Atopic Dermatitis (AD) is a chronic skin condition that affects millions of people worldwide. If you or someone you care about struggles with this condition, you know firsthand what a frustrating, painful and, at times, debilitating experience it can be. The good news is that the right management and treatment plan can help to improve symptoms, reduce flare-ups, and promote better overall health and wellness. This guide will provide you with a comprehensive overview of Atopic Dermatitis and its management, including diagnosis, treatment options, and prevention strategies.[1][2][3]
What is Atopic Dermatitis?
Definition and Overview
Atopic Dermatitis, also known as eczema, is a type of chronic inflammatory skin disease characterized by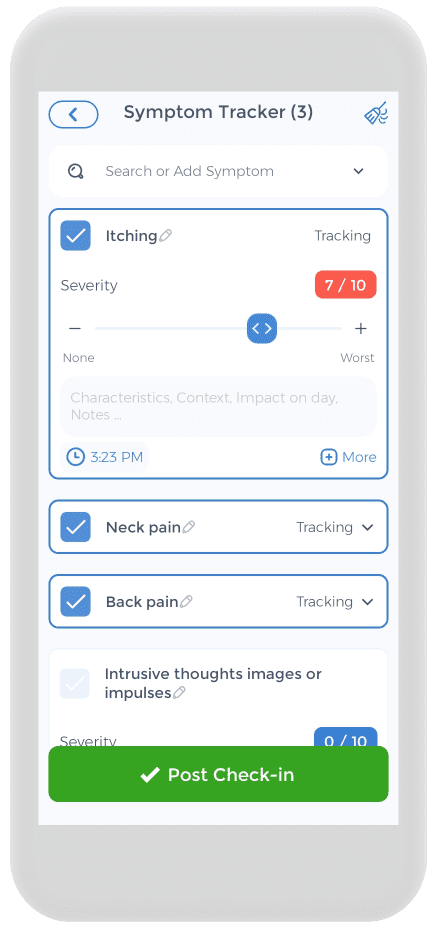 red, itchy, scaly, and inflamed skin. It can occur in adult and pediatric patients, but is most common pediatric patients. It is estimated that up to 20% of children and 3% of adults worldwide suffer from Atopic Dermatitis. AD is a complex condition, with multiple environmental and genetic factors contributing to its development.
red, itchy, scaly, and inflamed skin. It can occur in adult and pediatric patients, but is most common pediatric patients. It is estimated that up to 20% of children and 3% of adults worldwide suffer from Atopic Dermatitis. AD is a complex condition, with multiple environmental and genetic factors contributing to its development.
Atopic Dermatitis is a long-term condition that can cause significant discomfort and disability. It can affect various parts of the body, including the face, neck, hands, and feet. The condition can be challenging to manage, and it often requires a combination of medication, lifestyle changes, and self-care strategies.
Causes and Risk Factors
The exact cause of Atopic Dermatitis is unknown, but research suggests a complex interplay between genetic, environmental, and immunological factors. Genetics seems to play a significant role in its development, as it often runs in families. People with a personal or family history of allergies, hay fever, and asthma are more likely to develop Atopic Dermatitis. Additionally, exposure to irritants, allergens, and stress can also trigger or worsen symptoms.
Environmental factors such as pollution, climate, and humidity can also affect the severity of Atopic Dermatitis symptoms. For example, people living in urban areas with higher levels of air pollution may experience more severe symptoms than those living in rural areas. Similarly, people living in hot and humid climates may experience more sweating and itching, which can worsen the condition.
Common Symptoms and Signs
The symptoms of AD patients can vary significantly from person to person, and even from one episode to the next. They often occur in acute flares. Some of the most common symptoms include:
- Red or inflamed skin
- Dry and scaly skin
- Itching and scratching
- Blisters and oozing
- Thickened and leathery skin
These symptoms can lead to significant discomfort, pain, and disability, and can also affect the person’s self-esteem, mood, and sleep quality. It is essential to seek medical attention if you experience any of these symptoms to ensure an accurate diagnosis and effective treatment plan.
In addition to the physical symptoms, moderate to severe AD can also have a significant impact on a person’s mental health. Living with a chronic skin condition can be challenging, and it can lead to feelings of anxiety, depression, and social isolation. It is essential to seek support from family, friends, and healthcare professionals to manage both the physical and emotional aspects of the condition.
Managing and Treating Atopic Dermatitis
There is currently no cure for Atopic Dermatitis, but there are several treatment options available to manage symptoms and improve quality of life. Treatment typically involves a combination of medication, lifestyle changes, and self-care strategies.
