
Almost 50% of women who give birth will experience headaches in the postpartum period. While most headaches go away within six weeks, for some women they can be a long-term problem. This article will explore the different types of headaches that can occur after giving birth, their causes, and how to get relief.
One type of headache that can occur after giving birth is called a postpartum migraine. This type of headache is characterized by a moderate to severe throbbing pain on one or both sides of the head, along with nausea and sensitivity to light and sound. Postpartum migraines are thought to be caused by hormone changes during pregnancy and the postpartum period.
Another type of headache that can occur after childbirth is tension-type headache. This type of headache feels like a tight band around the head or pressure behind the eyes and may be accompanied by fatigue, irritability, and difficulty concentrating. Tension headaches are thought to be caused by stress, fatigue, dehydration, or muscle tension.
Postpartum headaches can be managed with over-the-counter pain relievers such as ibuprofen or acetaminophen, as well as lifestyle changes such as regular exercise, maintaining a healthy diet, and getting enough sleep. If headaches persist for more than six weeks or become more severe, it is important to seek medical attention to rule out any underlying medical conditions.[1][2][3]
Table of Contents
- Introduction to Headaches – Types and Causes
- Possible Causes of Postpartum Headaches
- Does a C-Section Have an Impact on Postpartum Headaches?
- A note on pre-eclampsia
- Sleep Deprivation
- How Can Postpartum Headaches Be Treated?
- Tips for Managing Your Postpartum Migraine
- Blood Patch
- Are you breastfeeding?
- Monitoring Your Postpartum Headache Symptoms
- Monitoring your treatment
Introduction to Headaches – Types and Causes
A headache is a pain or an ache in the head. Headaches can be caused by different things such as stress, allergies, tension, lack of sleep, or sinus infections. There are different types of headaches. The most common type is a tension headache. Tension headaches are caused by muscle tightness and contractions in the head and neck area.
Other types of headaches include:
– Migraines: A migraine is a type of headache that is throbbing or pulsing. It is often accompanied by nausea, vomiting, and sensitivity to light and sound.
– Cluster headaches: Cluster headaches are a rare type of headache that occur in clusters. They are severe and cause pain on one side of the head.
– Sinus headaches: Sinus headaches are caused by inflammation in the sinuses. They often occur with a cold or fever.
– Headaches caused by changes in hormones: Changes in hormones can cause headaches. This includes during pregnancy and after giving birth (postpartum).
– A postdural puncture headache: is caused when a needle penetrates the spinal column from a lumbar puncture
– Stiff neck headaches are caused by muscle tension that builds up in the neck and scalp area. They can be relieved with rest, massage, or stretching exercises.[4][5][6][7]
Possible Causes of Postpartum Headaches
There can be many different causes for postpartum headaches. Some of the more common ones include hormone changes, water loss, and lack of sleep. But it’s also important to note that women with migraine, those who are older, or those who have had many births are more at risk for headaches.
Progesterone levels drop significantly after delivery, which can lead to headaches and fatigue. Dehydration from water loss during labor or breastfeeding can also cause headaches. Finally, the lack of sleep that comes with having a new baby can contribute to headaches as well.
If you have a family history of headaches or migraines, you may be more likely to experience postpartum headaches. It may help if you maintain a separate migraine diary to keep track of when they occur and to also discover any potential triggers.
The good news is that most headaches will go away on their own within the first six weeks postpartum. However, if they continue or become more severe, it’s important to seek medical attention. Headache symptoms can be tracked using the CareClinic app. This will help you keep track of your symptoms and provide information to your doctor.
Does a C-Section Have an Impact on Postpartum Headaches?
The short answer is yes. A Postpartum headache can occur anytime in the first 6 weeks after giving birth, and they can be either primary or secondary headaches. A primary headache is a headache that’s not associated with any other condition, while a secondary headache is a headache that’s caused by another condition, such as medication overuse, a head injury or infection.
One in four people get postpartum migraines within 2 weeks of giving birth, and they’re often more severe than other types of headaches. If you’re experiencing postpartum headaches, it’s important to track your symptoms using the CareClinic app. This will help you determine what type of headache you’re experiencing and provide information to your doctor about how best to treat them.
High blood pressure, pre-eclampsia, and other medical conditions associated with a C-section can also be factors in postpartum headaches because these conditions can interfere with the body’s ability to regulate hormones and also lead to fatigue, dehydration, and increased muscle tension. It is important for a woman who has had a C-section to pay close attention to her headaches and be sure to discuss them with her doctor as soon as possible.[8]
A note on pre-eclampsia
Pre-eclampsia is a serious and potentially life-threatening condition that can occur during pregnancy, typically after the 20th week, and is marked by high blood pressure and the appearance of protein in the urine. This condition can have severe implications for both mother and baby if not addressed immediately.
