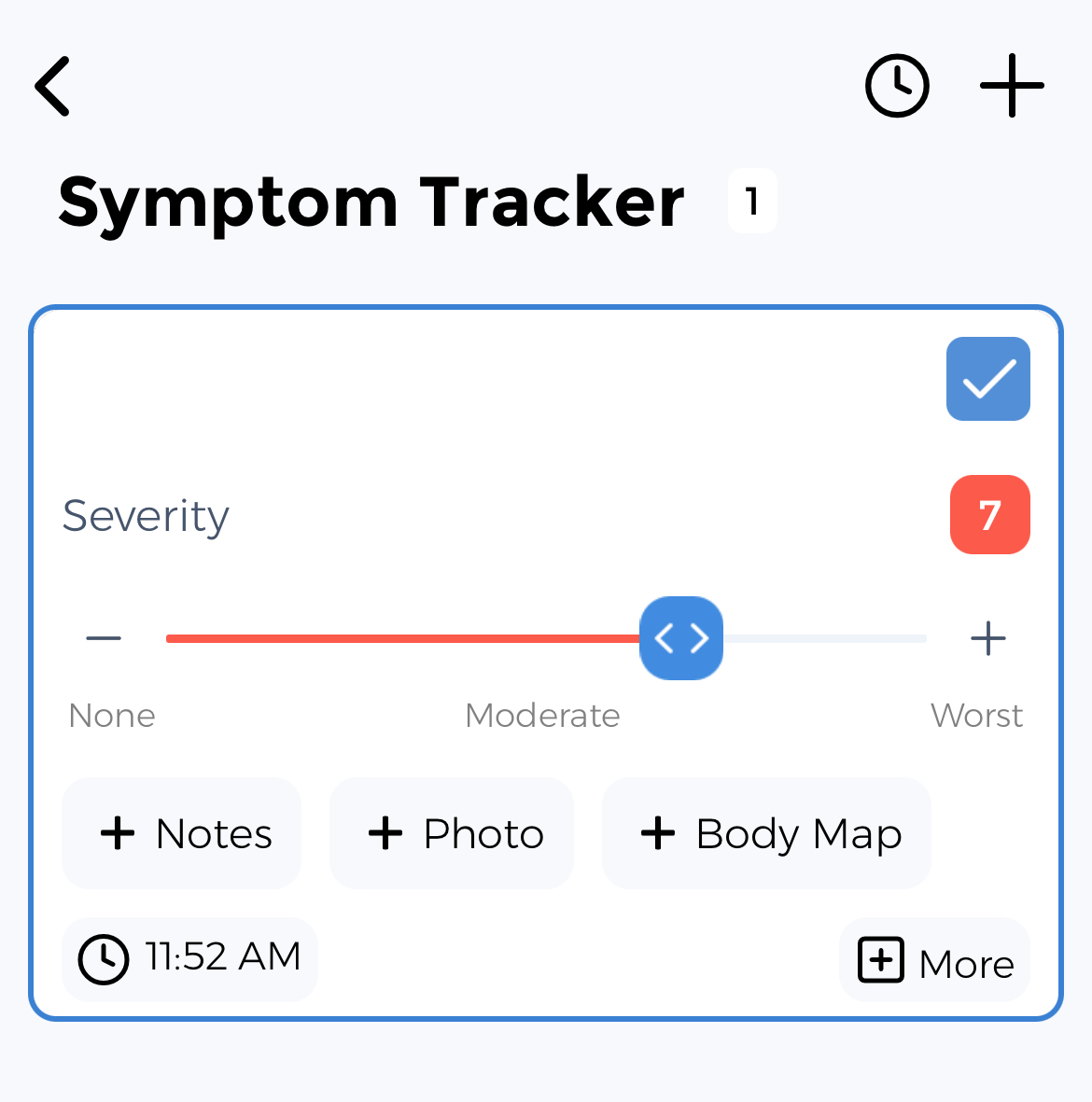
Functional Dyspepsia Symptom Tracker: Your Health Assistant
Living with Functional Dyspepsia means dealing with upper abdominal pain, early satiety, fullness after eating, and more. But here's the truth: Data is your most powerful tool. Every logged symptom reveals patterns—so you can take informed action.
Functional dyspepsia is a chronic disorder of sensation and movement in the upper digestive tract causing persistent indigestion without identifiable structural cause. It includes postprandial distress syndrome and epigastric pain syndrome subtypes. Tracking symptoms, food triggers, and treatment responses helps manage this common but challenging condition.
Key Functional Dyspepsia Symptoms You Should Track
Struggling with symptoms like these? Tracking them reveals patterns, triggers, and how they impact your daily life.
Upper abdominal pain
Early satiety
Fullness after eating
Bloating
Belching
Nausea
Burning sensation
Food intolerance
Weight loss
Appetite changes
Abdominal distension
Vomiting
Track Your Functional Dyspepsia Treatments
Tracking how these common treatments affect your symptoms can help you and your healthcare provider optimize your care plan:
Our tracker helps you monitor when you take medications and how they affect your symptoms over time.
Standardized Functional Dyspepsia Assessments
Complete these evidence-based assessments in the App to measure your severity and monitor your progress:
⚡ Knowledge Is Your Superpower
The difference between feeling overwhelmed by Functional Dyspepsia and feeling in control starts with data. When you track your symptoms, you transform uncertainty into clarity. Every data point brings you closer to understanding your unique patterns.
It's free to try for anyone—whether you're managing your own condition, supporting a child, helping an aging parent, or assisting a partner. Our tracker adapts to your specific role in the health journey.
How the CareClinic Functional Dyspepsia Symptom Tracker Adapts to Your Needs
Adults
Caregivers
Parents of Children
Young Adults
Your Complete Functional Dyspepsia Management Toolkit
Uncover Patterns & Insights
Map your Functional Dyspepsia symptoms like a detective solving a case.
Understand Your Medication's Impact
Turn guesswork into strategy. See how treatments affect your well-being with clear health insights.
Objectively Measure Your Progress
Use clinically validated tools to objectively measure your progress.
Other Tools You May Like...
Plus 6 more specialized tracking tools available
Access All Tracking ToolsAlso Supports Other Conditions Like
Irritable Bowel Syndrome Tracker
Irritable Bowel Syndrome warriors use our tracker to monitor abdominal pain, bloating.
GERD Tracker
GERD warriors use our tracker to monitor heartburn, regurgitation.
Generalized Anxiety Disorder Tracker
Generalized Anxiety Disorder warriors use our tracker to monitor excessive worry, restlessness.
Major Depressive Disorder Tracker
Major Depressive Disorder warriors use our tracker to monitor persistent sadness, loss of interest.
Success Stories from Our Community
"The tracker's reminders helped me stay consistent with monitoring my {symptom}, which led to discovering that I realized that stress affected my upper abdominal pain more than I'd thought possible."
"Using the various trackers together gave me a complete picture of my Functional Dyspepsia. The meal size tracker helped me see exactly how bloating changed throughout the day, while the medication tracker showed me how to improve my daily management."
Take Control of Your Functional Dyspepsia Journey
Transform from feeling like a passive patient to becoming an informed self-advocate. Join thousands who've discovered new insights about their condition.
Designed by people who understand the daily challenges of managing chronic conditions, we're here to support you and your ❤️ ones.
Download Your Functional Dyspepsia Tracker NowYour Data is Protected
Private & Secure
HIPAA Compliant
GDPR Compliant
Never Sell Data
Your data is yours: You get full control over who can view your information. CareClinic keeps all your data secure and encrypted.
References based on studies by: