For additional information, see our guide on what is gastroesophageal reflux disease self-care.
Living with colitis, an inflammatory bowel disease, presents unique challenges, as the condition not only causes physical discomfort but can also disrupt the essential aspect of daily life—sleep. The impact of colitis sleeping position on sleep quality underscores the importance of adopting specific sleeping positions tailored to alleviate symptoms and promote a restful night’s sleep.
Understanding that discomfort is a constant companion for those with colitis, the quest for the ideal sleeping position becomes crucial. For individuals grappling with this condition, several recommended sleeping positions can contribute to enhanced comfort and minimized disruption during the night.[1][2][3]
The Importance of Sleep for Colitis Sufferers
Quality sleep is crucial for everyone, but it’s especially important for those with chronic illnesses like colitis. Sleep allows the body to rest, repair, and rejuvenate, which can help manage symptoms and promote overall health.
Unfortunately, colitis can often interfere with sleep. The discomfort and pain associated with this condition can make it difficult to fall asleep or stay asleep. This lack of sleep can exacerbate symptoms, leading to a vicious cycle of pain and sleeplessness.[4][5]
Relationship between Colitis and Sleep
The intricate relationship between colitis and sleep becomes evident when considering the disruptive impact this inflammatory bowel disease can have on nightly repose. The discomfort and persistent pain associated with colitis create formidable barriers to the ease of falling asleep and maintaining a restful state throughout the night. As if contending with the challenges of a chronic illness were not arduous enough, the coexistence of colitis and disrupted sleep establishes a distressing dynamic, potentially amplifying the severity of symptoms.
This intersection of colitis and sleeplessness establishes a disheartening cycle, where the lack of adequate sleep can intensify the very symptoms it seeks to alleviate. Sleep deprivation has been shown to compromise the immune system, exacerbate inflammation, and heighten pain sensitivity—factors that are particularly detrimental for individuals with colitis. Consequently, the interplay between pain and sleeplessness creates a relentless loop, each factor perpetuating the other in a distressing dance that diminishes overall well-being.
Recognizing the intricate link between colitis and sleep underscores the imperative for a comprehensive approach to managing this chronic condition. While medical interventions and dietary considerations are integral components of colitis management, prioritizing sleep as a therapeutic element cannot be overstated. Developing tailored strategies to mitigate sleep disturbances becomes a vital aspect of the holistic care required for those navigating the challenges of colitis.
In essence, understanding the importance of quality sleep for colitis sufferers extends beyond a mere acknowledgment of its benefits—it becomes a strategic imperative. By actively addressing sleep disruptions and prioritizing restorative sleep, individuals with colitis can potentially break free from the detrimental cycle of pain and sleeplessness, contributing to a more balanced and resilient approach to managing their health.[6][7][8]
Understanding Colitis and Its Impact on Sleep
Colitis is characterized by inflammation of the colon’s inner lining, leading to symptoms such as abdominal pain, diarrhea, and rectal bleeding. These symptoms can be particularly bothersome at night, disrupting sleep and leading to fatigue and decreased quality of life.
Furthermore, some medications used to treat colitis can also interfere with sleep. Steroids, for example, can cause insomnia. Understanding the impact of colitis and its treatment on sleep is the first step towards finding solutions.[9]
Best Colitis Sleeping Position
Navigating a restful night’s sleep with colitis involves more than just closing your eyes. The right sleeping position can make a significant difference in managing symptoms and promoting overall well-being. Explore the following recommended sleeping positions tailored for colitis sufferers to enhance comfort and alleviate discomfort.
Left Side Sleeping
One of the best sleeping positions for people with colitis is on the left side. This position can help gravity move waste through the colon more efficiently, potentially reducing discomfort and bloating.
Moreover, left-side sleeping can also aid in digestion and reduce heartburn, which can be beneficial for those with colitis who also suffer from gastroesophageal reflux disease (GERD).
Elevated Upper Body
Elevating the upper body while sleeping can also be beneficial for colitis sufferers. This position can help reduce acid reflux, a common issue for those with this condition. Using a wedge pillow or adjustable bed can help achieve this position.
Additionally, this position can also help reduce pressure on the colon, potentially reducing discomfort and aiding in a better night’s sleep.