Medications such as topical corticosteroids, calcineurin inhibitors, and antihistamines can help reduce inflammation, itching, and other symptoms. In severe cases, oral medications and light therapy may be necessary.
Lifestyle changes such as avoiding triggers, using gentle skincare products, and wearing loose-fitting clothing can also help manage symptoms. Self-care strategies such as moisturizing regularly, taking warm (not hot) baths, and avoiding scratching can also help prevent flare-ups.
It is essential to work closely with a healthcare professional to develop an effective treatment plan that addresses your specific symptoms and needs. With proper management, most people with Atopic Dermatitis can lead healthy, active lives.[4][5]
Diagnosing Atopic Dermatitis
Atopic Dermatitis, also known as eczema, is a chronic skin condition that affects millions of people worldwide. It is characterized by dry, itchy, and inflamed skin that can be red, scaly, and even blistered. While the exact cause of Atopic Dermatitis is unknown, it is believed to be related to a combination of genetic and environmental factors.
Medical History and Physical Examination
If you suspect you may have Atopic Dermatitis, it is important to seek medical attention from a dermatologist. Your doctor will likely begin with a comprehensive medical history and physical examination. They will ask about your symptoms, their frequency and duration, and any triggers you have noticed. They may also examine your skin closely to look for signs of Atopic Dermatitis, such as dryness, redness, and scaling.
During the examination, your doctor may also ask about your family history of skin conditions, as Atopic Dermatitis tends to run in families. They may also inquire about any other medical conditions you have or medications you are taking that may be contributing to your symptoms.
Diagnostic Tests and Procedures
In some cases, your doctor may recommend additional diagnostic tests or procedures to help diagnose or monitor your condition. These may include blood tests (to check for allergies or infections), allergy patch testing (to identify skin allergens), a skin prick test, or a cortisol stimulation test.
In a skin prick test, a small amount of a suspected allergen is placed on the skin, and the skin is then pricked with a needle. If you are allergic to the substance, a small red bump will appear on the skin within 15-20 minutes to indicate allergic sensitization.
Another diagnostic test that may be performed is a skin biopsy. In a skin biopsy, a small sample of skin is removed and examined under a microscope to look for signs of Atopic Dermatitis or other skin conditions.
Differential Diagnosis
It is important to differentiate Atopic Dermatitis from other skin conditions that share similar symptoms, such as allergic contact dermatitis, psoriasis, allergic rhinitis, fungal cutaneous infections or other skin infections. An accurate diagnosis is crucial for developing an effective treatment plan.
Allergic or irritant contact dermatitis is a type of eczema that is caused by contact with an irritant or allergen causing allergic reactions, while psoriasis is a chronic autoimmune condition that causes skin cells to build up rapidly, resulting in thick, scaly patches of skin. Fungal infections, such as ringworm, can also cause similar symptoms.
If you are diagnosed with Atopic Dermatitis, your doctor will work with you to develop a treatment plan that may include topical creams or ointments, oral medications, and lifestyle changes to help manage your symptoms and prevent flare-ups.[6][7][8][9]
Treatment Options for Atopic Dermatitis
Atopic Dermatitis, also known as eczema, is a chronic inflammatory skin condition that affects millions of people worldwide. It is characterized by red, itchy, and scaly patches of skin that can be both uncomfortable and unsightly. While there is no cure for Atopic Dermatitis, there are several treatment options available that can help to manage symptoms and improve quality of life.
Topical Treatments

Topical steroid creams or ointments are the most commonly prescribed topical treatments for Atopic Dermatitis. These medications work by reducing inflammation and suppressing the immune system. They can be very effective in managing symptoms, but long-term use can lead to thinning of the skin and other side effects. Calcineurin inhibitors, such as tacrolimus and pimecrolimus, are another type of topical medication that can be used to treat Atopic Dermatitis. These medications work by suppressing the immune system and reducing inflammation, without the side effects associated with higher-potency topical steroids.
Topical immunomodulators, such as crisaborole, are a newer class of medication that work by targeting specific immune cells involved in the development of Atopic Dermatitis. These medications can be effective in managing symptoms and may be a good option for people who cannot tolerate or do not respond to other topical treatments.
Wet wrap therapy involves applying a moisturizer or medication to the skin, followed by wrapping the affected area in wet bandages or clothing. This can help to enhance the effectiveness of topical treatments and reduce itching and inflammation. Phototherapy, also known as light therapy, involves exposing the skin to specific wavelengths of light to reduce inflammation and itching. It is typically used in moderate to severe cases and can be used alone or in combination with other treatments.