It can cause headaches, vision disturbances, and abdominal pain. It is important to seek medical attention as soon as possible if any of these symptoms occur. The condition occurs as a result of a defect in the placenta that prevents it from providing enough oxygen and nutrients to the baby.
Pre-eclampsia can lead to serious health problems for both mother and child if left untreated. If pre-eclampsia is diagnosed, it will be important for the woman to follow her doctor’s orders regarding medications and lifestyle changes in order to reduce the risk of postpartum headaches.[9][10]
Sleep Deprivation
Sleep deprivation can have a major impact on postpartum headaches. After giving birth, many women experience fatigue and exhaustion due to the lack of sleep. This lack of sleep arises from those long late-night feedings and the need to care for a newborn.
It is important to get as much sleep as possible during this time, even if it means taking naps throughout the day or having someone else take over diaper duty while you rest. Additionally, try to adjust your schedule so that you are sleeping when your baby sleeps – this will help prevent sleep deprivation and reduce the risk of postpartum headaches.
Finally, if you’re feeling overwhelmed, make sure to talk to someone about it. Whether it’s a friend or family member, a therapist or your doctor, talking to someone can help you get through this difficult time. Having support during this period is essential![11][12][13][14][15]
How Can Postpartum Headaches Be Treated?
If you’re experiencing a postpartum headache, there are a few things you can do to find relief.
- Try to stay hydrated by drinking lots of water and avoiding caffeine.
- Take a break and rest when you can.
- Apply a cold or warm compress to your forehead or neck.
- Try over-the-counter pain relievers like ibuprofen or acetaminophen.
If you’re still experiencing headaches after trying these home remedies, it’s important to see your healthcare provider to rule out any other causes.[16][17]
Tips for Managing Your Postpartum Migraine
If you’re struggling with migraines, here are a few things that might help:
- Get plenty of rest and sleep when you can. This can be tough to do when you have a newborn, but it’s important to try.
- Take breaks during the day to sit or lie down and relax. If possible, have someone else watch the baby so you can take a nap.
- Drink lots of fluids and eat healthy foods. This will help your body recover from the stress of childbirth and adjust to the hormonal changes.
- Avoid stress as much as possible. Try to find time for yourself, even if it’s just a few minutes each day.
- Ask your partner or family members for help with household tasks and childcare.
- If you’re breastfeeding, you can also try taking a daily supplement of vitamin B6, which has been shown to help reduce migraines. You should also talk to your doctor about other medications that might be safe to take while breastfeeding.
Blood Patch
In some cases, a blood patch may be recommended to treat postpartum migraines. This procedure involves injecting a small amount of your own blood into the area where the headache is concentrated. The injection helps seal up any leaks in your dura (the membrane that surrounds the brain and spinal cord) that could be causing headaches. Blood patches are generally considered safe and can effectively reduce the severity of postpartum migraines.[22][23]
Are you breastfeeding?
A note before you take medications for your headache: if you’re breastfeeding, be sure to talk to your doctor before taking any medications. Many pain relievers and migraine medications can pass through breast milk and may not be safe for your baby. The American Academy of Pediatrics recommends that you get a prescription medication specifically approved for use while breastfeeding. Over-the-counter medications may also be safe, but it’s best to check with your healthcare provider first.[24][25]
Monitoring Your Postpartum Headache Symptoms
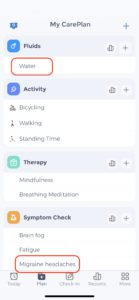
You can further track your symptoms with CareClinic to gain insight into the effectiveness of your care plan and make necessary modifications. This way, you can monitor trends in how you feel over time and how well your strategies are working to alleviate your symptoms. For example, if you find that certain foods seem to worsen your headaches, you can adjust your diet accordingly.
In addition to tracking your symptoms with CareClinic, you can also save any therapies, physical activities, and notes that may be helpful for managing postpartum headaches. For example, many people find relaxation techniques such as yoga, meditation, or deep breathing exercises to be beneficial in alleviating their headache symptoms. These activities can easily be scheduled into your CareClinic care plan.
One of the other benefits of using an app like CareClinic to manage postpartum headaches and migraines is its convenience. With CareClinic, new mothers can easily keep track of their symptoms and treatments from wherever they are. Another benefit is privacy. CareClinic keeps all of your personal data secure, so you can be sure that your confidential medical information is only accessible to you. Lastly, your data is backed up and encrypted, so you don’t have to worry about losing any of your information. If you would still like to use an offline method such as maintaining an offline printable headache diary, you can click here to print one.
Monitoring your treatment

Utilizing the CareClinic app, mothers can now monitor and record their postpartum headache or migraine symptoms. This information can help you and your healthcare team develops an effective treatment plan. Moreover, CareClinic ensures you’re receiving the best care possible by sending timely reminders for your medications and appointments. Postpartum headaches can be uncomfortable and even painful, yet with the help of family and friends, you’ll feel better soon! The right support makes all the difference in helping to heal faster. You can start by downloading the CareClinic app by tapping the button below, the app works on Android and iPhone!
