Gastroparesis, a condition characterized by delayed emptying of the stomach, can cause various uncomfortable symptoms such as nausea, bloating, and abdominal pain. While there is no known cure for gastroparesis, managing symptoms through a well-designed diet can make a significant difference in your overall quality of life. In this article, we will explore effective gastroparesis diet tips that can help you alleviate your symptoms and improve your daily life.
Understanding Gastroparesis: Causes and Symptoms
Gastroparesis can be caused by a variety of factors, including diabetes, nerve damage, and certain medications. The condition occurs when the muscles in the stomach fail to contract properly, leading to delayed gastric emptying. As a result, food and fluids stay in the stomach for an extended period, causing symptoms such as nausea, vomiting, early satiety, and bloating.
If you suspect you have gastroparesis, it’s crucial to consult with your healthcare provider for a proper diagnosis and treatment plan. They may recommend diagnostic tests, such as gastric emptying studies or endoscopy, to confirm the condition and determine its underlying cause.
When it comes to managing gastroparesis, diet plays a vital role in symptom control. A well-designed gastroparesis diet can help reduce symptoms, improve digestion, and enhance your overall well-being.
Furthermore, in addition to dietary modifications, medications may also be prescribed to help manage symptoms associated with gastroparesis. These medications can include prokinetics, which help improve stomach emptying, and antiemetics, which help control nausea and vomiting.
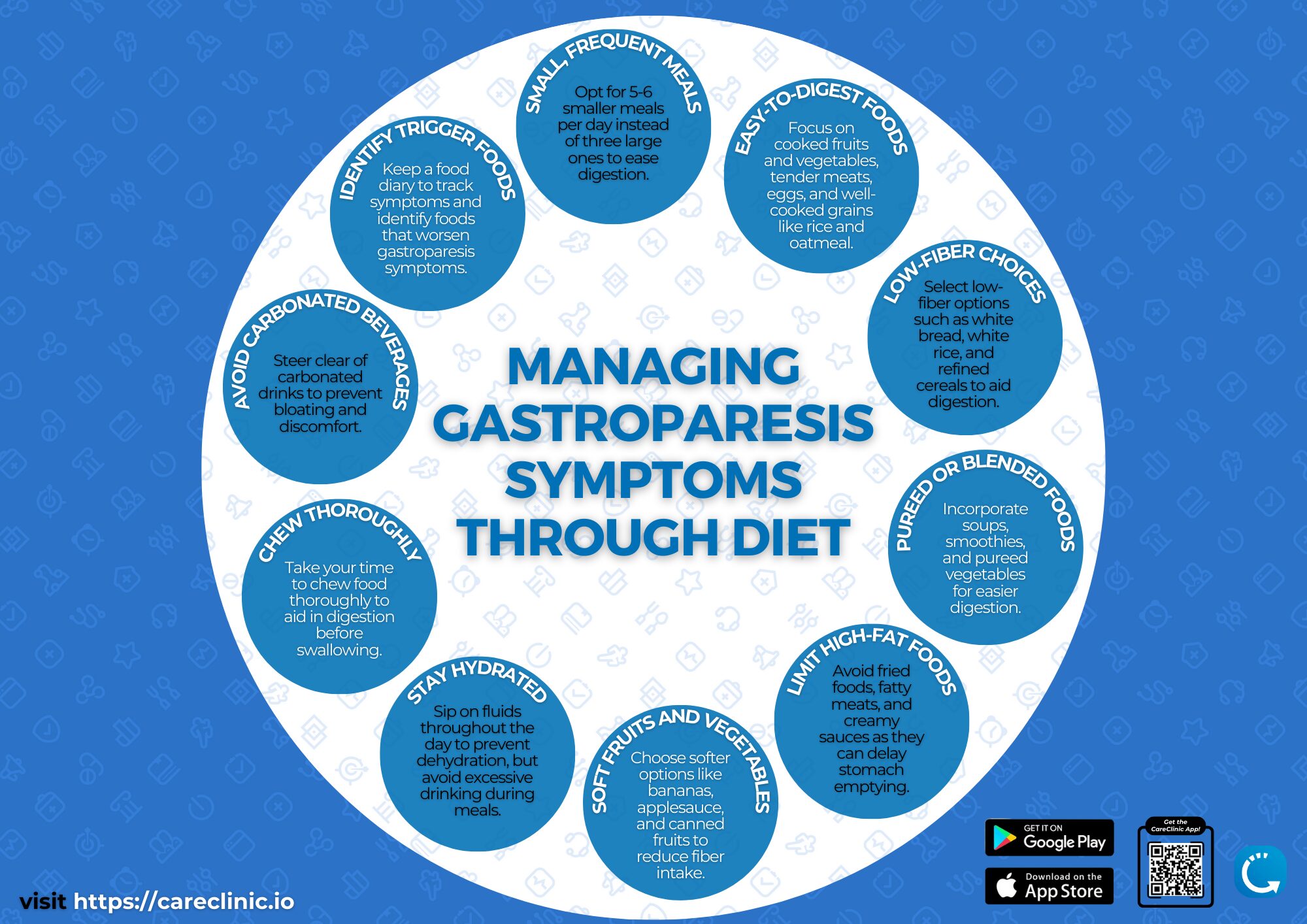
It is important for individuals with gastroparesis to eat smaller, more frequent meals to alleviate symptoms. Avoiding high-fat and high-fiber foods can also help prevent exacerbation of symptoms. Additionally, staying hydrated and engaging in light physical activity, such as walking, can aid in promoting digestion and reducing discomfort.
The Role of Diet in Managing Gastroparesis
A gastroparesis diet focuses on consuming foods that are easy to digest and pass through the stomach more quickly. By choosing the right foods, you can minimize the symptoms associated with delayed gastric emptying and promote optimal digestion. Here are some essential components of a gastroparesis diet:
When it comes to managing gastroparesis, it’s not just about what you eat, but also how you eat. Taking the time to thoroughly chew your food and savor each bite can greatly aid in digestion. This allows your stomach to break down the food more effectively, making it easier for your body to absorb the nutrients. Additionally, taking small bites and eating slowly can help prevent discomfort and reduce the risk of triggering symptoms.
Foods to Include in Your Gastroparesis Diet
Incorporating certain foods into your gastroparesis diet can help alleviate symptoms and provide much-needed nutrition. Here are some examples of foods that are generally well-tolerated:
- Low-fiber fruits and vegetables, such as bananas, melons, and cooked carrots. These options are gentle on the stomach and provide essential vitamins and minerals.
- Lean proteins, including chicken, fish, and tofu. These protein sources are easier to digest compared to fatty meats, making them ideal for individuals with gastroparesis.
- Soft, easily digestible grains like white rice and mashed potatoes. These options provide energy without putting excessive strain on the digestive system.
- Healthy fats, such as avocado and olive oil. These fats are easier to process and can help promote satiety and overall well-being.
- Low-fat dairy products, like yogurt and cottage cheese. These dairy options are generally well-tolerated and can provide a good source of calcium and protein.
Remember to chew your food thoroughly and take small bites to aid in digestion. Avoiding large meals and opting for smaller, more frequent meals throughout the day can also help manage symptoms.
Foods to Avoid for Gastroparesis Management
While certain foods can benefit individuals with gastroparesis, others can exacerbate symptoms and should be avoided. Here are some foods you may want to limit or avoid:
- Fatty, greasy foods that are harder to digest. These types of foods can slow down the digestion process and lead to discomfort.
- Foods high in fiber, such as whole grains and raw vegetables. While fiber is generally considered healthy, it can be difficult to digest for individuals with gastroparesis.
- Carbonated beverages and alcohol, which can cause bloating and discomfort. These drinks can further delay gastric emptying and worsen symptoms.
- Spicy foods that may irritate the stomach. The heat from spices can trigger symptoms and cause discomfort for individuals with gastroparesis.