Systemic Treatments
If your symptoms are severe or do not respond to topical treatments, your doctor may recommend a systemic treatment. These can include oral corticosteroids, immunosuppressive agents, or biologics. These treatments can be effective in controlling symptoms, but evidence suggests they also carry higher risks of side effects and require close monitoring.
Oral corticosteroids, such as prednisone, can be used to quickly reduce inflammation and itching in severe cases of Atopic Dermatitis. However, they can also cause significant side effects, such as weight gain, high blood pressure, and increased risk of infection, and should only be used for short periods of time.
Immunosuppressive agents, such as cyclosporine and methotrexate, work by suppressing the immune system and reducing inflammation. These medications can be effective in managing symptoms, but they also carry a higher risk of side effects and require close monitoring.
Biologics, such as dupilumab, are a newer class of medication that work by targeting specific proteins in the immune system that are involved in the development of Atopic Dermatitis. These medications can be highly effective in managing symptoms and may be a good option for people who do not respond to other treatments. However, they are also very expensive and may not be covered by insurance.
Alternative and Complementary Therapies
Many people use alternative or complementary therapies to manage their Atopic Dermatitis symptoms, such as probiotics, herbal remedies, or acupuncture. While these therapies may have some benefits, it is crucial to discuss them with your doctor first, as some can have harmful interactions with prescription medications or may exacerbate symptoms.
Probiotics, which are live bacteria and yeasts that are beneficial for gut health, may also have some benefits for people with Atopic Dermatitis. Some studies have shown that probiotics can help to reduce inflammation and improve skin barrier function, but more research is needed to confirm these findings.
Herbal remedies, such as chamomile and calendula, have been used for centuries to treat various skin conditions, including Atopic Dermatitis. While these remedies may have some anti-inflammatory and soothing properties, there is limited scientific evidence to support their use.
Acupuncture, a traditional Chinese medicine practice that involves inserting thin needles into specific points on the body, may also be helpful for managing Atopic Dermatitis symptoms. Some studies have shown that acupuncture can help to reduce itching and improve sleep quality, but more research is needed to confirm these findings.
In conclusion, Atopic Dermatitis is a chronic inflammatory skin condition that can be both uncomfortable and unsightly. While there is no cure for Atopic Dermatitis, there are several treatment options available that can help to manage symptoms and improve quality of life. It is important to work closely with your doctor to determine the best treatment plan for your individual needs and to discuss any alternative or complementary therapies you may be considering.[10][11]
Managing Atopic Dermatitis Flare-Ups
Atopic Dermatitis, also known as eczema, is a chronic skin condition that affects millions of people worldwide. It is characterized by dry, itchy, and inflamed skin that can be painful and uncomfortable. While there is no cure for Atopic Dermatitis, there are several ways to manage and reduce symptoms.
Identifying and Avoiding Triggers
One of the most effective ways to manage Atopic Dermatitis is to identify and avoid triggers that can worsen symptoms. Common triggers may include stress, exposure to allergens and irritants, hot or cold temperatures, and certain foods or medications. Keeping a symptom diary can help you identify your triggers and take steps to avoid them.
For example, if you notice that your symptoms worsen after eating certain foods, such as dairy or gluten, you may want to consider eliminating them from your diet. Similarly, if you notice that your symptoms are worse during the winter months, you may want to take extra precautions to protect your skin from the cold and dry air.
Developing a Skincare Routine
Developing a skincare routine is crucial for managing Atopic Dermatitis symptoms. This may involve using gentle, fragrance-free products, moisturizing regularly, and avoiding harsh soaps and hot showers. Your doctor may also recommend specific skincare products or regimens to manage your symptoms.
It is important to keep your skin moisturized, as dry skin can worsen Atopic Dermatitis symptoms. Using a thick, emollient moisturizer can help to soothe and protect your skin. You may also want to consider using a humidifier in your home to add moisture to the air.
Managing Stress and Anxiety
Stress and anxiety can exacerbate Atopic Dermatitis symptoms. Practicing relaxation techniques, such as meditation or deep breathing, and seeking support through therapy or support groups can help to reduce stress and improve overall well-being.
It is important to take care of your mental health as well as your physical health when managing Atopic Dermatitis. Stress can trigger flare-ups, so finding ways to manage stress can be an important part of your treatment plan.
By identifying and avoiding triggers, developing a skincare routine, and managing stress and anxiety, you can effectively manage Atopic Dermatitis symptoms and improve your quality of life.
