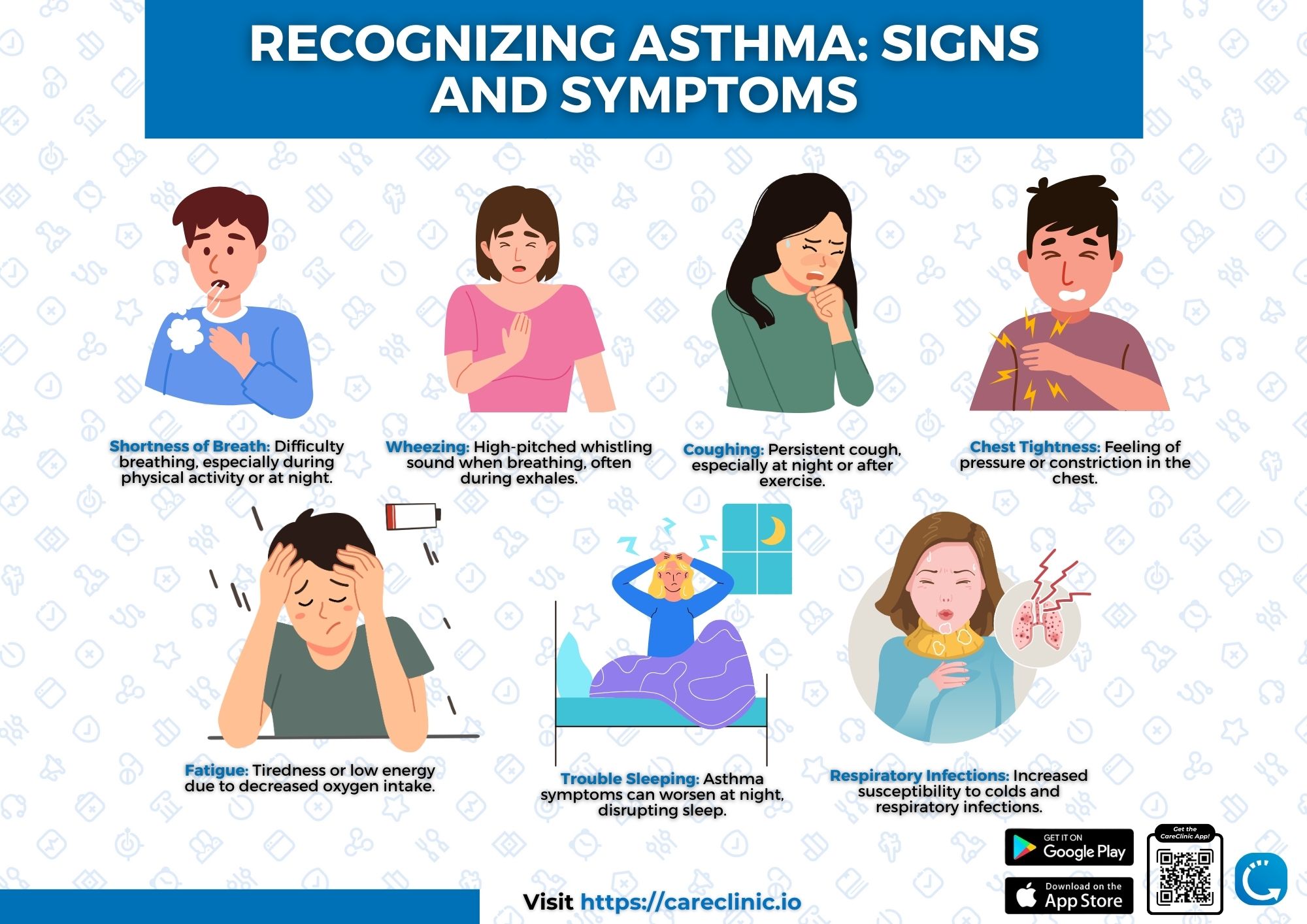
Asthma is a chronic respiratory condition that affects millions of people worldwide. It is characterized by inflammation and narrowing of the airways. Leading to recurring episodes of wheezing, coughing, chest tightness, and shortness of breath. While there is no cure for asthma, proper management can help control symptoms and prevent asthma attacks.