- Caffeinated beverages, as they can stimulate gastric acid production. This can lead to increased stomach acid and potential irritation.
By avoiding these trigger foods, you can minimize symptoms and optimize your digestion process. Remember, everyone’s tolerance to different foods may vary, so it’s important to listen to your body and make adjustments accordingly.
Overall, managing gastroparesis through diet involves making mindful choices and paying attention to how your body responds to different foods. By following a gastroparesis diet that focuses on easy-to-digest options and avoiding trigger foods, you can help alleviate symptoms and improve your overall well-being.
Meal Planning and Portion Control for Gastroparesis
In addition to carefully selecting the right foods, meal planning and portion control are essential aspects of managing gastroparesis. Implementing the following strategies can greatly improve your symptoms:
Importance of Small, Frequent Meals
 Instead of having three large meals a day, aim to consume smaller, more frequent meals throughout the day. This approach helps ease the burden on your digestive system and prevents excessive stomach distention, which can worsen symptoms. Consider dividing your daily food intake into five to six small meals.
Instead of having three large meals a day, aim to consume smaller, more frequent meals throughout the day. This approach helps ease the burden on your digestive system and prevents excessive stomach distention, which can worsen symptoms. Consider dividing your daily food intake into five to six small meals.
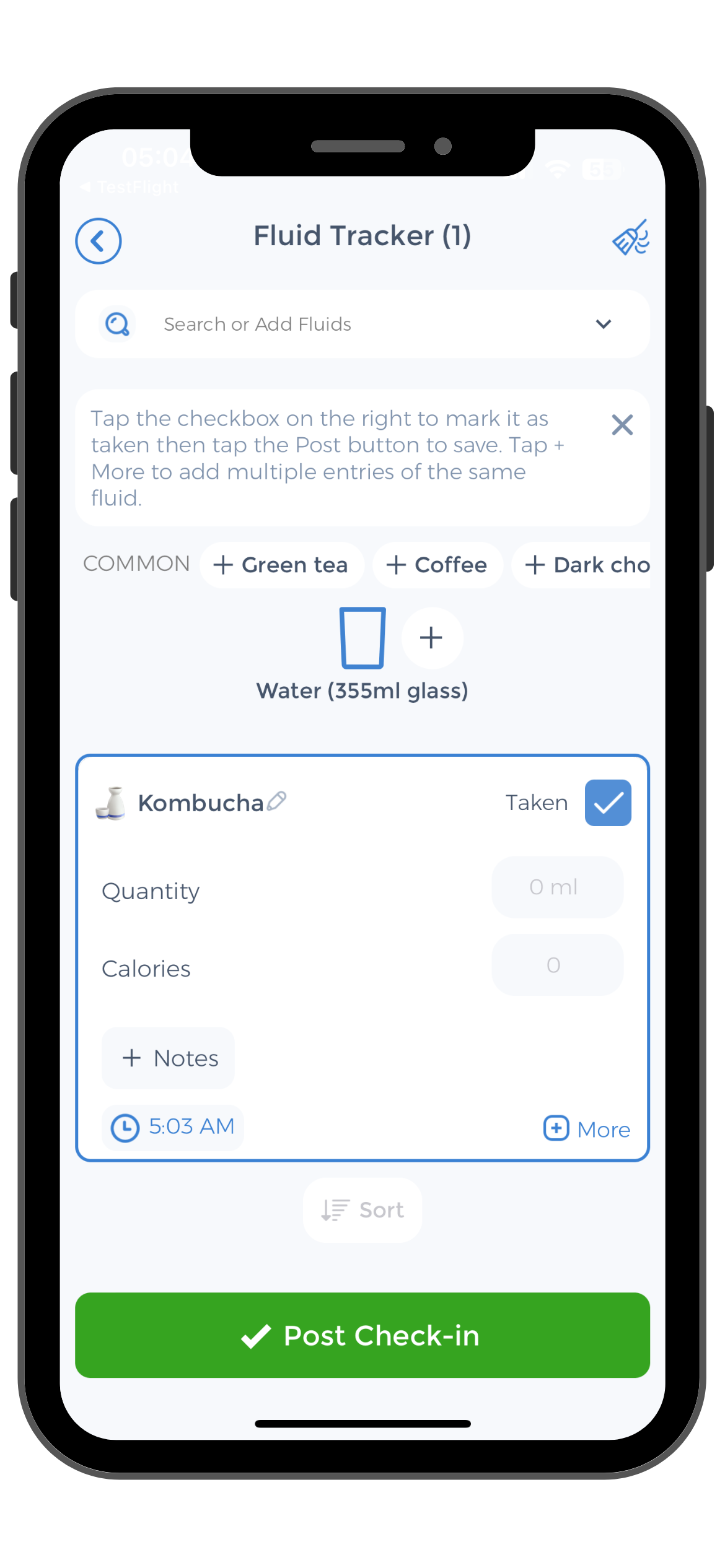
The CareClinic App can be an excellent tool for scheduling and tracking your meals. With its user-friendly interface and customizable reminders, it can help you establish a consistent eating routine tailored to your specific needs. Remember to consult your healthcare provider or a registered dietitian to develop a meal plan that suits you best.