Living with Atopic Dermatitis
Atopic Dermatitis, also known as eczema, is a chronic skin condition that affects millions of people worldwide. It is characterized by dry, itchy, and inflamed skin that can be painful and uncomfortable. While there is no cure for Atopic Dermatitis, there are many ways to manage the condition and improve quality of life.
Coping with the Emotional Impact
Living with Atopic Dermatitis can be emotionally challenging. The constant itching and discomfort can affect self-esteem, body image, and social relationships. It is not uncommon for people with the condition to feel embarrassed or self-conscious about their skin.
One way to cope with the emotional impact of Atopic Dermatitis is to seek support from loved ones. Talking to friends and family members about your feelings can help you feel less alone and more understood. Additionally, participating in therapy or support groups can provide a safe space to discuss your struggles and learn coping strategies.
Practicing self-care is also essential for improving emotional well-being. This can include activities such as meditation, yoga, or spending time in nature. Taking care of your mental health is just as important as taking care of your physical health.
Tips for Parents and Caregivers
Caring for a child with pediatric Atopic Dermatitis can be challenging. The constant itching and discomfort can be distressing for both the child and their caregivers. However, there are many things parents and caregivers can do to support their child and improve their quality of life.
Creating a safe and supportive environment is crucial for children with childhood Atopic Dermatitis. This can include using gentle, fragrance-free products, avoiding harsh chemicals, and keeping the skin moisturized. Educating yourself and others about the condition can also help to reduce stigma and increase understanding.
Seeking appropriate medical care and treatment is essential for managing Atopic Dermatitis. This can include topical creams, oral medications, or light therapy. Working closely with your child’s healthcare provider can help to develop an effective treatment plan.
Resources and Support Groups
There are many resources and support groups available to people with Atopic Dermatitis and their families. These can include online forums, informational websites, and local or national advocacy groups. Connecting with others who understand what you are going through can provide a sense of community and support.
Your doctor or healthcare provider can help connect you with these resources. Don’t be afraid to ask for help or reach out to others who have experience with Atopic Dermatitis.[12][13][14][15]
Preventing Atopic Dermatitis
Atopic Dermatitis, also known as eczema, is a chronic skin condition that affects millions of people worldwide. It is characterized by dry, itchy, and inflamed skin, and can be a source of significant discomfort and distress.
Strategies for At-Risk Individuals
While it is not possible to prevent Atopic Dermatitis entirely, certain strategies can help to reduce the risk of its development. For example, studies have shown that early introduction of solid foods may reduce the risk of eczema in infants. Breastfeeding may also be protective against eczema, as breast milk contains beneficial compounds that can help to strengthen the immune system.
Another important strategy for preventing eczema is to avoid exposure to allergens and irritants. Common triggers of eczema include dust mites, pet dander, pollen, and certain foods. By identifying and avoiding these triggers, individuals with a family history of eczema or other allergic conditions may be able to reduce their risk of developing the condition.
Early Intervention and Management
If you do develop Atopic Dermatitis, early intervention and management can reduce the severity and frequency of symptoms. It is crucial to seek medical attention early if you experience any symptoms, such as itching, redness, or dryness of the skin. Your doctor may recommend a comprehensive treatment plan that includes moisturizers, topical steroids, and other medications to manage your condition effectively.
In addition to medical treatment, there are several lifestyle changes that may help to manage eczema symptoms. For example, taking short, lukewarm baths and using fragrance-free soaps and detergents can help to prevent skin dryness and irritation. Wearing soft, breathable fabrics and avoiding tight-fitting clothing can also help to reduce itching and discomfort.
Research and Future Developments
Research into Atopic Dermatitis and its treatment is ongoing, and new developments are emerging every year. For example, recent studies have suggested that probiotics, or “good” bacteria, may help to reduce the severity of eczema symptoms in some individuals. Other promising areas of research include the development of new topical medications and the use of light therapy to treat eczema.
As our understanding of the condition improves, we may see new and more effective treatments for Atopic Dermatitis in the future. Until then, however, it is important to take steps to prevent and manage eczema symptoms to improve your quality of life and reduce the risk of complications.[16][17][18][19][20][21]
Using the CareClinic App For Your Atopic Dermatitis Treatment Plan
Having an atopic dermatitis action plan is crucial, and the CareClinic app can help with that. You can use![]() the app as your skin disease diary. Just go to the diary section of the app and enter your daily symptoms, medications, and triggers as they occur. There are also specific sections on the app to track each of these. Next time you visit the doctor, this information will be handy in your pocket.
the app as your skin disease diary. Just go to the diary section of the app and enter your daily symptoms, medications, and triggers as they occur. There are also specific sections on the app to track each of these. Next time you visit the doctor, this information will be handy in your pocket.
