
Personality disorders are a complex and often misunderstood group of mental health disorders. Among them, two of the most well-known and widely studied are Antisocial Personality Disorder (ASPD) and Borderline Personality Disorder (BPD). While both disorders affect a person’s thoughts, emotions, and behaviors, they differ in several key ways.
In this article, we will provide a comprehensive comparative analysis of ASPD and BPD. Exploring their defining characteristics, prevalence, diagnosis, treatment options, and the challenges they present for mental health professionals. By shedding light on these disorders, we hope to enhance understanding and promote effective care for individuals living with ASPD and BPD.[1][2]
Understanding Personality Disorders
Personality disorders are characterized by enduring patterns of inner experience and behavior that significantly deviate from societal norms. These patterns typically manifest during adolescence or early adulthood and cause distress or impaired functioning in various areas of life. Individuals with personality disorders experience challenges in their self-perception, relationships, and emotional stability.
Let’s delve deeper into the different types of personality disorders. One common type is borderline personality disorder, which is characterized by unstable emotions, impulsive behaviors, and intense relationships. People with BPD often struggle with a fragile sense of self and have difficulty regulating their intense emotions. Another type is antisocial personality disorder (ASPD), which is characterized by a disregard for the rights of others, a lack of empathy, and a tendency towards manipulative and exploitative behaviors.
Prevalence of Personality Disorders
Personality disorders are more prevalent than commonly believed. With estimates suggesting that 10 to 15 percent of the general population may meet the criteria for one or more personality traits or disorders. Both ASPD and BPD are relatively common, although their prevalence rates vary. ASPD affects approximately 0.2 to 3.3 percent of the population, while BPD is estimated to impact 1.4 to 5.9 percent of individuals.
It is important to note that the prevalence rates of personality dimensions can vary depending on various environmental factors. Such as cultural differences, diagnostic criteria, and access to mental health services. Additionally, it is crucial to remember that these disorders exist on a spectrum. With individuals experiencing varying degrees of impairment and symptoms. Seek treatment from professionals and support is essential for individuals with personality disorders to manage their symptoms and improve their overall well-being.[3]
Characteristics of Antisocial Personality Disorder
ASPD is characterized by extreme emotions and a persistent disregard for the rights of others, along with an absence of empathy and remorse. Individuals with ASPD tend to exhibit a range of concerning behaviors. Including deceitfulness, impulsivity, aggression, and a consistent pattern of disregarding societal norms and laws. These features can often lead to significant difficulties in interpersonal relationships and legal issues.
One of the key characteristics of individuals with ASPD is their tendency to manipulate others for personal gain. They are skilled at charming people and using their charisma to exploit others for their own benefit. This manipulative behavior often allows them to navigate social situations with ease. But it comes at the expense of others’ well-being.
Another important aspect of ASPD is the lack of remorse or guilt. Individuals with this disorder do not feel remorse for their actions. No matter how harmful or destructive they may be. This absence of guilt enables them to engage in unethical or criminal behaviors and illegal activities without experiencing any emotional distress.
Diagnosis and Treatment of Antisocial Personality Disorder
Diagnosing ASPD typically involves a comprehensive assessment by a mental health professional. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and DSM-IV personality disorders outline the diagnostic criteria. Which includes the presence of conduct disorder symptoms before the age of 15 and a consistent pattern of antisocial behavior. While there is no cure for ASPD, various treatment approaches can be helpful in managing symptoms. Psychotherapy and cognitive-behavioral interventions may help individuals develop adaptive strategies and learn healthier ways of relating to others.
It is important to note that individuals with ASPD often have a poor prognosis for treatment success. Their lack of empathy and resistance to change make it challenging for therapists to establish a therapeutic alliance and engage them in the treatment process. Additionally, some research suggests that individuals with ASPD may be prone to substance abuse. Further complicating their treatment journey.[4]
Symptoms of Borderline Personality Disorder
Borderline Personality Disorder is a complex mental illness that affects approximately 1.6% of the population. It is characterized by emotional dysregulation, unstable relationships, and a distorted or poor self image-image. Individuals with BPD often experience intense mood swings, fear of abandonment, impulsivity, and an unstable sense of self. These symptoms can significantly impact various aspects of life, including work, relationships, and overall well-being.