What is Asthma?
Asthma is a chronic respiratory disease that causes inflammation and narrowing of the airways. This leads to increased sensitivity to various triggers. Such as allergens, exercise, and irritants. When exposed to triggers, the airways become inflamed. Making it difficult for air to pass through, resulting in symptoms like wheezing, coughing, and shortness of breath.
The Basics of Asthma
Asthma is a complex condition with various underlying causes. It often begins in childhood but can develop at any age. Genetic and environmental factors both play a role in the development of asthma. Common risk factors include a family history of asthma, exposure to tobacco smoke, and respiratory infections during early childhood.
Managing asthma involves identifying and avoiding triggers, taking prescribed medications, and monitoring lung function through peak flow readings.
Common Triggers of Asthma
There are several common triggers that can worsen asthma symptoms. These can vary from person to person, so it’s important to identify your specific triggers. Some common triggers include:
- Allergens: Pollen, dust mites, pet dander, and mold can trigger asthma symptoms in allergic individuals.
- Exercise: Physical exertion can lead to shortness of breath and coughing in people with exercise-induced asthma.
- Irritants: Strong odors, air pollution, smoke, and strong chemicals can all trigger asthma symptoms.
- Infections: Common colds and respiratory infections can worsen asthma symptoms.
Living with asthma can be challenging, but with proper management, individuals can lead fulfilling lives. It is important to have a comprehensive asthma action plan in place, which includes regular check-ups with a healthcare provider, understanding how to use inhalers correctly, and knowing when to seek emergency medical care.
In addition to medication, there are also complementary therapies that can help manage asthma symptoms. These include breathing exercises, such as deep breathing and pursed-lip breathing, which can help improve lung function and reduce the severity of asthma attacks. Other complementary therapies include acupuncture, yoga, and herbal remedies, although it’s important to consult with a healthcare professional before trying any alternative treatments.
The Importance of Monitoring Asthma
Regular monitoring of asthma is essential to ensure optimal management and to prevent exacerbations. Monitoring involves keeping track of symptoms, medication use, and most importantly, peak flow readings.
Proper monitoring of asthma is not just about managing the condition when symptoms arise, but also about proactively staying ahead of potential triggers and complications. By closely monitoring your asthma, you can work with your healthcare team to develop a personalized action plan that addresses your specific needs and helps you maintain better control over your condition.
Role of Regular Check-ups
Regular check-ups with your healthcare provider are crucial for managing asthma effectively. During these visits, your healthcare provider will assess your symptoms, review your medications, and monitor your lung function. They may also adjust your treatment plan based on your current condition.
These check-ups serve as an opportunity for you to discuss any concerns or changes in your asthma symptoms with your healthcare provider. By maintaining a consistent schedule of check-ups, you can ensure that any developments in your condition are promptly addressed, and adjustments to your treatment plan can be made in a timely manner.
Self-Monitoring Techniques
 In addition to regular check-ups, self-monitoring plays a vital role in managing asthma. Self-monitoring allows you to track your symptoms, medication use, and lung function on a day-to-day basis.
In addition to regular check-ups, self-monitoring plays a vital role in managing asthma. Self-monitoring allows you to track your symptoms, medication use, and lung function on a day-to-day basis.
One effective way to self-monitor is by using a same peak flow meter. This handheld device measures best peak flow number the maximum airflow that you can exhale forcefully after taking a deep breath. Peak flow number readings can provide important insights into your lung function and help you identify any changes or worsening of symptoms.
Another self-monitoring technique that can be beneficial for individuals with asthma is keeping a symptom diary. By recording your symptoms, triggers, and medication use regularly, you can identify patterns and potential triggers that may exacerbate your asthma. This information can be valuable during check-ups with your healthcare provider, as it provides a detailed overview of your asthma management outside of the clinical setting.
Introduction to Peak Flow Reading
A peak flow meter is a simple device used to measure how well your lungs are working. It measures the force and speed of air as you exhale forcefully into the device. By using most peak flow meters and tracking your peak flow readings over time, you can get a better understanding of how well your asthma is controlled.
