Approximately 10% of reproductive-age women are diagnosed with endometriosis, a painful condition in which endometrial-like tissue grows in different locations of the body. This condition can lead to debilitating abdominal pain and can severely disrupt daily activities. For this reason, many non-hormonal and hormonal treatments currently exist to help alleviate the severe pain associated with endometriosis and prevent further complications from occurring. However, many other endometriosis digestive symptoms go unrecognized or treated, such as nausea. Nausea is an underrecognized endometriosis symptom but can cause just as significant disruptions to day-to-day activities. Fortunately, research has shown a variety of different causes of endometriosis-associated nausea and how you can treat nausea to help you feel better than ever! The CareClinic app allows you to do this through an easy-to-use, comprehensive interface. By using the app, you can determine trends in your nausea endometriosis symptom and treat it much more effectively![1][2][3][4]
Overview of Endometriosis
Every month, your uterine cavity buildings an inner lining called the endometrial tissue, or the endometrium1. The purpose of the endometrial tissue is to help support the early phases of fetal development in case you get pregnant. However, when fertilization does not occur, these layers of the uterine lining are simply not necessary. This is where your menstrual periods occur and lining sheds away from the uterine walls to be expelled in the form of menstrual blood.
In endometriosis, a lining very similar to the endometrium grows on other organs of body structures such as your abdomen, pelvis, or sometimes, even your chest. What’s important to note here is that like the endometrium, this endometriosis tissue (endometrial-like tissue) grows and is sensitive to your hormone levels. As these levels fluctuate and change through your menstrual cycle, this tissue can become inflamed and can cause ovarian cysts, superficial endometriosis lesions and adhesions, deeper nodules, and scar tissue formation1.
Where can Endometriosis Occur?
Endometriosis patients can experience endometrial-like tissue growth in many different areas of the body1. These pelvic organs and body parts include:
- On the outer wall of the uterus
- Fallopian tubes/Ovaries
- Vagina
- Peritoneum
- Bladder and ureters
- Intestines
- Rectum
- Diaphragm
Note that generally, the most common places where endometriosis occurs are naturally proximal to the uterus, where the endometrium typically grows1.
Causes of Endometriosis
Like many other conditions, endometriosis follows the trend of no known direct cause. However, there are many risk factors that can predict the likelihood of developing endometriosis, including family history, early onset of painful periods, a shorter menstrual cycle length and flow duration, as well as defects in the uterus and fallopian tubes1. It has also been found to most commonly occur in people of reproductive age – 25 to 40 – with a lower prevalence in the teenage years.

Moreover, the connection between a family history of endometriosis and the increased development risk has led experts to believe there may be a genetic component involved. It is important to note, however, that no direct genetic cause has been identified yet.
The takeaway: there is no direct known cause of endometriosis1. Instead, there are risk factors that can help you assess if you have a higher probability of development. One way to keep track of these risk factors is by using a healthcare app, such as CareClinic. CareClinic offers a variety of tools that allow you to record pertinent information that you can then send and show to your doctor to help assess your risk of endometriosis. This can be completed by using the Care Team feature within the CareClinic app. By adding your healthcare provider, they will automatically be informed about your recorded data, including your menstruation characteristics, to help quickly and efficiently assess your endometriosis risk over time.
Endometriosis Symptoms
The biggest symptom associated with endometriosis is abdominal pain1,2. Intense pain is a relatively ambiguous term, and it can be described as intense, mild, and across a variety of different locations. Pain can also be the result of something that is occurring, for example, rectal pain may result from rectal bleeding In the case of endometriosis, pain is generally experienced around the abdominal area and can sometimes extend into the pelvis and lower back. This severe abdominal pain can also tend to get worse in different scenarios, such as during menstruation or painful sex1.
Now, what’s important to remember, is that not everyone experiences the same endometriosis symptoms1. While some might experience debilitating abdominal pain, others may not even be aware they have the condition until another procedure is carried out. Like many of the other conditions we have discussed, endometriosis doesn’t look the same for everyone and this is an important aspect you should consider when assessing if you suspect the condition.
