes and home remedies, individuals can significantly improve their overall well-being.
When it comes to medical treatments for gastroparesis, the focus is on addressing the underlying causes and managing the symptoms. Healthcare providers may prescribe medications that promote gastric motility. Such as prokinetic agents, to enhance slow stomach emptying. Antiemetics can help relieve and control nausea, acid reflux, and vomiting, while pain medications may be used to alleviate discomfort. In severe cases, surgical interventions like gastric pacemakers may be considered to regulate stomach contractions.
In addition to medical treatments, certain lifestyle changes and home remedies can be beneficial in managing gastroparesis. One important aspect is making adjustments to the diet. Eating smaller, more frequent meals can help ease the burden on the stomach and aid in digestion. It is also crucial to chew food thoroughly to facilitate the breakdown process. Avoiding high-fat and high-fiber foods is recommended. As they can be more difficult to digest. Staying hydrated is essential as well, as dehydration can worsen symptoms.
The Importance of Healthcare Providers to Gastroparesis Patients
Working with a registered dietitian can be immensely helpful in developing a personalized meal plan that suits an individual’s specific needs. They can provide guidance on choosing easily digestible foods, such as soft fruits, cooked vegetables, and lean proteins. It is also advisable to avoid carbonated drinks and alcoholic beverages, as they can exacerbate symptoms.
The Importance of Food Diary to Keep Medical History and Gastroparesis Diagnosis
Keeping a food diary can be a useful tool in identifying trigger foods that worsen symptoms. By tracking what is consumed and noting any adverse reactions, individuals can better understand their own unique dietary triggers. This information can then be used to make informed decisions about food choices and meal planning.
Engage in Physical Activities to Improve Stomach Emptying
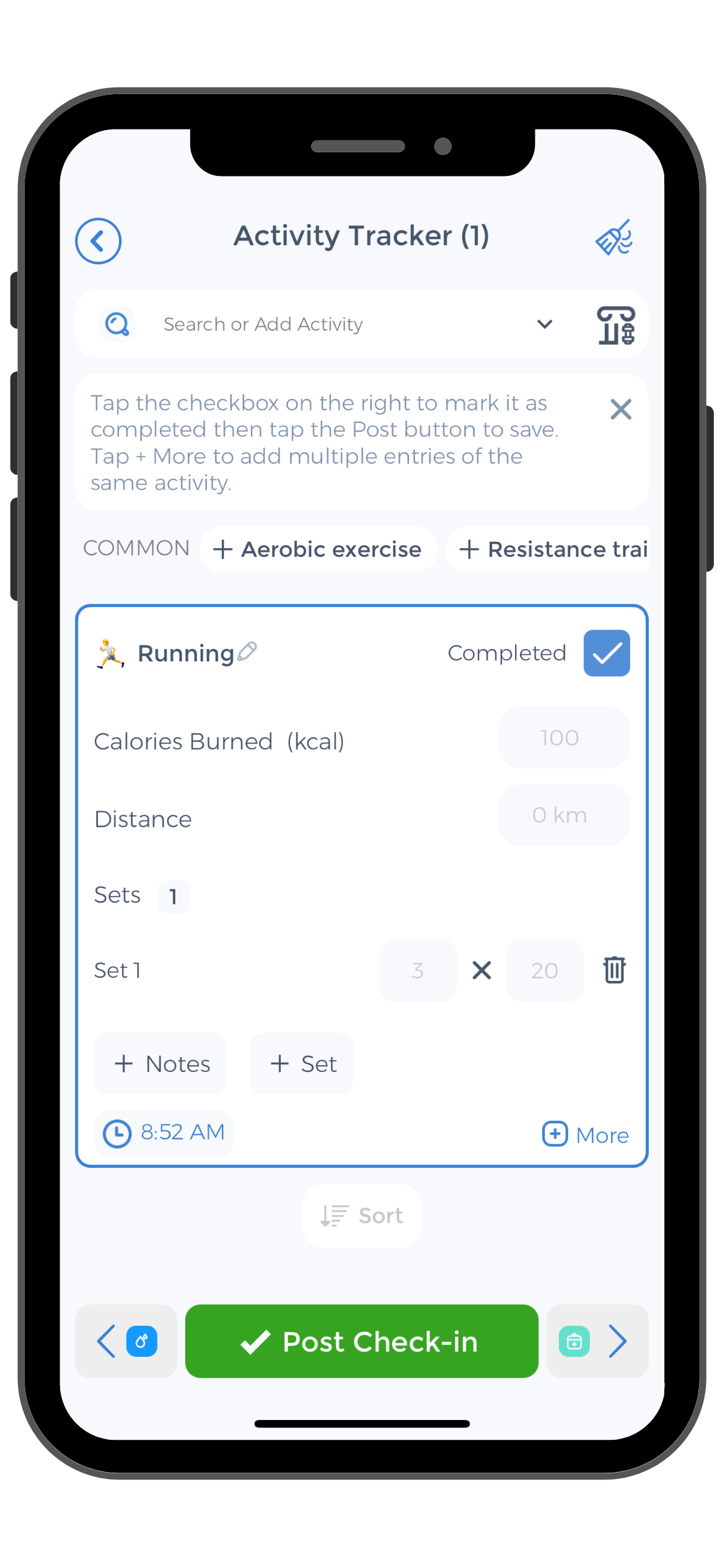
Engaging in gentle exercise, such as walking or yoga, can also aid digestion. Physical activity helps stimulate the muscles in the digestive tract, promoting movement and reducing symptoms. Additionally, finding stress management techniques that work well for each individual is crucial. Deep breathing exercises, meditation, or other relaxation techniques can help reduce stress levels, which in turn can have a positive impact on digestion.