When planning your small, frequent meals, it’s important to focus on nutrient-dense foods that are gentle on the stomach. Opt for easily digestible options such as lean proteins like chicken or fish, cooked vegetables, and soft fruits. These choices provide essential vitamins and minerals while minimizing the strain on your digestive system.
Furthermore, incorporating a variety of colors and textures into your meals can make them more appealing and enjoyable. Experiment with different cooking methods, such as steaming or baking, to enhance the flavors and textures of your dishes. Remember, meal planning for gastroparesis doesn’t have to be bland or boring!
The Role of Portion Control in Gastroparesis Management
Portion control is another key aspect of managing gastroparesis. By consuming smaller portions, you give your stomach ample time to empty, reducing the likelihood of symptoms. Here are some tips for practicing portion control:
- Use smaller plates and bowls to create the illusion of a fuller plate
- Avoid rushing through meals; take your time to savor each bite
- Avoid distractions, such as watching television or working while eating
By adopting mindful eating habits and focusing on portion control, you can maximize the effectiveness of your gastroparesis diet plan.
Additionally, it’s important to pay attention to your body’s hunger and fullness cues. Eating until you are comfortably satisfied, rather than overly full, can help prevent discomfort and promote better digestion. Remember, portion control is not about deprivation, but about finding the right balance for your individual needs.
Furthermore, incorporating regular physical activity into your routine can complement your portion control efforts. Engaging in low-impact exercises, such as walking or yoga, can aid in digestion and promote overall well-being. Consult with your healthcare provider before starting any new exercise regimen.
By implementing these strategies and making mindful choices, you can effectively manage your gastroparesis symptoms and improve your overall quality of life.
Hydration and Gastroparesis: The Connection
Proper hydration is crucial for maintaining overall well-being, and it becomes even more important when managing gastroparesis. Staying hydrated helps promote healthy digestion and prevents complications associated with dehydration. Here’s why hydration matters:
Importance of Staying Hydrated
Gastroparesis can cause fluid imbalances due to delayed gastric emptying. To compensate for potential fluid loss, it’s essential to drink adequate amounts of fluids throughout the day. Aim to consume at least eight cups (64 ounces) of fluid daily, or as recommended by your healthcare provider. Water, herbal teas, and clear broths are good choices for hydration.
Using the CareClinic App can be helpful for tracking your fluid intake and setting reminders to ensure you meet your daily hydration goals. Its intuitive interface and informative charts make monitoring your progress hassle-free.
