Living with chronic pain can be a difficult and debilitating experience. It can impact daily activities, relationships, and overall quality of life. Fortunately, there is growing evidence that cognitive behavioral therapy (CBT) can be an effective approach to managing chronic pain. In this article, we will explore the role of CBT in chronic pain treatment, including what it is, how it works, and its benefits and limitations.[1][2][3]
Understanding Chronic Pain
Before we dive into the details of CBT for pain, let’s first clarify what we mean by chronic pain. Chronic pain is defined as any pain that lasts for more than 3-6 months or beyond the normal healing time of an injury or illness. It can be caused by a variety of factors, including injury, illness, or a combination of both. It is estimated that over 20% of adults in the US suffer from chronic pain, making it a significant public health concern.
Defining Chronic Pain
Chronic pain is often described as a complex, multidimensional pain experience that includes physical,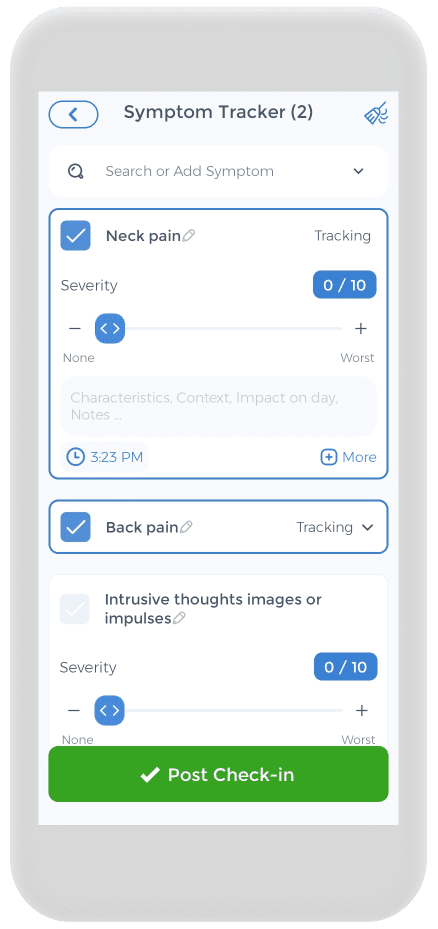 emotional, and cognitive components. It can be constant or intermittent, sharp or dull, and can impact various areas of the body. Chronic pain disorders are highly individualized, and each person’s experience may be different due to a variety of factors, such as genetics, lifestyle, and psychological state.
emotional, and cognitive components. It can be constant or intermittent, sharp or dull, and can impact various areas of the body. Chronic pain disorders are highly individualized, and each person’s experience may be different due to a variety of factors, such as genetics, lifestyle, and psychological state.
For many people, pain can be a frustrating and challenging condition to manage. It can affect every aspect of a person’s life due to daily pain, from their ability to work and enjoy hobbies to their relationships with friends and family, leading to a vicious cycle. Pain can also lead to other health problems, such as depression, anxiety, and sleep disturbances.
Common Causes of Chronic Pain
Chronic pain can be caused by a variety of factors, including but not limited to:
- Injury, such as a sprain or fracture
- Illness, such as arthritis or fibromyalgia
- Repetitive strain, such as carpal tunnel syndrome
- Neurological disorders, such as multiple sclerosis
- Psychological factors, such as stress and anxiety
It is important to note that chronic pain can also be caused by a combination of these factors, and these factors can make the pain worse. For example, someone with arthritis may also experience stress and anxiety, which can exacerbate their pain symptoms.
Treatment and Management of Chronic Pain
There are many different approaches to treating and managing chronic pain, and what works for one person may not work for another. Some common treatment methods and options include:
- Medications, such as pain relievers, anti-inflammatory drugs, and antidepressants
- Physical therapy, including exercises and stretches to improve strength and flexibility
- Acupuncture, massage, and other complementary therapies
- Cognitive-behavioral therapy (CBT), which focuses on changing negative thought patterns and behaviors that may be contributing to pain
Individuals with physical pain need to work closely with their healthcare providers to develop a treatment plan that is tailored to their specific needs. This may involve trying different treatments and making lifestyle changes, such as improving diet and exercise habits or reducing stress.