Some other gynecological symptoms and severe symptoms endometriosis patients have reported include2:
- Non-menstrual pelvic pain
- Difficult and painful urination
- Painful bowel movements
- Heavy menstruation, excessive bleeding and painful periods
- Spotting in between menstrual periods
- Infertility
Diagnosis and Treating Endometriosis
Upon a physical exam, it might not be easy to spot endometriosis straight off the bat. As we’ve already discussed, endometrial-like tissue can grow in a variety of places and may not be visible without additional testing. Therefore, the preliminary diagnosis of endometriosis is actually more heavily based on clinical history3. Tenderness in your abdomen and pelvic pain may lead your physician to suspect endometriosis – but these symptoms can be common to a variety of other conditions! Thus, you’ll often find yourself swept up into additional diagnostic tests, including urine testing, a pap test, and vaginal and endocervical swabs. These tests serve to help rule out another possible diagnosis before carrying out the gold standard for endometriosis: the laparoscopy3.
During a laparoscopy, your doctor will likely use a small camera called a laparoscope, to visualize what’s going on inside your body3. During this procedure, a small tissue sample might be taken and sent to the lab for confirmation of the diagnosis. However, this procedure is more invasive and is often considered only after other possible diagnoses have been ruled out3.
When it comes time to treat endometriosis, your healthcare provider will likely assess several factors. These include the severity of your endometriosis, your fertility plans, your age, and symptom severity1,3. To manage symptoms of endometriosis, there are generally 2 routes: surgery or pain medications.
Medications for Endometriosis
There are 2 broad types of drugs used to treat endometriosis: non-steroidal anti-inflammatory drugs (NSAIDs) and low-dose combined oral contraceptive pills (COCPs)3. Generally, NSAIDs are used first and their effectiveness is assessed at the end of 3 months. Following this first-line treatment, second-line hormonal therapy includes the COCPs, gonadotropin-releasing hormone (GnRH) agonists and hormone-based medications which can help reduce endometriosis pain. In some cases, like with gonadotropin-releasing hormone (GnRH) agonists, they can even stop the hormones that cause the conditions from being produced1,3.
Surgical Intervention
In the more severe cases of endometriosis, surgery is often used in treating endometriosis. Surgery can come in many different procedures, each with a different target end result3. One of the most common procedures includes, once again, laparoscopy1. This type of laparoscopy, however, employs small 5 mm instruments. These are used, with the help of the camera, to remove endometriosis lesions. Alternatively, laser-based instruments might be used for the same purpose1,3.
Only when necessary, your doctor might recommend a hysterectomy. This is where the uterus and additional areas of endometriosis are completely removed3. Needless to say, this procedure needs to be considered in the context of many other factors, including the patient’s future plans regarding fertility and the presence of other uterine conditions1.[5]
What Happens if Endometriosis is left Untreated? Is it Dangerous?
Endometriosis can cause significant symptoms and discomfort – so what happens if you discover the condition later in its progression or if you choose not to go on treatment to manage symptoms? The answer boils down to the severity of the condition and the duration of time for which it is left untreated4.
The majority of the time, leaving endometriosis untreated can reduce fertility and inflict damage to surrounding pelvic organs, such as the ovaries and reproductive organs4. This damage can present in the form of inflammation and gastrointestinal symptoms (GI symptoms)as well. Chronic inflammation can subsequently increase your risk for cardiovascular disease as well4. Additionally, many studies have found that untreated endometriosis can increase the risk of complications during childbirth5. Endometriosis patients have been found to be at higher risk for pregnancy loss, early labour, placenta previa, and emergency c-sections.
However, in some cases, the condition might just resolve itself. Endometriosis lesions may get smaller and become scarcer and symptoms may disappear1. This is most often observed after menopause when the hormones responsible for the condition are produced to a lesser degree.
So, is leaving endometriosis untreated dangerous? The short answer: it can be but in different ways than what you might expect. The main result is pain, and this pain can cause serious effects on the quality of life of someone with endometriosis. In fact, many studies have found that this type of chronic pain can significantly harm a person’s mental health and is correlated to higher rates of depression and anxiety6. It’s important to take these non-physical characteristics into consideration when deciding your course of action.[6][7][8]
Can Endometriosis cause Nausea?