Best Drinks for Gastroparesis Patients
 When choosing beverages, opt for those that are easily digestible and won’t exacerbate your symptoms. Here are some examples of drinks suitable for gastroparesis patients:
When choosing beverages, opt for those that are easily digestible and won’t exacerbate your symptoms. Here are some examples of drinks suitable for gastroparesis patients:
- Water: Plain water is always a great option to stay hydrated
- Herbal teas: Mild herbal teas such as chamomile or ginger can help soothe the stomach
- Low-acid fruit juices: Choose juices that are low in acidity, such as apple or pear juice
- Smoothies: Blending fruits and vegetables into a smoothie can provide healthful nutrients while being easier to digest
Remember to avoid carbonated beverages and those high in caffeine or alcohol, as these can worsen symptoms for many gastroparesis patients. Additionally, be cautious with dairy-based drinks, as they may be difficult to digest for some individuals. Experiment with different beverages and take note of how your body responds to find what works best for you. Always consult with your healthcare provider or a registered dietitian for personalized advice on managing gastroparesis symptoms through dietary choices.
Nutritional Supplements for Gastroparesis
In some cases, individuals with gastroparesis may struggle to meet their nutritional needs solely through their diet. In such instances, nutritional supplements can be a valuable addition to your self-care routine:
Essential Vitamins and Minerals for Gastroparesis
Individuals with gastroparesis may be at risk of nutrient deficiencies due to impaired digestion and reduced food intake. A healthcare professional can assess your nutritional status and recommend specific vitamins and minerals to supplement your diet.
For example, supplements of vitamin D, vitamin B12, and iron may be beneficial for some individuals with gastroparesis. However, it’s important to consult your healthcare provider before initiating any new supplements to ensure they are appropriate for your unique needs and medical history.
The Role of Probiotics in Gastroparesis Management
Probiotics, which are beneficial bacteria, have gained attention for their potential to support digestive health. While research specifically focused on gastroparesis is limited, incorporating probiotics into your routine may offer some benefits. Probiotics can help promote a healthy gut microbiome and improve overall digestion.