Regular monitoring of peak flow readings can provide valuable insights into your respiratory health and help you and your healthcare provider make informed decisions about your asthma management plan. It is a proactive approach that empowers individuals with asthma to take control of their condition and make timely adjustments to their treatment regimen.
What is a Peak Flow Meter?
A peak flow meter is a handheld device that you blow into to measure your peak expiratory flow (PEF). It consists of a tube with a scale and a movable indicator. The scale is measured in liters per minute (L/min) and the indicator moves based on highest peak flow number and on the force of your exhalation.
Peak flow meters come in various designs and sizes, but they all serve the same essential function of assessing lung function. Some of peak flow test meters are digital, providing precise numerical readings, while others have a simple mechanical design that relies on airflow to move the marker along the scale.
Understanding Peak Flow Readings
Peak flow readings are categorized into three zones: green, yellow, and red. These peak flow zones are based on your personal best peak flow value, which is determined when your asthma is well-controlled.
The green zone indicates good control and means that your asthma is well-managed. It is the range where you should ideally be most of the time. The yellow zone suggests caution and indicates that your asthma may be getting worse, prompting you to take action such as adjusting your medication or contacting your healthcare provider. The red zone signifies a medical emergency and requires immediate attention, as it indicates a severe decline in lung function and potentially life-threatening asthma exacerbation.
How to Use a Peak Flow Meter
Using a peak flow meter is a simple and effective way to monitor your lung function at home. Here is a step-by-step guide on how to use a peak flow meter:
Step-by-Step Guide:
- Stand up straight and make sure the indicator is at the bottom of the scale.
- Take a deep breath and place the mouthpiece of the peak flow meter in your mouth, sealing your lips tightly around it.
- Blow out as hard and as fast as you can into the device. Make sure there is no air leakage around your lips.
- Check the reading on the scale and record it.
- Repeat the test two more times, allowing a short break between each attempt.
- Use the highest reading of the three as your peak flow value.
Tips for Accurate Readings:
- Use the peak flow meter at the same time each day.
- Take your medication as prescribed before performing the test.
- Stand up straight and avoid leaning forward or backward during the test.
- Repeat the test three times and record the highest value.
 Peak flow meters are essential tools for individuals with asthma or other respiratory conditions. They measure how quickly you can expel air from your lungs, helping you and your healthcare provider monitor your lung function over time. Regular use of a peak flow meter can provide valuable insights into the effectiveness of your treatment plan and help you identify potential triggers that worsen your symptoms.
Peak flow meters are essential tools for individuals with asthma or other respiratory conditions. They measure how quickly you can expel air from your lungs, helping you and your healthcare provider monitor your lung function over time. Regular use of a peak flow meter can provide valuable insights into the effectiveness of your treatment plan and help you identify potential triggers that worsen your symptoms.
When using a peak flow meter, it’s important to maintain a consistent testing routine to ensure accurate and reliable results. Find a quiet and well-lit area to perform the test, as distractions and poor lighting can affect your technique and the readings. Remember to keep your peak flow meter clean by following the manufacturer’s instructions for proper maintenance and storage. Additionally, consider keeping a peak flow meter readings diary to track your readings and share them with your healthcare team during follow-up appointments.
Interpreting Your Peak Flow Readings
Understanding your peak flow readings is essential for managing your asthma effectively. Here’s a breakdown of what your peak flow readings mean:
What Your Readings Mean:
In the green zone, your lung function is good, and your asthma is well-controlled. You can continue with your regular activities and follow your treatment plan.
In the yellow zone, your lung function is moderate, and your asthma may be worsening. This is a signal to take action and consider adjusting your treatment plan, such as increasing your medication or contacting your healthcare provider for further guidance.
In the red zone, your lung function is significantly decreased, and you may be experiencing a severe asthma attack. This requires immediate medical attention. Follow your emergency action plan or seek medical help right away.
When to Seek Medical Help:
While self-monitoring with a peak flow meter is valuable, it’s important to find your personal best to know when to seek medical help:
- If your peak flow readings consistently fall in the yellow or red zone.