There are many symptoms of endometriosis that are not talked about as often. Despite their lack of mention in the more common or characteristic symptoms of the condition, these symptoms can be just as serious and can leave you feeling significantly unwell. One of the major symptoms reported by patients with endometriosis is nausea. So, what is nausea and how does it relate to the condition?
Defining Nausea
Nausea is simply defined as the urge to vomit7. That unsettled, uneasy feeling in your stomach leaves you feeling sick. Oftentimes, nausea is a sign of another condition, including the stomach flu, food poisoning, appendicitis, and motion sickness7. For today’s purposes, nausea is a sign of endometriosis that should be considered by your physician.
Oftentimes, nausea is mistaken for vomiting and the 2 terms are considered synonymous7. This isn’t technically true. Essentially, vomiting is generally preceded by nausea, but nausea doesn’t always lead to vomiting7. Think of the relationship between the 2 like toasting a piece of bread. Toasting will always occur but will only sometimes lead to burnt toast, however, burnt toast is always preceded by toasting the bread.
The Gastrointestinal Symptoms of Endometriosis
As you might have guessed, nausea is implicated in the gastrointestinal system. Symptoms of the gastrointestinal system, like nausea, are often overlooked and not spoken about in endometriosis patients. However, these symptoms have been found to be much more serious in patients as compared to others in a 2015 study8. In fact, in patients with bowel endometriosis – endometriosis tissue growth in areas affecting the bowel and bowel movements – increased nausea and vomiting were observed. Additionally, it was found that there is an existing relationship between patients with endometriosis, also having irritable bowel syndrome (IBS). Moreover, the currently used treatment continued to aggravate the gastrointestinal symptoms (GI symptoms) associated with irritable bowel syndrome8. Thus, it is important to consider the type of treatment you would like to take if you experience nausea as a symptom of endometriosis.
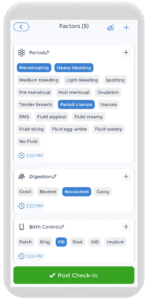
The Common Causes of Endometriosis Associated Nausea
Nausea that comes with irritable bowel syndrome and bowel endometriosis may be aggravated or caused by a variety of different situations. Two of the more common ones include menstruation and eating a meal. Distinguishing the correlation between these possible causes and your nausea can sometimes be difficult. Fortunately, the CareClinic app encompasses many features that help make this easier for you! For example, recording your nausea symptom in the symptom tracker and your periods with the period tracker can help you come up with correlation charts to see the relationship between the two. This gives you a good visual and can help you identify what you need to change to feel better, sooner!
Nausea during your Period
Many people who do experience nausea with endometriosis report that the symptom appears to get worse during a specific point in their menstrual cycle: the period9. The reason for this boils down to the fact that an endometrial lesion is composed of tissue similar to that of the endometrium, or endometrial tissue. Therefore, they behave in the same way9.
During your menstrual periods, your uterine lining bleeds and leaves the body as menstrual blood9. Similarly, the lesions swell and bleed as well, but have no way out. This causes significant pain and discomfort. This doubled with lesion location close to the GI tract, has been found to contribute to the experience of gastrointestinal symptoms like nausea during your period9.
Additionally, during your menstrual periods, a hormone-like molecule called prostaglandins causes your uterus to contract in order to help get rid of the lining9. These contractions are what many call period or menstrual cramps. In people with endometriosis, this intestinal cramping is generally quite severe and the discomfort has contributed to the feeling of nausea. Additionally, prostaglandin entrance into the bloodstream can also play a hand in nausea9.
Nausea after Eating
Some people have also reported endometriosis-associated gastrointestinal symptoms (GI symptoms) like nausea to get worse following a meal9. Again, this comes down to the gastrointestinal aspects of endometriosis. After eating, sometimes we feel bloated, and this abdominal bloating can actually get worse if you have endometriosis. Bloating occurs because your body is working to digest food. Unfortunately, bloating is also uncomfortable and can cause some pain that leads to nausea. Additionally, bowel lesions of endometriosis can cause obstructions in the GI tract and once again, lead to symptoms like nausea. However, this is quite rare, only affecting about 5 to 12% of endometriosis patients9.[11]
Preventing Endometriosis Associated Nausea
Taking Medication
Your physician might recommend taking certain medications to help reduce your gastrointestinal endometriosis symptoms9. While some of these medications can aggravate symptoms of nausea, some can help ease them instead. Taking these medications may help manage your nausea9.