One of the hallmark symptoms of BPD is emotional dysregulation. This means that individuals with BPD may have difficulty managing their emotions. Leading to intense and often unpredictable mood swings. For example, they may go from feeling extremely happy and elated to suddenly becoming overwhelmed with sadness or anger management. These emotional fluctuations can make it challenging for individuals with BPD to maintain stable relationships and can also impact their ability to function in day-to-day life.
Therapeutic Approaches for Borderline Personality Disorder
 The treatment of BPD usually involves a combination of group therapy, psychotherapy, medication, and self-help strategies. Dialectical Behavior Therapy (DBT) is a widely recognized and evidence-based treatment approach for BPD. Developed by psychologist Marsha M. Linehan, DBT aims to enhance emotional regulation, develop interpersonal effectiveness, and cultivate mindfulness skills.
The treatment of BPD usually involves a combination of group therapy, psychotherapy, medication, and self-help strategies. Dialectical Behavior Therapy (DBT) is a widely recognized and evidence-based treatment approach for BPD. Developed by psychologist Marsha M. Linehan, DBT aims to enhance emotional regulation, develop interpersonal effectiveness, and cultivate mindfulness skills.
During DBT, individuals with BPD learn various coping mechanisms and skills to manage their emotions effectively. These skills include mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. By learning and practicing these skills, individuals with BPD can gain better control over their emotions, improve their relationships, and enhance their overall well-being.
In addition to therapy, medication can also be prescribed to help manage specific symptoms of BPD, such as depression, anxiety, or impulsivity. Medications like antidepressants, mood stabilizers, and antipsychotics may be used in conjunction with psychotherapy to provide comprehensive treatment.
Self-help strategies can also play a crucial role in managing BPD symptoms. For example, maintaining a structured routine can help individuals with BPD feel more grounded and in control. Engaging in stress-reducing techniques, such as deep breathing exercises or journaling, can also provide relief during moments of emotional distress. Additionally, practicing self-care activities, such as engaging in hobbies or spending time in nature, can help individuals with BPD nurture their overall well-being.
It is important to remember that BPD is a highly treatable condition, and with the right support and resources, individuals with BPD can lead fulfilling and meaningful lives. If you or someone you know is struggling with BPD, reaching out to a mental health professional is the first step towards finding effective treatment and support.[5]
Comparing Antisocial and BPD
Antisocial Personality Disorder and Borderline Personality Disorder may seem two distinct conditions at first glance. But upon closer examination, we can uncover some intriguing similarities between the two. Both disorders share common features same traits that can significantly impact an individual’s life.
One striking similarity is the presence of impulsivity in both ASPD and BPD. Individuals with these disorders often struggle with acting on impulse without considering the potential consequences. This impulsivity can manifest in various ways, such as engaging in risky behaviors, making impulsive decisions, or having difficulty controlling their emotions.
Another shared characteristic is the challenge of maintaining stable relationships. Both ASPD and BPD can make it challenging for individuals to establish and sustain healthy connections with others. The interpersonal difficulties experienced by those with these disorders can stem from their emotional dysregulation. This can cause intense mood swings and unpredictable behavior.
Similarities Between Antisocial and Borderline Personality Disorders
Furthermore, individuals with ASPD and BPD may find themselves engaging in increased risk-taking behaviors. The impulsivity and emotional instability associated with these disorders can lead individuals to seek out thrill-seeking experiences or engage in behaviors that others might perceive as reckless or dangerous.
Additionally, difficulties in social functioning and a lack of empathy are prevalent in both disorders. Individuals with ASPD and BPD may struggle to navigate social situations effectively, often experiencing challenges in understanding and interpreting social norms and cues. These difficulties can further isolate individuals and contribute to their overall distress.
Key Differences Between Antisocial and Borderline Personality Disorders
While ASPD and BPD share some commonalities, it is crucial to recognize their fundamental differences. These differences lie in the core characteristics that define each disorder, shedding light on the distinct challenges faced by individuals living with ASPD and BPD.
ASPD is characterized by a lack of empathy and indifference towards the welfare of others. Individuals with ASPD often display a pattern of exploiting and manipulating individuals for personal gain. Their primary focus is on fulfilling their own needs and desires, with self-harming behaviors often disregarding the impact of self-harm and their actions on others.
In contrast, BPD is marked by emotional instability, an intense fear of abandonment and emotional abuse, and a fragile sense of very low self-esteem. Individuals with BPD often experience extreme emotional highs and lows, struggling to regulate their emotions effectively. The fear of abandonment can lead to desperate efforts to avoid real or perceived rejection, which can strain relationships and contribute to a tumultuous inner world.