The Impact of Chronic Pain on Daily Life
Chronic pain can have a profound impact on daily activities, making it difficult to work, exercise, or even perform basic tasks such as cooking or cleaning. It can also lead to social isolation, depression, anxiety, and other mental health and psychiatric symptoms, further complicating treatment and management.
One of the challenges of managing chronic pain is finding ways to maintain a sense of purpose and enjoyment in life despite the limitations it can impose. This may involve finding new hobbies or activities that can be done despite pain, or finding ways to adapt existing activities to make them more manageable.
Ultimately, the key to managing chronic pain is taking a holistic approach that addresses both physical, emotional, and psychosocial factors. By working closely with healthcare providers and making lifestyle changes as needed, individuals with chronic pain can improve their quality of life and find ways to thrive despite their condition.[4][5][6][7]
Cognitive Behavioral Therapy: An Overview
![]() Cognitive behavioral therapy (CBT) is a form of psychotherapy that focuses on changing negative thoughts, emotions, and behaviors. It is based on the idea that the way we think and feel can influence our behaviors and the way we experience pain. CBT is a structured, time-limited approach that typically involves weekly sessions with a trained therapist.
Cognitive behavioral therapy (CBT) is a form of psychotherapy that focuses on changing negative thoughts, emotions, and behaviors. It is based on the idea that the way we think and feel can influence our behaviors and the way we experience pain. CBT is a structured, time-limited approach that typically involves weekly sessions with a trained therapist.
Cognitive behavior therapy is widely used for treating depression, anxiety disorders, and post-traumatic stress disorder (PTSD), as well as other mental health problems. However, it is also increasingly being used as a treatment for chronic pain.
Principles of Cognitive Behavioral Therapy
Cognitive behavioral therapy is an evidence-based treatment based on several key principles, including:
- Identifying negative or unhelpful thoughts
- Reframing negative thoughts into more positive or realistic ones
- Develop and learn coping skills to better manage stress and pain
- Creating a plan of action to achieve goals related to pain management and overall health and wellness
By identifying negative feelings and thoughts and reframing them into more positive or realistic ones, individuals can gain a greater sense of control over their thoughts and emotions. This can lead to a reduction in stress and anxiety, which can in turn help to reduce pain levels.
Developing coping skills is also an important part of CBT skills. Coping skills can include relaxation techniques, such as deep breathing or meditation, as well as physical activities, such as exercise or yoga. By learning and practicing these skills, individuals can better manage their pain and improve their overall quality of life.
The Process of Cognitive Behavioral Therapy
CBT techniques typically involve several stages, including:
- Evaluation: The cognitive behavioral therapist assesses the patient’s current level of pain, functioning, and mood.
- Goal-setting: The patient and therapist work together to identify specific goals related to pain management and overall functioning.
- Therapy sessions: The patient meets with the therapist regularly to learn and practice coping skills, identify and challenge negative thoughts, and develop a plan of action.
- Outcome evaluation: The therapist evaluates progress toward the patient’s goals and makes any necessary adjustments to the treatment plan.
CBT is typically a short-term treatment, with most patients seeing significant improvement within 12-16 weeks. However, the length of treatment can vary depending on the individual and the severity of their pain.
Benefits and Limitations of Cognitive Behavioral Therapy
CBT treatment is effective in reducing pain intensity, improving mood, and enhancing overall functioning in individuals with chronic pain. It can also be used in conjunction with other pain management approaches, such as medication and physical therapy to improve treatment outcomes and reduce pain.
However, CBT interventions are not a one-size-fits-all approach, and they may not be effective for everyone. Additionally, it requires a strong commitment to attending therapy sessions and actively participating in the treatment process. Individuals need to work closely with their therapist to develop a personalized treatment plan that meets their specific needs, which may also involve acceptance and commitment therapy.