Adjusting your Diet and Eating Habits
Adding more fruits, vegetables, omega-3-rich foods and whole grains to your diet has been shown to help reduce endometriosis symptoms, including nausea9. You might also decide to cut back on some of the more harmful foods. These can include high-FODMAP foods, saturated and trans fats, red meat, gluten, dairy, caffeine, and alcohol9.
Additionally, developing healthy eating habits can also help prevent feelings of nausea9. For example, try to consume smaller but more frequent meals, and slow down your eating. Try to avoid eating too many warm or hot, strong-smelling, spicy and greasy foods, as these can make your nausea worse9!
Change your Posture & Clothing
Finally, when you are bloated, the last thing your want to do is to place and strain or pressure on your stomach9. This can further enhance nausea. Thus, try to avoid lying down, bending over, or performing activities that put a strain on your abdomen direct after eating9.
Stay away from tight-fitting clothes as well, as those super snug jeans may just push into your abdomen and make you feel worse9. Instead, opt for looser-fitting clothing that allows your stomach to breath9.[12]
Nausea Home Remedies for Endometriosis Nausea
Like for other causes of nausea you might experience, there are many ways to alleviate the symptom and get you feeling better. Some of these home remedies and tips include:
- Anti-Nausea Medications: There are many over-the-counter nausea medications available. Some examples include Pepto-Bismol and Gravol9.
- Eating Bland Foods: while you’re feeling nausea, it is often best to stick to and eat bland foods. These foods include things like white rice, bananas, and unseasoned skinless chicken9.
- Try Ginger and Peppermint: Research has suggested that ginger can be effective at helping mild endometriosis nausea and painful menstrual cramps. Additionally, peppermint can help with nausea during pregnancy and after surgery. Try sipping on some ginger or peppermint tea or trying peppermint aromatherapy to help alleviate your symptoms9.
- Drink Enough Water: Nausea sometimes results in vomiting. Vomiting can lead you to be dehydrated. It is important for you to stay hydrated when you feel nauseous. Try taking small and regular sips of water to help keep your fluids down9.
- Distractions are Key: Take your mind off your nausea! Try reading a book, watching your favorite show or listening to some music to help distract yourself from your nausea9.
- Get Outside: Sometimes all you need is some fresh air to help ease your nausea. Open a window or take a walk until you feel better9.
How CareClinic can help
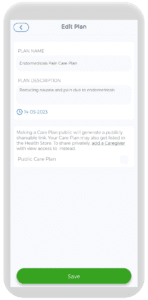
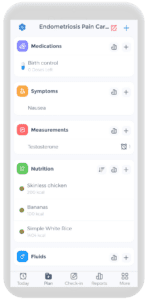
Luckily, the CareClinic app allows you to track these different aspects all in one place. Once you’ve established a non-hormonal or hormonal treatment plan, you can also use the app to determine if it’s working well for you. For example, if you decide to start medication for endometriosis, such as oral birth control, you can track your dosage in the medication tracker and your nausea and other endometriosis-related symptoms in the symptoms tracker to determine if the medication is helping. Additionally, use the Care Plan feature to design a quick check-in page that encompasses all the different parts of your endometriosis management. This can include specific symptoms you experience, your medication and dosage, period tracking and more!
Creating this custom Care Plan can help you keep track of everything related to your condition in one place. It becomes easier to manage your condition and make changes as necessary to help you feel better, faster than ever!