Understanding these distinctions is crucial in providing appropriate support and treatment for individuals with ASPD and BPD. By recognizing the unique challenges faced by each person developing each disorder, mental health professionals can tailor interventions that address the specific needs of individuals living with these conditions.[6][7][8]
Challenges in Diagnosing Antisocial and Borderline Personality Disorders
Diagnosing both Antisocial Personality Disorder (ASPD) and Borderline Personality Disorder (BPD) can be challenging due to overlapping symptoms and comorbidity with other mental health conditions. Mental health professionals must conduct a thorough assessment to differentiate between the two disorders. They consider the individual’s overall clinical picture, family history, and social context.
When it comes to diagnosing ASPD, mental health professionals often face difficulties due to the deceptive and manipulative nature of individuals with this disorder. These individuals may present themselves as charming and charismatic, making it challenging to identify the underlying antisocial behaviors. Moreover, the comorbidity of ASPD with other mental health conditions, such as substance abuse or mood disorders, further complicates the diagnostic process.
On the other hand, diagnosing BPD can also pose significant challenges. The symptoms of BPD, such as emotional instability, impulsivity, and intense fear of abandonment, can overlap with other mental health disorders, making it crucial for mental health professionals to carefully assess and differentiate between them. Additionally, individuals with BPD often experience rapid mood swings and have a history of unstable relationships, risk factors that can further complicate the diagnostic process.
Strategies for Treating Antisocial Personality Disorders
Treating ASPD and BPD often requires a multidimensional approach, including psychotherapy, medication (when appropriate), and support from family member and a mental health team. However, due to the unique challenges associated with each disorder, tailored treatment plans are necessary.
For individuals with ASPD, psychotherapy can focus on developing empathy, improving impulse control, and addressing the underlying emotional deficits. Cognitive-behavioral therapy (CBT) has shown promising results in helping individuals with ASPD recognize and modify their maladaptive behavior patterns. Additionally, medication may be prescribed to manage comorbid antisocial conditions, such as depression or anxiety, that often accompany ASPD.