- If you experience severe asthma symptoms that don’t improve with rescue medication.
- If you notice a sudden drop in your peak flow readings or a significant increase in your asthma symptoms.
 It is crucial to remember that asthma is a chronic condition that requires ongoing management and monitoring. By regularly tracking and measuring your peak flow readings, you can gain valuable insights into the state of your lung function and the effectiveness of your treatment plan. However, peak flow readings alone do not provide a complete picture of your asthma control.
It is crucial to remember that asthma is a chronic condition that requires ongoing management and monitoring. By regularly tracking and measuring your peak flow readings, you can gain valuable insights into the state of your lung function and the effectiveness of your treatment plan. However, peak flow readings alone do not provide a complete picture of your asthma control.
It is recommended to keep a diary of your symptoms, triggers, and medication usage alongside your peak flow readings. This comprehensive approach allows you and your healthcare provider to identify patterns and make informed decisions about your asthma management. By analyzing the data from your peak flow readings, symptom diary, and medication usage, your healthcare provider can tailor your treatment plan to suit your specific needs.
Additionally, it’s important to understand that peak flow readings can vary throughout the day. Factors such as time of day, physical activity, exposure to triggers, and even emotions can influence other peak flow readings and your lung function. Therefore, it is advisable to measure your peak flow readings at consistent times each day, preferably before taking any asthma medicine, to obtain accurate and comparable results.
Top 3 Peak Flow Meters You Can Buy
Keeping track of your lung health is important, especially if you have asthma or other respiratory issues. A peak flow meter is a simple device that helps you measure how well your lungs are working by checking the speed of your breath. With many options available, it can be hard to know which one to choose. To help you out, we’ve picked the top 3 peak flow meters that are accurate, easy to use, and reliable. Whether you need one for personal use or for your medical practice, these are the best choices you can buy.
OMRON PeakAir Peak Flow Meter
The PeakAir Peak Flow Meter measures your Peak Expiratory Flow Rate (PEFR), or the highest speed you can blow air from your lungs. Recommended by healthcare professionals, this device helps you monitor changes in your airflow. Along with using the Peak Flow meter, your doctor will provide a treatment plan to guide your actions based on your readings.
 Buy OMRON PeakAir Peak Flow Meter Here
Buy OMRON PeakAir Peak Flow Meter Here
Nascool Digital Peak Flow Meter
This high-accuracy peak flow meter features a pressure differential sensor, ensuring precise measurements without the need for calibration. It meets ATS, ERS, and WRIGHT standards, and automatically displays Peak Expiratory Flow (PEF) and Forced Expiratory Volume in 1 second (FEV1). Compact, durable, and easy to clean, it doesn’t require disposable mouthpieces. An accompanying app helps track asthma management by recording symptoms, triggers, and medications, although data must be entered manually. Suitable for those monitoring their respiratory health, including asthma sufferers, people with respiratory issues or COPD, smokers, athletes, and children over 6.
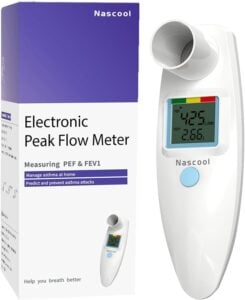 Buy Nascool Digital Peak Flow Meter Here
Buy Nascool Digital Peak Flow Meter Here
Microlife Digital Peak Flow Meter
The Microlife Digital Peak Flow Meter with FEV1 is a top choice for managing lung conditions, measuring air flow velocity and volume to detect early warning signs of asthma and other respiratory issues. Featuring a digital diary, it helps track lung performance and supports effective disease management when used alongside a doctor’s guidance, making it ideal for patients with asthma, COPD, and other lung diseases.
 Buy Microlife Digital Peak Flow Meter Here
Buy Microlife Digital Peak Flow Meter Here
Understanding asthma and use your peak flow and readings is an integral part of managing asthma effectively. By using a peak flow meter and monitoring your peak flow readings regularly, you can track changes in your lung function and take appropriate action to prevent asthma exacerbations. Remember to work closely with your healthcare provider to develop an individualized treatment plan that includes regular check-ups, self-monitoring techniques, and keeping a symptom diary. With proper management and self-care, you can live a full and active life, keeping your asthma symptoms under control.