Overall, CBT skills are a valuable tool for individuals with chronic pain who are looking to improve their quality of life and manage their pain more effectively.[8][9][10]
The Connection Between Chronic Pain and Cognition
The relationship between chronic pain and cognition is complex and bidirectional. That is, chronic pain can impact cognitive functioning, and cognitive processes can influence the way we perceive and experience pain.
Chronic pain can lead to changes in the brain, including alterations in gray matter volume and changes in neural activity. These changes can impact cognitive functioning, such as attention, memory, and decision-making. For example, individuals with chronic pain may have difficulty concentrating or remembering information due to the constant distraction of pain.
On the other hand, cognitive processes can also influence the experience of pain. For example, distraction techniques, such as engaging in a mentally stimulating task, can reduce pain perception by redirecting attention away from the pain.
The Role of Thoughts and Beliefs in Pain Perception
Research has shown that negative thoughts and beliefs about pain can increase pain perception and intensity. For example, individuals who catastrophize about pain and believe that it is uncontrollable may experience more intense pain than those who are able to reframe negative thoughts about emotional pain and focus on coping strategies.
Positive thinking and belief in one’s ability to manage pain can have a positive impact on pain perception. CBT intervention focuses on changing negative thought patterns and beliefs about pain to improve pain management and overall functioning.
The Impact of Emotions on Pain
Emotional factors, such as stress and anxiety, can also impact pain perception and intensity. When we are stressed or anxious, our body releases a range of hormones that can affect the way we experience pain. Additionally, negative emotions can exacerbate pain by increasing muscle tension and causing us to focus more on the pain itself.
Relaxation techniques, such as deep breathing and progressive muscle relaxation, can help reduce chronic stress and anxiety and improve pain management. Mindfulness-based stress reduction (MBSR) is another treatment approach that focuses on cultivating mindfulness and reducing stress to improve overall well-being and pain management.
The Influence of Behavioral Patterns on Pain
Our behaviors can also impact pain perception and intensity. For example, avoiding activities that cause pain may make the pain worse by leading to increased muscle tension and reduced overall functioning.
Physical therapy and occupational therapy can help individuals with chronic pain develop healthy behavioral patterns and improve overall functioning. These therapies may include exercise programs, ergonomic adjustments, cognitive therapy, and activity pacing strategies.[11][12]
Cognitive Behavioral Therapy For Pain Management
Living with chronic pain can be a debilitating experience that affects every aspect of a person’s life. It can lead to feelings of frustration, hopelessness, and despair, and can make even the simplest tasks seem impossible. However, there is hope for those who suffer from chronic pain. Cognitive Behavioral Therapy (CBT) is an effective treatment for chronic pain management. CBT is a behavioral medicine, a type of psychotherapy that focuses on changing negative thoughts, emotions, and behaviors and replacing them with more positive and adaptive ones.
Cognitive Restructuring
Cognitive restructuring is a key component of CBT for chronic pain management. It involves identifying negative thoughts related to pain and challenging them with more positive or realistic ones. Negative thoughts can include beliefs such as “I will never be able to do the things I love because of my ongoing pain now” or “My pain will never go away.” These thoughts can be replaced with more positive ones, such as “Although it may be difficult, I can still find ways to do the things that are important to me” or “My pain may never completely go away, but I can learn to manage it and live a fulfilling life.”
Cognitive restructuring can be a challenging process, as negative thoughts can be deeply ingrained and automatic. However, with the help of a trained therapist, individuals can learn to recognize and challenge these thoughts and replace them with more positive and adaptive ones.
Relaxation Techniques
Relaxation techniques are another important component of CBT for chronic pain management. Chronic pain can lead to muscle tension and overall stress, which can exacerbate pain and make it more difficult to cope. Relaxation techniques such as deep breathing, progressive muscle relaxation, and guided imagery can be effective in reducing muscle tension and overall stress levels.