Whether you develop eczema, psoriatic arthritis, or another skin disorder, our goal is to help with disease control. You can also track your medications and treatments, whether it be topical corticosteroids, emollient treatment, topical moisturizers, topical antihistamines, topical antibiotics, or topical calcineurin inhibitors.
Atopic Dermatitis can be a challenging condition to live with, but with the right management and treatment plan, it is possible to reduce symptoms and improve overall well-being. This guide has provided a comprehensive overview of the condition, including diagnosis, treatment options, and prevention strategies. It is essential to work with your healthcare provider to develop a personalized treatment plan that meets your unique needs and goals.
Sources:
- https://www.mayoclinic.org/diseases-conditions/atopic-dermatitis-eczema/symptoms-causes/syc-20353273
- https://www.aad.org/public/diseases/eczema/types/atopic-dermatitis
- https://nationaleczema.org/eczema/types-of-eczema/atopic-dermatitis/
References
- “Eczema | Johns Hopkins Medicine”. https://www.hopkinsmedicine.org/health/conditions-and-diseases/eczema
- “Atopic Dermatitis (Eczema) – Skin Disorders – Merck Manual Consumer Version”. https://www.merckmanuals.com/home/skin-disorders/itching-and-dermatitis/atopic-dermatitis-eczema
- “Atopic Dermatitis: Diagnosis and Treatment – PubMed”. https://pubmed.ncbi.nlm.nih.gov/32412211/
- “How common is atopic dermatitis? | Global Atopic Dermatitis Atlas”. https://www.atopicdermatitisatlas.org/en/explore-data/atopic-dermatitis/how-common-is-atopic-dermatitis
- “Atopic Dermatitis Treatment, Symptoms & Causes | NIAMS”. https://www.niams.nih.gov/health-topics/atopic-dermatitis
- “Atopic Dermatitis: Diagnosis and Treatment | AAFP”. https://www.aafp.org/pubs/afp/issues/2020/0515/p590.html
- “S2k guideline on diagnosis and treatment of atopic dermatitis — short version – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC4861742/
- “Advances in Skin & Wound Care”. https://journals.lww.com/aswcjournal/fulltext/2018/12000/diagnosis_and_management_of_atopic_dermatitis__a.3.aspx
- “Diagnosis and Management of Atopic Dermatitis for Primary Care Providers | American Board of Family Medicine”. https://www.jabfm.org/content/33/4/626
- “Management of Atopic Dermatitis: Guideline from the American Academy of Dermatology | AAFP”. https://www.aafp.org/pubs/afp/issues/2014/1201/p798.html
- “American Academy of Dermatology issues updated guidelines for the management of atopic dermatitis in adults with topical therapies”. https://www.aad.org/news/updated-atopic-dermatitis-guidelines-topical-therapies
- “Asthma and Allergy Foundation of America”. https://en.wikipedia.org/wiki/Asthma_and_Allergy_Foundation_of_America
- “Understanding Eczema in Children: Tips to Manage Flare-ups and Improve Comfort – Care& Family Health”. https://careand.ca/post/eczema-in-children-tips-manage-flare-ups-improve-comfort/
- “Atopic dermatitis: Self-care”. https://www.aad.org/public/diseases/eczema/types/atopic-dermatitis/self-care
- “Helping Your Child Cope With Eczema | Atopic Dermatitis and Kids”. https://nationaleczema.org/blog/helping-child-cope-eczema/
- “Early exposure to solid foods and the development of eczema in children up to 4 years of age”. https://pubmed.ncbi.nlm.nih.gov/19573205/
- “Association between the age of solid food introduction and eczema: A systematic review and a meta-analysis – PubMed”. https://pubmed.ncbi.nlm.nih.gov/29570230/
- “Timing of introduction to solid food, eczema and wheezing in later childhood: a longitudinal cohort study – PMC”. https://pmc.ncbi.nlm.nih.gov/articles/PMC10577938/
- “Timing of introduction of solid food and risk of allergic disease development: Understanding the evidence | Allergologia et Immunopathologia”. https://www.elsevier.es/en-revista-allergologia-et-immunopathologia-105-articulo-timing-introduction-solid-food-risk-S0301054612002960
- “Atopic dermatitis”. https://en.wikipedia.org/wiki/Atopic_dermatitis
- “Probiotics for the treatment of eczema: a systematic review – PubMed”. https://pubmed.ncbi.nlm.nih.gov/19573037/