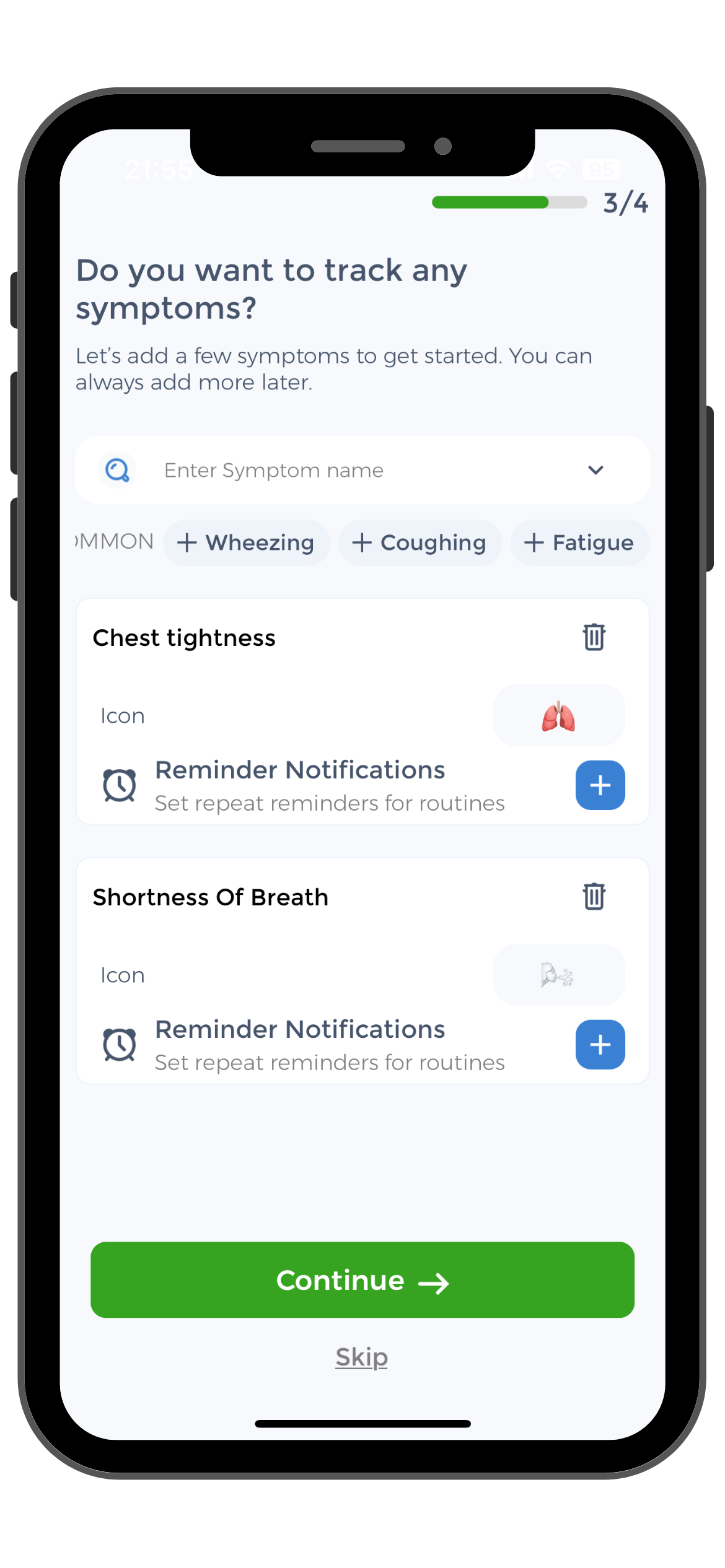
Use the CareClinic App for Asthma Peak Flow Meters Monitoring
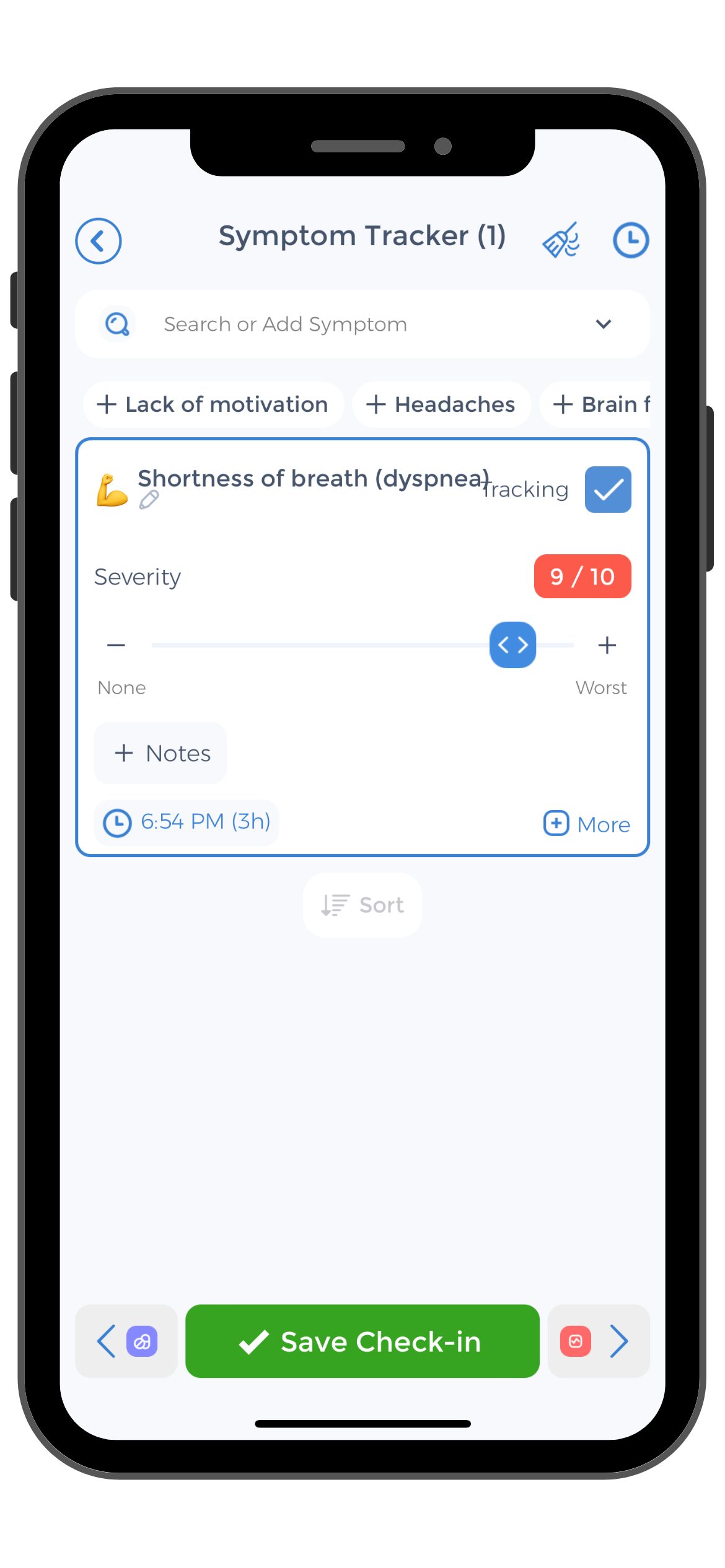
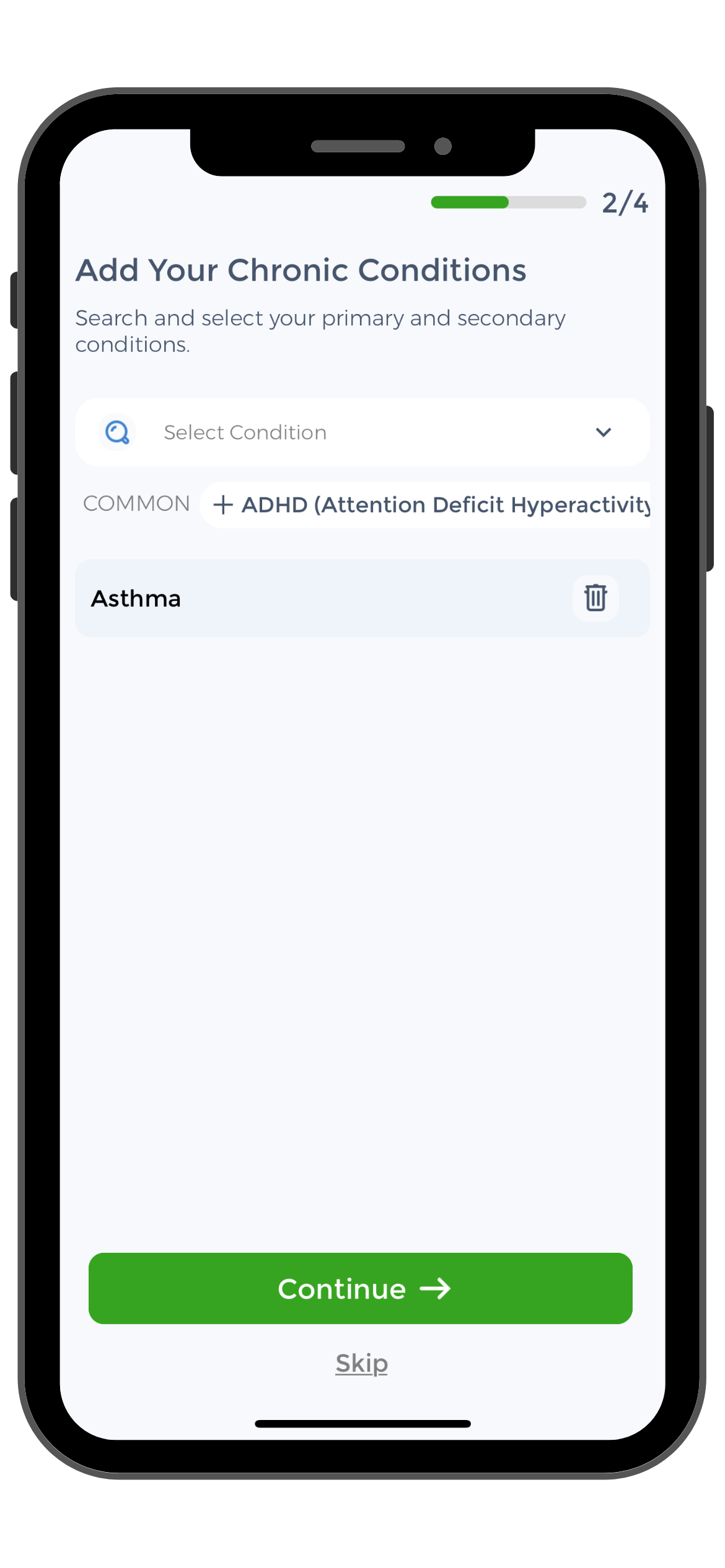
Take control of your asthma management with the CareClinic App, a comprehensive tool designed to help you monitor your peak flow values and manage your condition effectively. The app allows you to track your daily symptoms, and medication usage, and take your peak flow and readings all in one place, providing a clear picture of your asthma over time.
With features like medication reminders and personalized health reports, CareClinic ensures you stay on top of your asthma management plan. By consistently using the app, you can identify triggers, notice trends, and make informed decisions with your healthcare provider.
Download the CareClinic App Today
Experience the benefits of having a digital health partner by your side with the CareClinic App. Its user-friendly interface makes it simple to record your peak flow readings, which is crucial for detecting early signs of asthma exacerbation. The app’s ability to generate insights and visual charts from peak flow meter helps both you and your healthcare provider adjust your treatment plan for optimal outcomes.
Don’t let asthma control your life; install the CareClinic App today and breathe easier knowing you have the tools to manage your health effectively.