Deep breathing involves taking slow, deep breaths and focusing on the sensation of the breath moving in and out of the body. Progressive muscle relaxation training involves tensing and then relaxing different muscle groups in the body, which can help reduce overall muscle tension. Guided imagery involves visualizing peaceful and relaxing scenes, which can help reduce stress and promote relaxation.
Goal Setting and Activity Pacing
Goal setting and activity pacing are important strategies for managing chronic pain. Chronic pain can make it difficult to engage in once enjoyable activities, which can lead to feelings of frustration and hopelessness. However, by breaking down large goals into smaller, manageable steps, individuals can gradually increase their activity levels over time.
Activity pacing involves balancing periods of activity with periods of rest to avoid overexertion and fatigue. By pacing activities and taking breaks when needed, individuals can reduce the risk of exacerbating their pain and increase their overall functioning.
Mindfulness & Acceptance
Mindfulness and acceptance are important skills for managing chronic pain. It involves![]() learning to be present in the moment without judgment and accepting pain as an inevitable part of life. By practicing mindfulness, individuals can learn to observe their pain without becoming overwhelmed by it and can reduce the emotional distress associated with chronic pain.
learning to be present in the moment without judgment and accepting pain as an inevitable part of life. By practicing mindfulness, individuals can learn to observe their pain without becoming overwhelmed by it and can reduce the emotional distress associated with chronic pain.
Acceptance involves acknowledging that chronic pain is a part of life and learning to live a fulfilling life despite it. This can involve finding new hobbies or activities that are less physically demanding, or learning to adapt to physical limitations to continue engaging in activities that are important to them.
In conclusion, CBT is a powerful tool for managing chronic pain. By using techniques of cognitive behavior therapy, such as cognitive restructuring, relaxation, goal setting, and mindfulness, individuals with cancer pain can learn to manage their pain and live a fulfilling life. If you or someone you know is struggling with chronic pain, consider seeking the help of a trained CBT therapist.[13][14]
Evidence Supporting the Use of CBT for Chronic Pain
There is growing evidence that CBT can be an effective approach to managing chronic pain. Research studies have found that CBT can lead to significant reductions in pain intensity, improved mood, and enhanced functioning.
Chronic pain can be a debilitating condition that affects millions of individuals worldwide. It can impact a person’s ability to work, socialize, and engage in everyday activities. While there are various medical treatment options available for chronic pain, CBT has emerged as a promising approach.
Research Findings on CBT and Chronic Pain
A recent meta-analysis of 60 studies found that CBT is effective in reducing pain intensity and improving overall functioning in individuals with chronic pain. The studies included in the meta-analysis involved individuals with a range of chronic pain conditions, including fibromyalgia, chronic back pain, and arthritis.
Another study published in JAMA found that CBT was more effective than usual care in reducing pain intensity and improving physical functioning in individuals with chronic back pain. The study involved 342 individuals with chronic back pain who were randomly assigned to receive either CBT or usual care.
Comparing CBT to Other Pain Management Approaches
While CBT is effective in reducing pain and improving functioning, it is not the only approach to chronic pain management. Other approaches to treat chronic pain, such as medication, physical therapy, and mindfulness-based interventions, may also be effective for some individuals.
Medication can be an effective way to manage chronic pain, but it is not without its risks. Long-term use of pain medication can lead to dependence, addiction, and other adverse effects. Physical therapy can help individuals with chronic pain improve their physical functioning and reduce pain, but it may not address the underlying psychological factors that contribute to the pain.
Mindfulness-based interventions, such as mindfulness meditation and yoga, have also been shown to be effective in reducing chronic pain. These approaches focus on increasing awareness and acceptance of the present moment and can help individuals develop a more positive relationship with their pain.
Long-term Benefits of CBT for Chronic Pain
Research has also shown that the benefits of CBT for chronic pain may extend beyond the end of treatment. A study published in the Journal of Pain found that individuals who received CBT therapy for chronic pain still had lower pain scores and improved functioning one year after treatment compared to those who received usual care.