References
- Cleveland Clinic. (2022, July 27). Health Library. Retrieved from: https://my.clevelandclinic.org/health/diseases/10857-endometriosis
- Agarwal, S. K., Chapron, C., Giudice, L. C., Laufer, M. R., Leyland, N., Missmer, S. A., Singh, S. S., & Taylor, H. S. (2019). Clinical diagnosis of endometriosis: a call to action. American Journal of Obstetrics and Gynecology, 220(4), 354.e1–354.e12. https://doi.org/10.1016/j.ajog.2018.12.039
- Parasar, P., Ozcan, P., & Terry, K. L. (2017). Endometriosis: Epidemiology, Diagnosis and Clinical Management. Current Obstetrics and Gynecology Reports, 6(1), 34–41. https://doi.org/10.1007/s13669-017-0187-1
- Villines, Z. (2022, October 31). What are the risks of untreated endometriosis?. Medical News Today. Retrieved from: https://www.medicalnewstoday.com/articles/what-happens-if-endometriosis-is-left-untreated
- Zullo, F., Spagnolo, E., Saccone, G., Acunzo, M., Xodo, S., Ceccaroni, M., & Berghella, V. (2017). Endometriosis and obstetrics complications: a systematic review and meta-analysis. Fertility and Sterility, 108(4), 667-672.e5. https://doi.org/10.1016/j.fertnstert.2017.07.019
- Armour, M., Sinclair, J., Ng, C. H. M., Hyman, M. S., Lawson, K., Smith, C. A., & Abbott, J. (2020). Endometriosis and chronic pelvic pain have a similar impact on women, but time to diagnosis is decreasing: an Australian survey. Scientific Reports, 10(1). https://doi.org/10.1038/s41598-020-73389-2
- Cleveland Clinic. (2019, July 23). Nausea & Vomiting. Health Library. Retrieved from: https://my.clevelandclinic.org/health/symptoms/8106-nausea–vomiting
- Ek, M., Roth, B., Ekström, P., Valentin, L., Bengtsson, M., & Ohlsson, B. (2015). Gastrointestinal symptoms among endometriosis patients—A case-cohort study. BMC Women’s Health, 15(1). https://doi.org/10.1186/s12905-015-0213-2
- Seladi-Schulman, J. (2022, March 22). Can endometriosis cause nausea?. Retrieved from: https://www.healthline.com/health/endometriosis/endometriosis-nausea
References
- “Endometriosis”. https://www.who.int/news-room/fact-sheets/detail/endometriosis%E2%81%A0
- “Nausea in Endometriosis: where does it come from? – The Endometriosis Nutritionist”. https://theendometriosisnutritionist.online/articles/nausea-in-endometriosis/
- “Endometriosis Symptoms and Signs | Article | GLOWM”. https://www.glowm.com/article/heading/vol-3–endometriosis–endometriosis-symptoms-and-signs/id/417643
- “Nausea and Endometriosis: Causes and Treatment | MyEndometriosisTeam”. https://www.myendometriosisteam.com/resources/nausea-and-endometriosis
- “Endometriosis – Symptoms and causes – Mayo Clinic”. https://www.akamai.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656
- “Endometriosis and risk of cardiovascular disease: a systematic review and meta-analysis – PubMed”. https://pubmed.ncbi.nlm.nih.gov/39833762/
- “Adverse pregnancy outcomes for women with endometriosis: a systematic review and meta-analysis”. https://pubmed.ncbi.nlm.nih.gov/34541648/
- “Endometriosis: A Comprehensive Exploration of Inflammatory Mechanisms and Fertility Implications – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC11370979/
- “Relevance of gastrointestinal symptoms in endometriosis”. https://pubmed.ncbi.nlm.nih.gov/19694698/
- “Endometriosis and irritable bowel syndrome: a systematic review and meta-analysis – PubMed”. https://pubmed.ncbi.nlm.nih.gov/32949284/
- “Endometriosis and Prostaglandins – Seckin Endometriosis Center”. https://drseckin.com/endometriosis-and-prostaglandins/
- “Endometriosis Diet: What to Eat and What to Avoid”. https://flo.health/menstrual-cycle/lifestyle/diet-and-nutrition/endometriosis-diet
- “Effect of aromatherapy with peppermint, ginger, and lavender on postoperative nausea severity after oral surgery under general anaesthesia: A single-blind randomized controlled trial – PubMed”. https://pubmed.ncbi.nlm.nih.gov/40154579/