By combining medical treatments, lifestyle changes, and home remedies, individuals with gastroparesis can take control of their condition and improve their quality of life. It is important to remember that managing gastroparesis is an ongoing process that requires patience and perseverance. With the right strategies and support, individuals can find relief from symptoms and regain a sense of well-being.[5][6]
Coping with Gastroparesis to Manage Symptoms
The emotional impact of living with gastroparesis should not be underestimated. Coping with the daily challenges and potential limitations associated with this condition requires resilience, support, and a proactive approach to self-care.
One aspect of coping with gastroparesis that is often overlooked is the impact on relationships. Family members and friends may struggle to understand the complexities of the condition, leading to feelings of isolation and frustration for both the individual with gastroparesis and their loved ones. Open communication, education about the condition, and patience are key in navigating these challenges and fostering strong, supportive relationships.
Emotional Impact of Living with Gastroparesis
Gastroparesis can take an emotional toll on individuals and their loved ones. Dealing with chronic symptoms, lifestyle changes, and the uncertainty of long-term prognosis can lead to frustration, anxiety, and even depression. Seeking professional counseling or joining support groups can provide a platform for sharing experiences and gaining valuable insights from others facing similar challenges.
It’s important to recognize that the emotional impact of gastroparesis can vary greatly from person to person. Some individuals may experience feelings of grief and loss for the life they once had, while others may find strength and resilience in the face of adversity. Acknowledging and validating these diverse emotional experiences is essential in promoting mental well-being and coping strategies.
Support Systems and Resources for Patients
Building a strong support system is crucial for individuals with gastroparesis. Connecting with others who understand the unique struggles of this condition can provide comfort, encouragement, and a sense of belonging. Online communities and patient advocacy organizations can serve as valuable sources of information and emotional support. CareClinic, a comprehensive health management app, offers features designed to help individuals track symptoms, medications, and appointments, and connect with support networks.
Additionally, healthcare providers play a vital role in supporting patients with gastroparesis. Collaborating with a multidisciplinary team, including gastroenterologists, dietitians, mental health professionals, and physical therapists, can ensure comprehensive care that addresses the physical, emotional, and social aspects of living with gastroparesis. By working together, patients and healthcare providers can develop personalized treatment plans that optimize quality of life and overall well-being.[7][8][9]
Future Outlook and Research
The field of gastroparesis research is continuously evolving, offering hope for improved treatment options and better overall life expectancy. Ongoing research strives to uncover the underlying causes, develop more effective therapies, and enhance our understanding of gastroparesis.
One area of research that shows great promise is the exploration of the gut microbiome and its role in gastroparesis. Recent studies have found that alterations in the gut microbiota composition may contribute to the development and progression of gastroparesis. Researchers are now investigating the potential of probiotics and prebiotics in restoring a healthy gut microbiome and alleviating symptoms of gastroparesis. By targeting the gut microbiota, scientists hope to provide a more targeted and personalized approach to treatment.
Advances in Gastroparesis Treatment
Recent advances in gastroparesis treatment have shown promising results. Innovative approaches include the use of botulinum toxin injections to relax the pyloric sphincter and promote stomach emptying. This minimally invasive procedure has been found to be effective in improving gastric emptying and reducing symptoms in some patients.
Another exciting avenue of research is the development of novel drug therapies specifically designed to target the underlying mechanisms of gastroparesis. Researchers are exploring the potential of medications that enhance gastric motility, reduce inflammation in the stomach, and modulate the nervous system. These advancements hold the potential to revolutionize the treatment landscape for gastroparesis and provide patients with more effective and tailored therapeutic options.