The study involved 342 individuals with chronic back pain who were randomly assigned to receive either CBT or usual care. The individuals who received CBT had significantly lower pain scores and improved functioning one year after treatment compared to those who received usual care.
In conclusion, CBT has emerged as a promising approach to managing chronic pain. While it may not be the only approach to chronic pain management, research has shown that it can lead to significant reductions in pain intensity, improved mood, more pain control, and enhanced functioning. Furthermore, the benefits of CBT may extend beyond the end of treatment, making it a valuable long-term solution for individuals with chronic pain.[15][16][17][18][19]
Implementing Cognitive Behavioral Therapy in Chronic Pain Treatment
Chronic pain is a complex condition that can be difficult to manage. Cognitive Behavioral Therapy (CBT) is a type of therapy that is effective in reducing chronic pain. CBT is talk therapy that focuses on changing negative thought patterns and behaviors that can contribute to pain and disability.
If you are considering CBT for chronic pain, there are several things you should keep in mind:
Finding a Qualified Cognitive Behavioral Therapist
It is important to find a therapist who is trained in CBT and has experience working with individuals with chronic pain and psychiatric disorders. This will ensure that you receive the most effective treatment possible. You may want to ask your healthcare provider for recommendations of a licensed therapist or search for a therapist online.
It is also important to find a licensed therapist whom you feel comfortable with and whom you can trust to practice CBT with. Building a strong therapeutic relationship is essential for successful treatment.
Integrating CBT with Other Pain Management Strategies
CBT is most effective when used in conjunction with other pain management approaches, such as medication and physical therapy. Talk to your healthcare provider about developing a comprehensive treatment plan that includes multiple approaches.
It is important to remember that CBT is not a quick fix for chronic pain. It can take time to see improvements, and it is important to be patient and persistent in your treatment.
Tips for Success in CBT for Chronic Pain
To get the most out of CBT for chronic pain patients, it is important to:
- Be engaged and actively participate in therapy sessions. This means being open and honest with your therapist, asking questions, and practicing the skills you learn in therapy.
- Practice coping skills and strategies outside of therapy. CBT is most effective when you apply the skills you learn in therapy to your daily life. This may involve practicing relaxation techniques, challenging negative thoughts, or engaging in activities that please you.
- Be patient and persistent, as it may take time to see improvements. Chronic pain can be a challenging condition to manage, but with the right treatment and support, it is possible to improve your quality of life.
Overall, CBT can be a valuable tool in the treatment of chronic pain. By working with a qualified therapist and integrating CBT with other various pain management techniques and strategies, you can take control of your pain and improve your overall well-being.
Using the CareClinic App to Manage Pain
Having a pain diary is crucial for your health, and the CareClinic app can help with that. You can use the app as your health and clinical journal. Just go to the pain diary section of the app and enter your daily symptoms, medications, and other triggers, as they occur. There are also specific sections on the app to track each of these. This can help you be aware of early warning signs. The app is here to help you deal with your increased pain. Whether you suffer from chronic low back pain, chronic musculoskeletal pain, or other chronic pain syndromes due to tissue injury. The app also has a medication section where you can precisely track the pain therapies you are undergoing, whether it be internal medicine, psychological treatments, cognitive therapies, pain medicine, or other treatments.
CBT has shown promise as an effective approach to managing chronic pain. Ongoing research is exploring ways to personalize CBT for individual needs and to integrate it with other pain management approaches for optimal results. Ultimately, a holistic, patient-centered approach that combines multiple techniques may be the most effective way to manage chronic pain and improve overall quality of life. [20]
FAQs
What are the specific techniques used in CBT for chronic pain management?
How does CBT compare to medication in the treatment of chronic pain?
What can I expect in my first CBT session for chronic pain?
How long does it usually take to see improvements with CBT for chronic pain?
What role does mindfulness play in CBT for chronic pain?