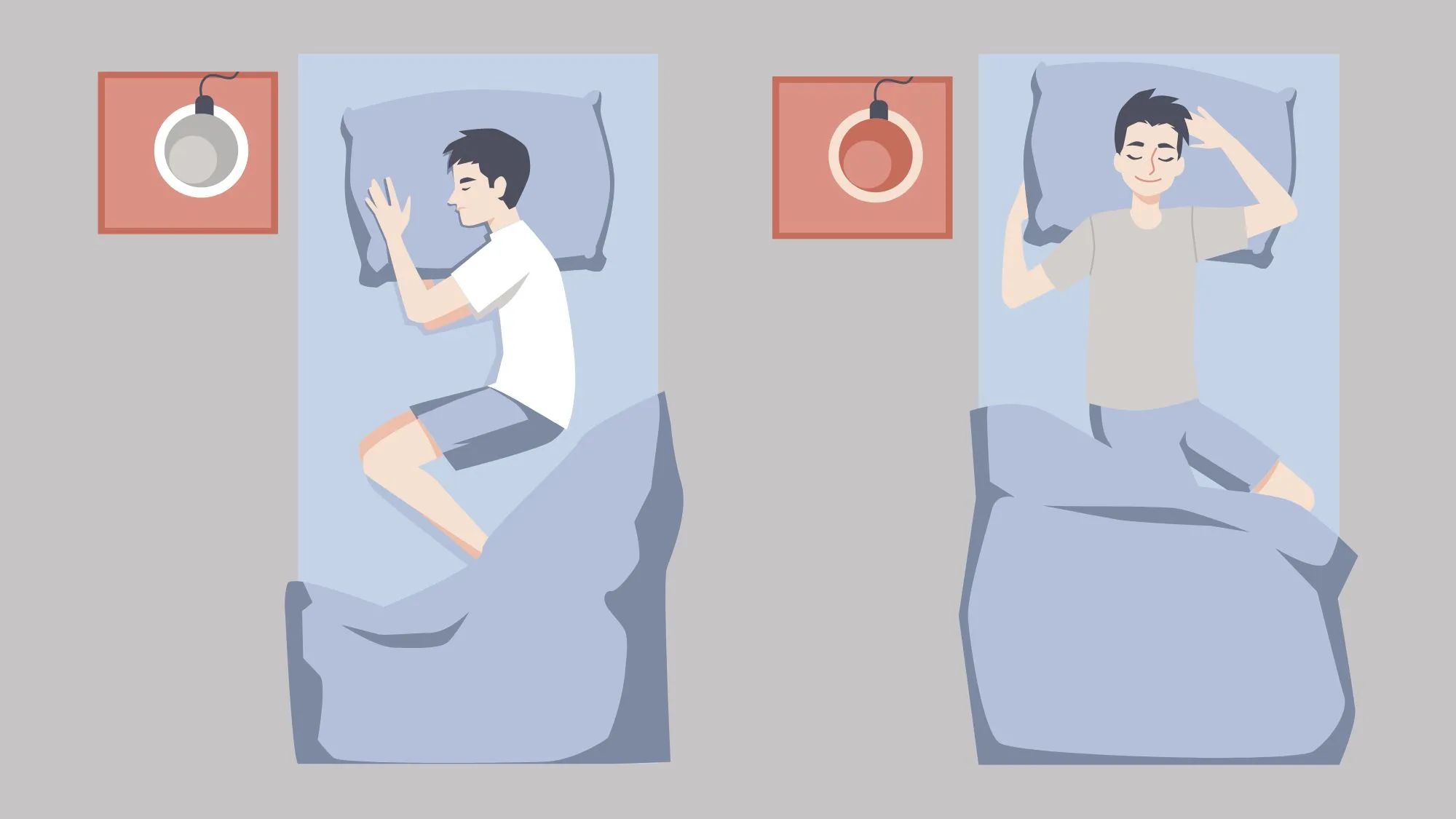
Fetal Position
The fetal position, where you sleep on your side with your knees drawn up towards your chest, can also be beneficial. This position can help reduce pressure on the abdomen, potentially alleviating discomfort.
However, it’s important to note that this position may not be comfortable for everyone, and it’s crucial to find a position that works best for you.[10][11]
Additional Tips for Better Sleep with Colitis
Living with colitis necessitates a multifaceted approach to well-being, and achieving restful sleep is a critical component of this holistic strategy. Beyond discovering the right sleeping positions, consider incorporating the following tips into your routine to enhance the quality of your sleep and, consequently, your overall quality of life.