Strategies for Treating Borderline Personality Disorders
 When it comes to BPD treatment, dialectical behavior therapy (DBT) has emerged as one of the most effective treatment approaches. DBT combines individual therapy, group skills training, and phone coaching to help individuals regulate their emotions, improve interpersonal relationships, and develop coping mechanisms. Medication, such as mood stabilizers or antidepressants, may also be prescribed to manage specific symptoms associated with BPD.
When it comes to BPD treatment, dialectical behavior therapy (DBT) has emerged as one of the most effective treatment approaches. DBT combines individual therapy, group skills training, and phone coaching to help individuals regulate their emotions, improve interpersonal relationships, and develop coping mechanisms. Medication, such as mood stabilizers or antidepressants, may also be prescribed to manage specific symptoms associated with BPD.
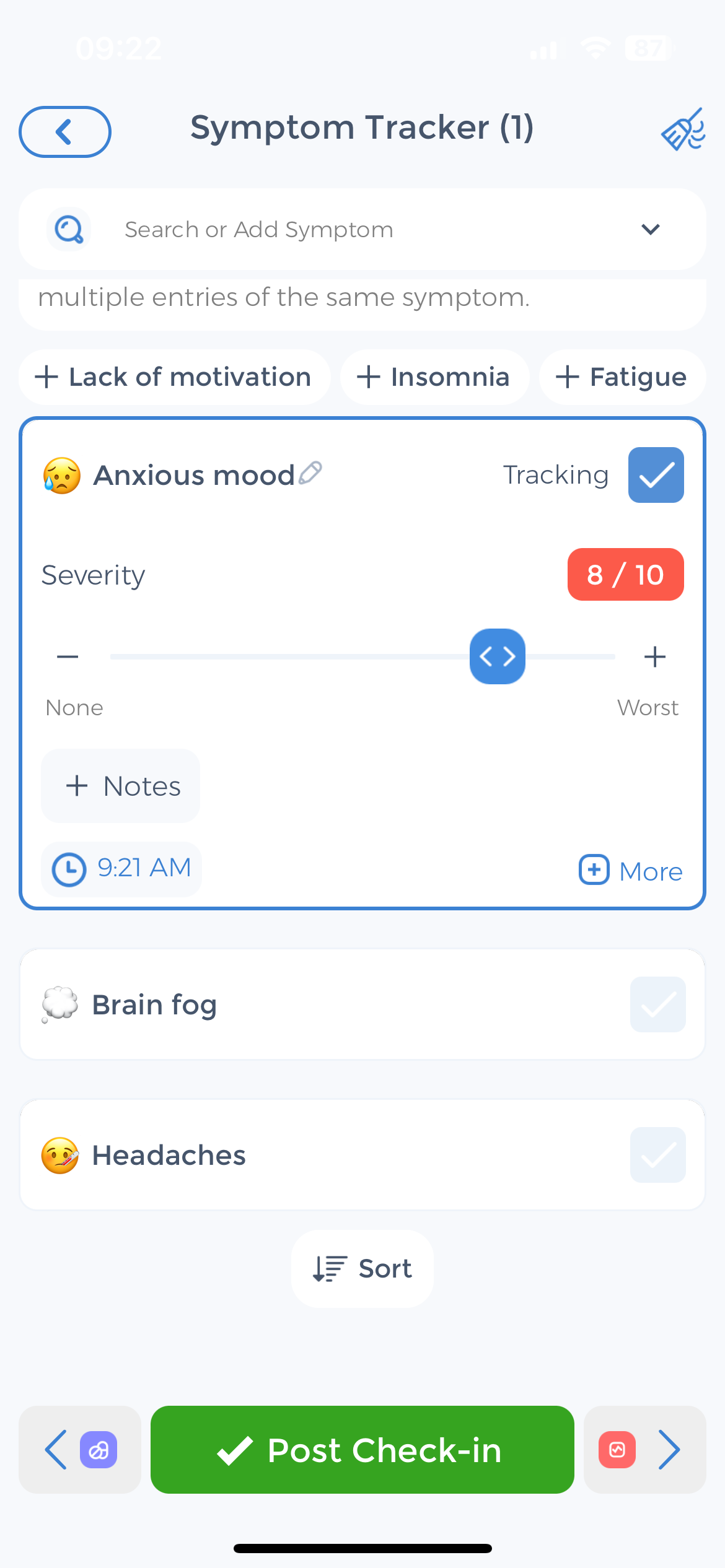
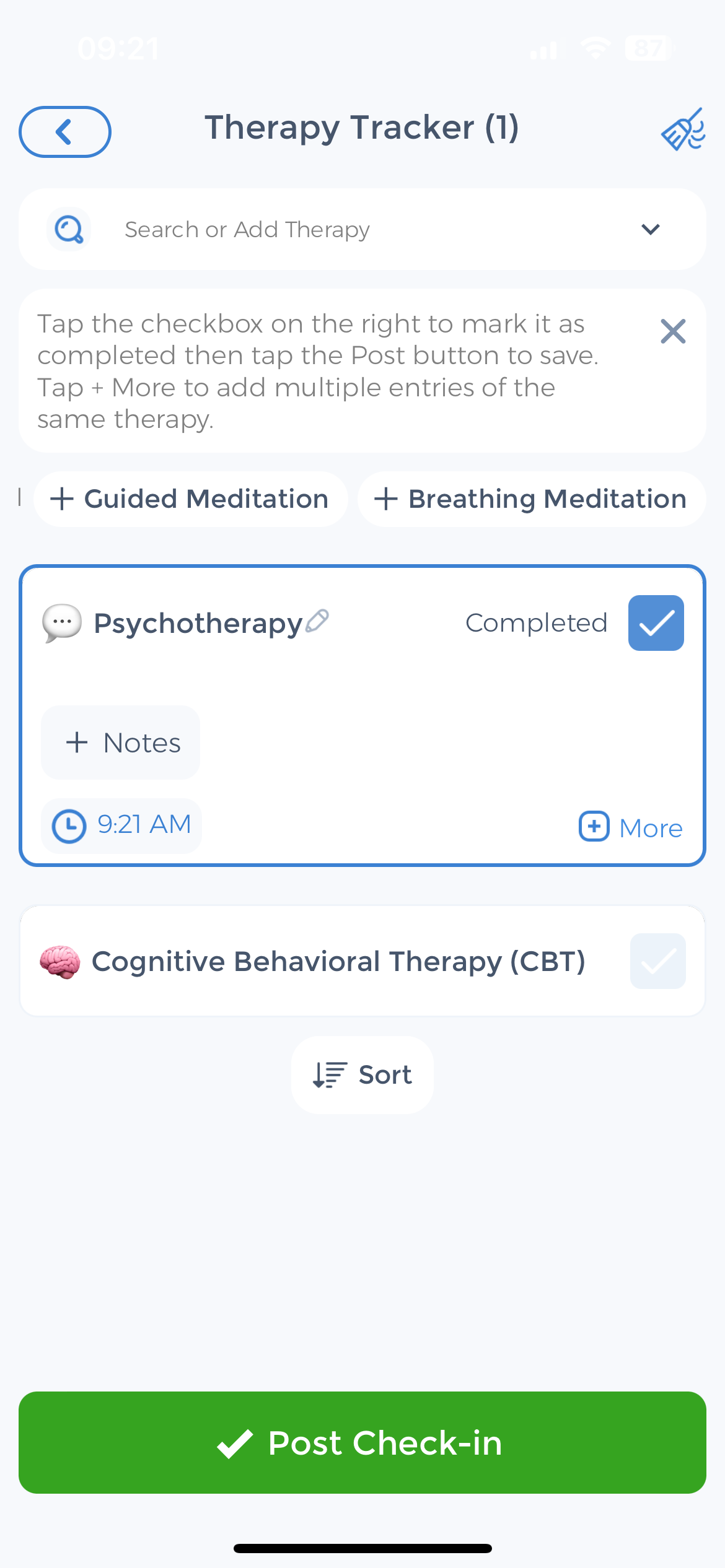
In addition to professional treatment, individuals living with ASPD or BPD can benefit from actively engaging in self-care practices. This may include maintaining a stable routine, engaging in stress-reducing activities such as exercise or meditation, and seeking social support from trusted individuals. Utilizing comprehensive self-care platforms like the CareClinic App can aid in tracking symptoms, medication adherence, and overall well-being.
By expanding their knowledge and understanding of ASPD and BPD, mental health professionals can provide more effective care and support for individuals living with these disorders. It is through ongoing research, collaboration, and a compassionate approach that we can continue to further improve outcomes and the well-being and quality of life for those affected by ASPD and BPD.
Use the CareClinic App to Manage Symptoms of Antisocial Personality Disorders