The CareClinic App can help you stay on top of your supplement routine by scheduling reminders and providing you with a personalized history of your supplement usage. It serves as an invaluable tool for self-care and tracking your progress.
Lifestyle Changes to Complement a Gastroparesis Diet
Exercise and Gastroparesis
Incorporating light to moderate exercise into your routine can have numerous benefits when managing gastroparesis. Exercise stimulates digestion, improves muscle contractions, and can help relieve some of the symptoms associated with delayed gastric emptying.
Engaging in low-impact activities such as walking, swimming, or gentle stretching can be beneficial. It’s important to listen to your body and start with activities that feel comfortable. Gradually increase intensity or duration as tolerated, always taking cues from your body’s response.
The CareClinic App allows you to track your exercise routine, set goals, and monitor your progress over time. It helps you maintain a consistent exercise schedule and prompts you to engage in physical activity when you might otherwise forget.
Stress Management and Gastroparesis
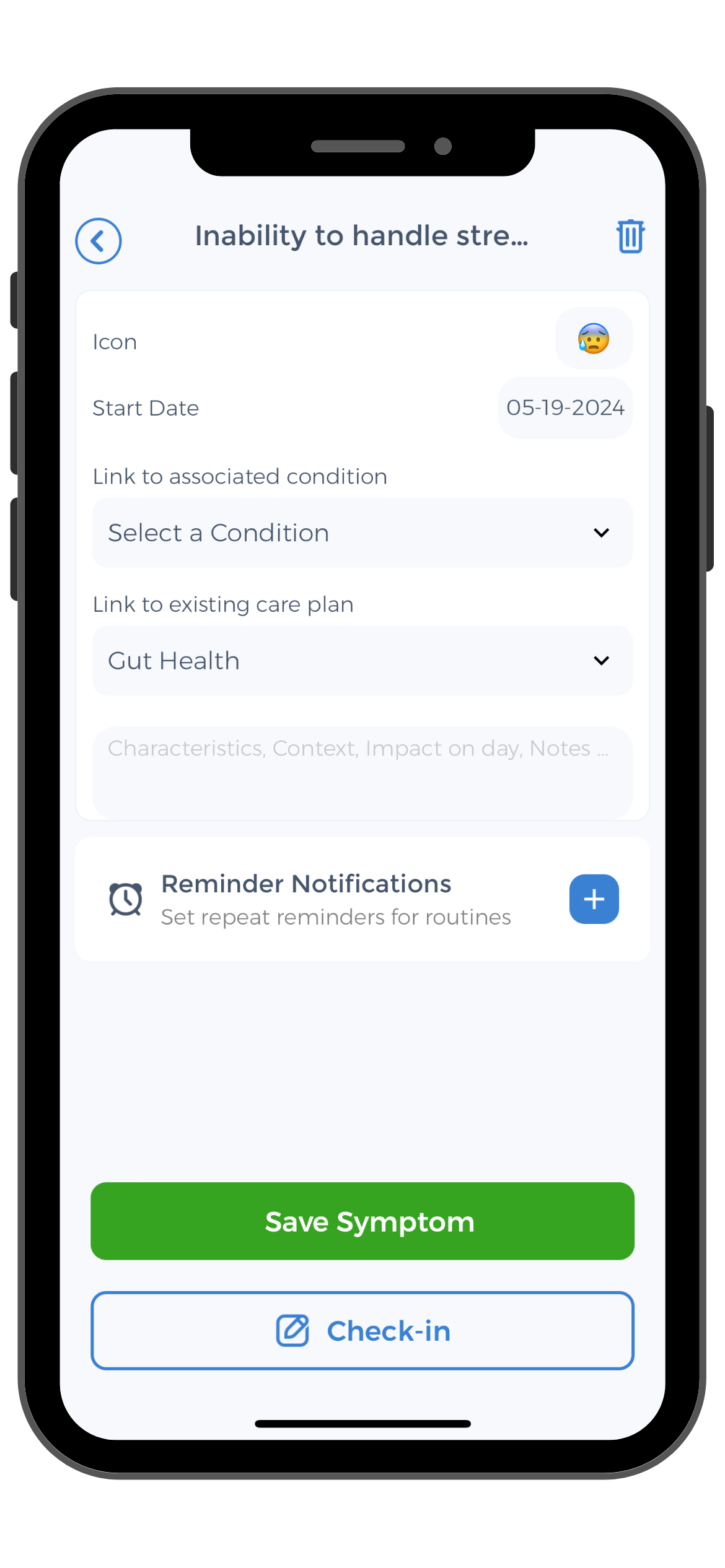 Stress can exacerbate gastrointestinal symptoms, including those associated with gastroparesis. Incorporating stress management techniques into your daily routine can have a positive impact on your symptoms and overall well-being.
Stress can exacerbate gastrointestinal symptoms, including those associated with gastroparesis. Incorporating stress management techniques into your daily routine can have a positive impact on your symptoms and overall well-being.
Explore relaxation techniques such as deep breathing exercises, meditation, or yoga. Additionally, taking time to engage in activities you enjoy, such as hobbies or spending time with loved ones, can help reduce stress levels and promote a sense of calm.
The CareClinic App includes a comprehensive set of features to support mental health and stress management. From mindfulness exercises to mood tracking, it serves as a valuable companion on your journey to optimal self-care.
Managing gastroparesis symptoms requires a multidimensional approach. By following an appropriate diet, practicing portion control, staying hydrated, considering nutritional supplements, and adopting lifestyle changes, you can take control of your symptoms and improve your overall well-being. Remember, it’s essential to consult with your healthcare provider or a registered dietitian for personalized advice and guidance. With the assistance of the CareClinic App, you can enhance your self-care journey and achieve better symptom management and overall health.