Maintain a Regular Sleep Schedule
Keeping a consistent sleep schedule can help regulate your body’s internal clock, making it easier to fall asleep and wake up. Try to go to bed and wake up at the same time every day, even on weekends.
Additionally, establishing a relaxing bedtime routine can signal to your body that it’s time to sleep. This could include activities such as reading a book, listening to calming music, or practicing deep breathing exercises.
Manage Diet and Medication
What you eat and when you take your medication can also impact your sleep. Try to avoid eating large meals close to bedtime, as this can lead to discomfort and disrupt sleep. If your medication causes insomnia, talk to your doctor about possibly adjusting the timing of your doses.
Furthermore, certain foods can exacerbate colitis symptoms. Keeping a food diary can help identify any triggers and aid in managing your condition.
Exercise Regularly
Regular exercise can help manage colitis symptoms and promote better sleep. However, it’s important not to exercise too close to bedtime, as this can interfere with sleep. Aim for at least 30 minutes of moderate exercise most days of the week, but try to finish exercising at least a few hours before bed.
Remember, managing colitis and achieving better sleep requires a holistic approach. It’s not just about finding the right sleeping position, but also about managing your diet, medication, and lifestyle. Always consult with your healthcare provider before making any changes to your treatment plan.[12][13][14]
Use the CareClinic App to Track Colitis Sleeping Position
The CareClinic App is your comprehensive solution for managing your colitis sleeping position. Expect features like sleep stage recording, trend analysis, and tailored recommendations that work together to enhance your sleep patterns and colitis sleeping position. By consistently tracking your sleep and related health habits within the CareClinic App, you can uncover the keys to restful nights and energized mornings. Experience the benefits of informed self-care and join the community of users achieving improved health outcomes. Install the CareClinic App today and embark on a journey to better sleep and overall well-being.[15]
References
- “Try a New Sleeping Position in the Bedroom”. https://www.bezzyibd.com/discover/managing-ibd/health-sleep-position-matters/
- “Sleep Hygiene for Ulcerative Colitis: Enhancing Restorative Sleep – Cure Ulcerative Colitis”. https://cureulcerativecolitis.com/sleep-hygiene-for-ulcerative-colitis-enhancing-restorative-sleep/
- “Sleep | Crohn's & Colitis Foundation”. https://www.crohnscolitisfoundation.org/justlikeme/living-with-crohns-and-colitis/sleep
- “A meta-analysis on sleep quality in inflammatory bowel disease”. https://pubmed.ncbi.nlm.nih.gov/34214847/
- “Sleep Quality Drives Next Day Pain and Fatigue in Adults With Inflammatory Bowel Disease: A Short Report – PubMed”. https://pubmed.ncbi.nlm.nih.gov/37526279/
- “How to Get Better Sleep When You Have IBD”. https://time.com/6270567/how-to-sleep-better-ibd-remedies/
- “How sleep deprivation can cause inflammation – Harvard Health”. https://www.health.harvard.edu/healthbeat/how-sleep-deprivation-can-cause-inflammation
- “Addressing poor sleep quality to improve IBD health outcomes | Crohn's & Colitis Foundation”. https://www.crohnscolitisfoundation.org/blog/addressing-poor-sleep-quality-to-improve-ibd-health-outcomes
- “Insomnia and IBD: Tips for Better Sleep | MyCrohnsAndColitisTeam”. https://www.mycrohnsandcolitisteam.com/resources/insomnia-and-ibd
- “Sleep in this position for better gut health | MDLinx”. https://www.mdlinx.com/article/sleep-in-this-position-for-better-gut-health/3kl6LeKZfAtdGngYjAF05D
- “The Best Sleeping Positions for Digestion”. https://greatist.com/health/best-sleeping-position-for-digestion
- “Sleep Hygiene is Important for IBD”. https://inflammatoryboweldisease.net/living/sleep-hygiene
- “Strategies for a better night's sleep with IBD – Sharecare”. https://www.sharecare.com/digestive-health/ibd/strategies-good-night-sleep-ibd
- “How to Sleep Better With Ulcerative Colitis”. https://www.healthcentral.com/condition/ulcerative-colitis/ulcerative-colitis-sleeping-position
- “Symptom & Mood Tracker – Apps on Google Play”. https://play.google.com/store/apps/details