If you’re navigating the complexities of Antisocial Personality Disorder or Borderline Personality Disorder, the CareClinic App can be an invaluable tool in your journey toward better health. With features designed to track mood changes, medication adherence, and therapy progress, the app provides a comprehensive platform to manage the intricacies of these mental disorders. By consistently logging your experiences and treatment responses, you can gain insights into patterns and triggers, enabling you and your healthcare provider to make informed adjustments to your care plan.
Download the CareClinic App and Track Behavioral Differences
The CareClinic App also offers the ability to set reminders for medication and therapy sessions, ensuring that you stay on track with your treatment regimen. This level of organization can lead to improved health outcomes and a greater sense of control over your well-being. Embrace the support that technology can provide; take the next step in managing your mental health by installing the CareClinic App today.
References
- “Borderline personality disorder”. https://en.wikipedia.org/wiki/Borderline_personality_disorder
- “Management of borderline personality disorder”. https://en.wikipedia.org/wiki/Management_of_borderline_personality_disorder
- “Personality Disorders – National Institute of Mental Health (NIMH)”. https://www.nimh.nih.gov/health/statistics/personality-disorders
- “What is Antisocial Personality Disorder? | SAMHSA”. https://www.samhsa.gov/mental-health/what-is-mental-health/conditions/antisocial-personality-disorder
- “Dialectical behavior therapy as treatment for borderline personality disorder – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC6007584/
- “Self-reported impulsivity in women with borderline personality disorder: the role of childhood maltreatment severity and emotion regulation difficulties | Borderline Personality Disorder and Emotion Dysregulation | Full Text”. https://bpded.biomedcentral.com/articles/10.1186/s40479-019-0101-8
- “Antisocial and borderline personality disorders revisited”. https://pubmed.ncbi.nlm.nih.gov/23200574/
- “[Impulse control disorders in borderline and antisocial personality disorder]”. https://pubmed.ncbi.nlm.nih.gov/17619383/
- “Antisocial and borderline personality disorders: two separate diagnoses or two aspects of the same psychopathology? – PubMed”. https://pubmed.ncbi.nlm.nih.gov/9202881/
- “Diagnosing borderline personality disorder: Avoid these pitfalls | MDedge”. https://www.mdedge.com/psychiatry/article/264397/personality-disorders/diagnosing-borderline-personality-disorder-avoid