Use the CareClinic App to Manage Gastroparesis Symptoms
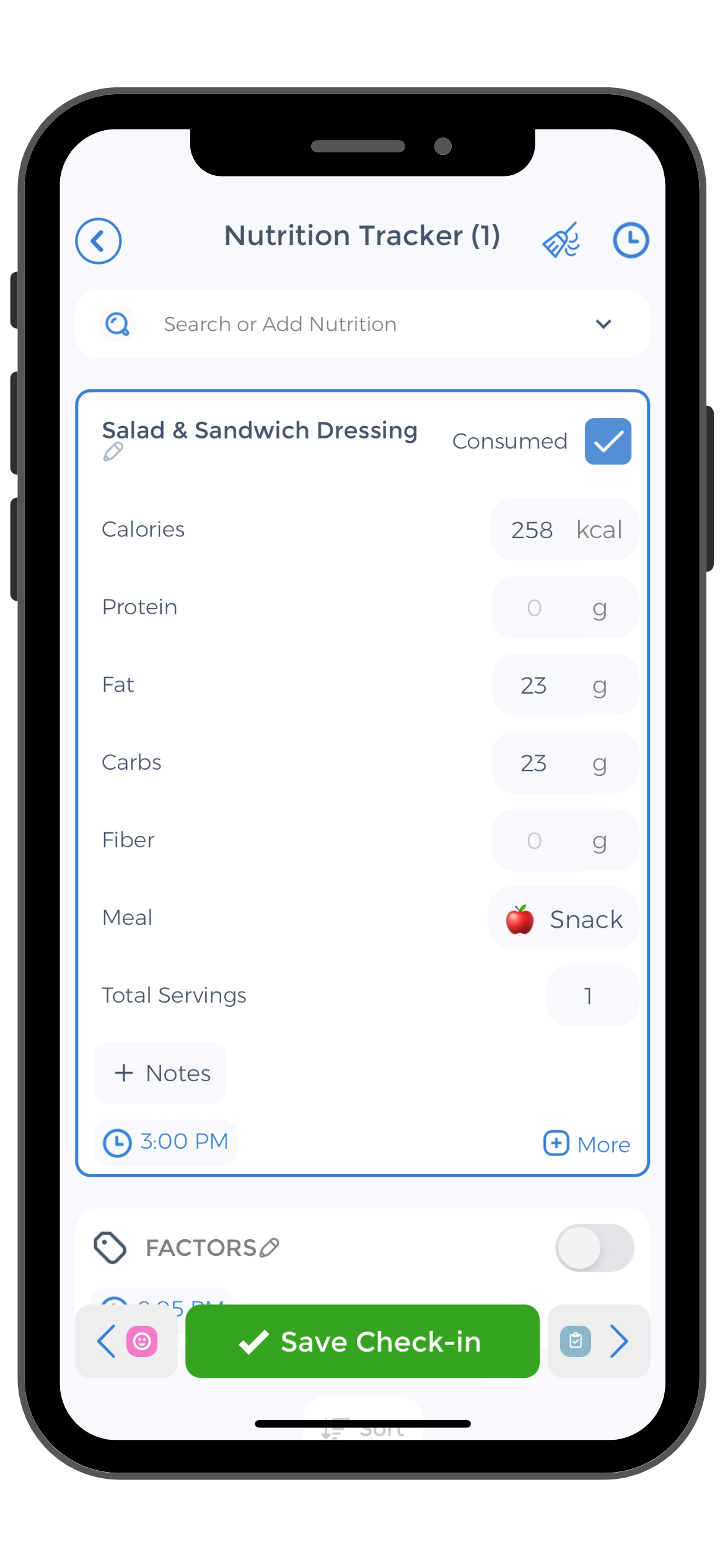
Take the next step in managing your gastroparesis symptoms with the CareClinic App. This comprehensive health app allows you to track your meals, hydration, and supplements, ensuring you stay on top of your gastroparesis diet. With features like customizable reminders and a user-friendly interface, the CareClinic App makes it easier to adhere to dietary recommendations and monitor your progress. By consistently using the app to manage your condition, you can identify patterns and make informed adjustments to your treatment plan.
Download the CareClinic App Today
Enhance your gastroparesis management by incorporating the CareClinic App into your daily routine. The app’s ability to track physical activity and stress management techniques provides a holistic approach to your health. Understand the impact of lifestyle changes on your symptoms and gain insights into what works best for you. To experience the benefits of optimized symptom management and improved health outcomes, Install App today.