Reference:
https://americanmigrainefoundation.org/resource-library/postpartum-headache/[26][27]
References
- “Postpartum Headaches: Causes, Diagnosis & Treatment”. https://my.clevelandclinic.org/health/diseases/postpartum-headache
- “Postpartum Headache”. https://elsevier-elibrary.com/contents/fullcontent/82175/epubcontent_v2/OEBPS/xhtml/chp0031.html
- “Postpartum Headache – StatPearls – NCBI Bookshelf”. https://www.ncbi.nlm.nih.gov/books/NBK537101/
- “Causes of headaches – Harvard Health”. https://www.health.harvard.edu/staying-healthy/causes-of-headaches
- “Types of Headaches | Mass General Brigham”. https://www.massgeneralbrigham.org/en/about/newsroom/articles/headache-types
- “Headaches: Types, Diagnosis & Treatment | Mercy”. https://www.mercy.net/service/headaches/
- “Headache: Types, Causes & Symptoms| Banner Brain & Spine”. https://www.bannerhealth.com/services/neurology/programs-care/headaches
- “Postpartum migraines: a long-term prospective study – PubMed”. https://pubmed.ncbi.nlm.nih.gov/23154716/
- “Pre-eclampsia”. https://www.who.int/news-room/fact-sheets/detail/pre-eclampsia
- “Preeclampsia – Symptoms and causes – Mayo Clinic”. https://www.akamai.mayoclinic.org/diseases-conditions/preeclampsia/symptoms-causes/syc-20355745
- “The Impact of Sleep Deprivation on New Mothers: 12 Effective Coping Strategies for Better Rest – Roswell, Alpharetta, Milton | Omega Pediatrics”. https://www.omegapediatrics.com/sleep-deprivation-newmoms-copingstrategies/
- “How to Reduce Sleep Deprivation with a Newborn Baby – Childbirth Concierge®”. https://childbirthconcierge.com/how-to-reduce-sleep-deprivation-with-a-newborn-baby/
- “The Exhausted Mom’s Guide to Postpartum Sleep Deprivation”. https://www.joinphoenixhealth.com/resourcecenter/postpartum-sleep-deprivation-and-depression/
- “Coping with Sleep Deprivation Impacting Mental Health”. https://joinphoenixhealth.com/resourcecenter/coping-with-sleep-deprivation-and-its-impact-on-mental-health/
- “Sleep Deprivation and Postpartum Depression”. https://www.sleepfoundation.org/pregnancy/sleep-deprivation-and-postpartum-depression
- “Postpartum Headaches: Causes, Treatment, and Prevention”. https://www.parents.com/postpartum-headache-causes-treatment-and-prevention-8627725
- “Headaches in pregnancy (natural remedies) | BabyCenter”. https://www.babycenter.in/pregnancy/pregnancy-health/headaches-in-pregnancy-natural-remedies_549297
- “Postpartum Migraine: Causes, Duration, Treatment, and More”. https://www.bezzymigraine.com/discover/living-well-mig/health-tips-for-managing-migraine-after-giving-birth/
- “Managing Migraine During Pregnancy and Lactation – Clinical Pain Advisor”. https://www.clinicalpainadvisor.com/features/managing-migraine-during-pregnancy-and-lactation/
- “How to Deal with Migraine in the Postpartum Period”. https://www.neurahealth.co/blog/migraine-in-the-postpartum-period
- “Headache: pregnancy and breastfeeding. Recommendations of the Spanish Society of Neurology’s Headache Study Group | Neurología (English Edition)”. https://www.elsevier.es/es-revista-neurologia-english-edition–495-articulo-headache-pregnancy-breastfeeding-recommendations-spanish-S2173580821001383
- “Journal of Obstetric Anaesthesia and Critical Care”. https://journals.lww.com/joac/fulltext/2011/01020/headache_in_the_parturient__pathophysiology_and.2.aspx
- “Epidural Blood Patch – StatPearls – NCBI Bookshelf”. https://www.ncbi.nlm.nih.gov/books/NBK482336/
- “Medication Safety Tips for Breastfeeding Parents – HealthyChildren.org”. https://www.healthychildren.org/English/ages-stages/baby/breastfeeding/Pages/Medications-and-Breastfeeding.aspx
- “Migraines and Breastfeeding – The Breastfeeding Network”. https://www.breastfeedingnetwork.org.uk/factsheet/migraines/
- “Managing Postpartum Headaches: Causes, Symptoms, and Treatment – DoveMed”. https://www.dovemed.com/health-topics/focused-health-topics/managing-postpartum-headaches-causes-symptoms-and-treatment
- “Postpartum Headaches: Causes, Symptoms, and Treatment”. https://www.centeronemedical.com/post/postpartum-headaches-causes-symptoms-and-treatment