References
- “Cognitive Behavioral Therapy (CBT) | Pain Management Education at UCSF”. https://pain.ucsf.edu/nonpharmacological-pain-management/cognitive-behavioral-therapy-cbt/
- “Association Between Psychological Interventions and Chronic Pain Outcomes in Older Adults: A Systematic Review and Meta-analysis | Pain Medicine | JAMA Internal Medicine | JAMA Network”. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2680318
- “Cognitive Behavioral Therapy for Pain Control – iResearchNet”. https://psychology.iresearchnet.com/health-psychology-research/arthritis/cognitive-behavioral-therapy-for-pain-control/
- “Chronic Pain Among Adults — United States, 2019–2021 | MMWR”. https://www.cdc.gov/mmwr/volumes/72/wr/mm7215a1.htm/
- “Chronic Pain – StatPearls – NCBI Bookshelf”. https://www.ncbi.nlm.nih.gov/books/NBK553030/
- “Impact of Chronic Pain on Patients’ Quality of Life: A Comparative Mixed-Methods Study – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC6558939/
- “Chronic Pain: What It Is, Symptoms, Treatment & Management”. https://my.clevelandclinic.org/health/diseases/4798-chronic-pain
- “Chronic Pain and Cognitive Behavioral Therapy: An Integrative Review – PubMed”. https://pubmed.ncbi.nlm.nih.gov/26604219/
- “10 Principles of Cognitive Behavior Therapy — Mind My Peelings”. https://www.mindmypeelings.com/blog/cbt-principles
- “Cognitive Behavioural Therapy for Chronic Non-Cancer Pain: A Review of Clinical Effectiveness – NCBI Bookshelf”. https://www.ncbi.nlm.nih.gov/books/NBK549547/
- “Cognitive-behavioral therapy increases prefrontal cortex gray matter in patients with chronic pain – PubMed”. https://pubmed.ncbi.nlm.nih.gov/24135432/
- “Chronic Pain | Fact Sheet – ABCT – Association for Behavioral and Cognitive Therapies”. https://www.abct.org/fact-sheets/chronic-pain/
- “Psychological therapies for the management of chronic pain | PRBM”. https://www.dovepress.com/psychological-therapies-for-the-management-of-chronic-pain-peer-reviewed-fulltext-article-PRBM
- “(CBT) Cognitive Behavioural Therapy – Chronic Pain Focus”. https://chronicpainfocus.com/cbt-cognitive-behavioural-therapy/
- “Efficacy of cognitive behavioral therapy for reducing pain susceptibility and increasing social engagement in patients with chronic low back pain: A systematic review and meta-analysis – PubMed”. https://pubmed.ncbi.nlm.nih.gov/37960716/
- “Guided internet-based cognitive-behavioral therapy for patients with chronic pain: A meta-analytic review”. https://pubmed.ncbi.nlm.nih.gov/36406977/
- “Effect of Medication Optimization vs Cognitive Behavioral Therapy Among US Veterans With Chronic Low Back Pain Receiving Long-term Opioid Therapy: A Randomized Clinical Trial | Physical Medicine and Rehabilitation | JAMA Network Open | JAMA Network”. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2798621
- “Effect of Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy or Usual Care on Back Pain and Functional Limitations in Adults With Chronic Low Back Pain: A Randomized Clinical Trial – PubMed”. https://pubmed.ncbi.nlm.nih.gov/27002445/
- “Cognitive behavioural therapy for a variety of conditions: an overview of systematic reviews and panoramic meta-analysis | NIHR Journals Library”. https://www.journalslibrary.nihr.ac.uk/hta/HTA25090
- “Cognitive-behavioral therapy for individuals with chronic pain: efficacy, innovations, and directions for research – PubMed”. https://pubmed.ncbi.nlm.nih.gov/24547801/
- “CBT for Chronic Pain: An Integrative Approach | Psychology Today”. https://www.psychologytoday.com/us/blog/the-man-cave/202108/cbt-for-chronic-pain-an-integrative-approach
- “Psychological therapies for the management of chronic pain – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC3986332/
- “Online CBT for chronic pain | Sevenoaks pain therapy | London pain treatment”. https://thinkcbt.com/cbt-for-chronic-pain