The Role of Ongoing Research in Improving Life Expectancy
 Ongoing research plays a vital role in advancing our understanding of gastroparesis and, ultimately, improving life expectancy for individuals with this condition. By exploring novel therapies, identifying genetic markers, and uncovering the complex mechanisms of gastroparesis, researchers are paving the way for more targeted and personalized treatment approaches.
Ongoing research plays a vital role in advancing our understanding of gastroparesis and, ultimately, improving life expectancy for individuals with this condition. By exploring novel therapies, identifying genetic markers, and uncovering the complex mechanisms of gastroparesis, researchers are paving the way for more targeted and personalized treatment approaches.
Additionally, advancements in technology are revolutionizing the way gastroparesis is diagnosed and monitored. Non-invasive imaging techniques, such as magnetic resonance imaging (MRI) and wireless motility capsules, allow for a more comprehensive assessment of gastric function. These tools provide valuable insights into the dynamics of gastric emptying and help clinicians tailor treatment plans to individual patients.
Participating in clinical trials and supporting research initiatives can contribute to progress in the field and provide hope for a brighter future. By volunteering for clinical trials, individuals with gastroparesis have the opportunity to access cutting-edge treatments and contribute to the advancement of medical knowledge. Moreover, supporting research initiatives through donations and advocacy efforts can help accelerate the development of new therapies and improve outcomes for individuals living with gastroparesis.
Gastroparesis is a challenging condition that requires comprehensive management and support. By understanding the definition, causes, and symptoms of gastroparesis, individuals can seek appropriate medical care and make necessary lifestyle adjustments. Embracing self-care strategies, building a strong support system, and staying informed about recent advancements in treatment and research are crucial steps in navigating the complexities of gastroparesis. Remember, you are not alone on this journey, and with the right tools and resources, you can lead a fulfilling life despite the challenges posed by this condition.
Use the CareClinic App to Monitor Gastroparesis Symptoms
Managing idiopathic gastroparesis effectively requires diligent tracking of symptoms, medications, and dietary habits, which is where the CareClinic App becomes an invaluable tool. With its comprehensive health diary feature, you can easily monitor your daily intake, symptom patterns, and medication schedules, allowing for a personalized approach to managing your condition and treating gastroparesis.
The app’s reminder system ensures you never miss a medication dose or a meal, helping to stabilize your routine and potentially reduce gastroparesis flare-ups. By consistently using CareClinic App, you gain insights that can lead to improved health outcomes and a better understanding of your condition.
Download the CareClinic App to Track Delayed Gastric Emptying and Abdominal Pain
As you navigate the complexities of gastroparesis, the CareClinic App serves as a supportive companion. Offering features like symptom tracking and reporting that can be shared with your healthcare provider for more informed treatment decisions. That can also help to avoid develop gastroparesis symptom severity. The app’s ability to correlate your activities with symptom trends provides a clear picture of what may be triggering your gastroparesis episodes, empowering you to make necessary adjustments.
Take the next step in managing your gastroparesis by installing the CareClinic App. Install App today and experience how it can contribute to a more controlled and fulfilling life despite your condition.
References
- “Gastroparesis: Symptoms, Causes, Diagnosis & Treatment”. https://my.clevelandclinic.org/health/diseases/15522-gastroparesis
- “Nutritional deficiencies and predictors of mortality in diabetic and nondiabetic gastroparesis – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC8596206/
- “Psychological controversies in gastroparesis: A systematic review – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC5323455/
- “Dietary Interventions for Gastroparesis: A Systematic Review – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC9526854/
- “Gastroparesis Diet Guidelines | Mayo Clinic Connect”. https://connect.mayoclinic.org/blog/gastroenterology-and-gi-surgery/newsfeed-post/gastroparesis-diet-guidelines-1/
- “Basic Dietary Guidelines – About Gastroparesis”. https://aboutgastroparesis.org/treatments/dietary-lifestyle-measures/basic-dietary-guidelines/
- “Scoping review: the social and emotional impacts of gastroparesis – PubMed”. https://pubmed.ncbi.nlm.nih.gov/39091657/
- “Exploration of the psychosocial issues associated with gastroparesis: a qualitative investigation”. https://pubmed.ncbi.nlm.nih.gov/28071866/
- “Scoping review: the social and emotional impacts of gastroparesis – Simons – Translational Gastroenterology and Hepatology”. https://tgh.amegroups.org/article/view/8873/html


